What is Hyperaldosteronism?
Aldosterone is a hormone that helps your body hold onto salt (sodium) and water which raises your blood pressure. It also makes your body get rid of potassium, which can cause low potassium levels (hypokalemia) in your blood. This hormone is produced by the zona glomerulosa, which is the outermost layer of your adrenal gland.
Producing too much aldosterone is a condition called hyperaldosteronism. This condition is often first noticed as high blood pressure, which can be from mild to severe and hard to manage with treatment. Hyperaldosteronism itself often goes undetected.
Hyperaldosteronism can be primary or secondary. Both types show similar symptoms, but tests are used to tell them apart. Primary hyperaldosteronism usually causes low levels of renin (a protein that controls blood pressure) and high aldosterone levels. This is because of a problem with the adrenal gland which makes too much aldosterone on its own. Secondary hyperaldosteronism is caused by too much renin being produced due to various reasons such as kidney problems, heart issues, liver failure resulting in fluid buildup in the abdomen (ascites), lung-related heart disease (cor pulmonale), being pregnant, certain types of tumor, eating too much licorice, specific genetic conditions, and kidney failure.
The diagnosis made initially for high levels of aldosterone (hyperaldosteronism) includes checking renin levels, aldosterone levels, and the ratio between aldosterone and renin. It often takes a long time to get a correct diagnosis for hyperaldosteronism, with more than a third of patients waiting over 5 years for a correct diagnosis, especially women.
It is recommended that people newly diagnosed with high blood pressure, especially those who don’t respond to common high blood pressure medications, get checked for hyperaldosteronism (high aldosterone levels or an aldosterone-to-renin ratio >20:1). Understanding the diagnosis and difference between types of hyperaldosteronism is critical to decide the right treatment. Surgery may be needed for primary hyperaldosteronism affecting only one adrenal gland, whereas medical treatment is usually used for disease affecting both adrenal glands and secondary hyperaldosteronism.
What Causes Hyperaldosteronism?
Hyperaldosteronism is a condition where your body produces too much aldosterone, a hormone that helps balance sodium and potassium levels in your blood. The reason behind this overproduction separates primary from secondary hyperaldosteronism. Usually, if you have high aldosterone but low renin (another hormone) levels, that hints at primary hyperaldosteronism. If your renin level is high as well, that indicates secondary hyperaldosteronism.
Primary Hyperaldosteronism
Primary hyperaldosteronism, also known as Conn syndrome, is caused by overproduction of aldosterone by the adrenal glands. The adrenal gland is an organ that sits just above your kidney. In a majority of patients (around 90% to be precise), the cause is usually a tumor in one adrenal gland. Sometimes, both adrenal glands can grow excessively large, but this is less common.
Some rare forms of primary hyperaldosteronism include excessive growth of one adrenal gland, aldosterone-secreting tumors generally located in the kidneys or ovaries, serious adrenal cancers that produce aldosterone, and a condition called familial hyperaldosteronism, which runs in families. It’s worth noting that newer data shows that the rate of dual adrenal gland overgrowth might account for 75% of all primary hyperaldosteronism cases.
In some extremely rare cases, primary hyperaldosteronism is caused by genetic abnormalities, such as Familial hyperaldosteronism type I, II, and III. Type I is a condition where the body produces excessive aldosterone because of a mixed-up gene. This variant is unique because it can be controlled with a specific type of medicine called glucocorticoids. Variants II and III are caused by other genetic abnormalities, and these conditions cannot be controlled with glucocorticoids.
Secondary Hyperaldosteronism
Secondary hyperaldosteronism is caused by issues in the renin-angiotensin-aldosterone system (RAAS), a complicated hormone system that helps regulate your body’s Blood Pressure and fluid balance. This overproduction could be due to a renin-producing tumor, potassium levels that are too high because of chronic kidney disease, or the narrowing of the arteries leading to the kidneys. There are also various conditions that can result in this type of hyperaldosteronism, like heart failure, pregnancy, liver cirrhosis with water accumulation in the abdomen, sleep apnea, or certain syndromes like Bartter or Gitelman.
In certain situations like heart failure, the amount of aldosterone your body produces might be normal, but the liver might lack the sufficient blood flow to get rid of the hormone. So, the hormone’s levels might appear elevated in the blood. People with secondary hyperaldosteronism typically have higher blood pressures and higher aldosterone levels than those with primary disease.
Risk Factors and Frequency for Hyperaldosteronism
Primary hyperaldosteronism is a condition that affects at least 10% of people with high blood pressure. The likelihood of having this condition increases if the high blood pressure is severe. In fact, it’s seen in over 20% of patients with resistant high blood pressure, especially in those below the age of 40 or those who have low levels of potassium in their blood. Previously, this condition was largely undetected due to variations in how patients were selected, methods of diagnosis, definitions of high blood pressure, and the lack of testing in patients who met the screening criteria.
In comparison, the diagnosis of secondary hyperaldosteronism is less common than primary hyperaldosteronism. Both conditions are seen more frequently in women. Additionally, African and Black American populations have a higher occurrence of hyperaldosteronism than the general population, particularly a form of the condition known as idiopathic bilateral adrenal hyperplasia.
Signs and Symptoms of Hyperaldosteronism
Hyperaldosteronism’s symptoms differ from person to person and can sometimes be without noticeable effects. The most common symptom is resistant hypertension, especially when paired with low potassium levels in your blood (hypokalemia). This problem is often seen in young women who aren’t responding to three or more high blood pressure medications. Other signs of this condition include fatigue, headaches, weakness, belly bloating, intestinal blockage, frequent and excessive urination, excessive thirst, and a form of diabetes caused by kidney malfunction (nephrogenic diabetes insipidus) due to hypokalemia.
Blood pressure in people with hyperaldosteronism can vary from normal to severe high blood pressure. This hypertension is often resistant to standard treatments. The reason for the high blood pressure is mainly due to excess re-absorption of sodium, an increase in blood volume, and increased resistance in the blood vessels. More symptoms can appear due to moderate to severe high blood pressure or from hypokalemia. High blood pressure could cause headaches, dizziness, vision problems, chest pain, and shortness of breath. Hypokalemia can cause muscle weakness, fatigue, heart palpitations, cramps, excessive thirst, and frequent urination due to nephrogenic diabetes insipidus.
Secondary hyperaldosteronism patients might have varying levels of blood pressure, but most will have some form of high blood pressure. Some conditions like renal artery stenosis and coarctation of the aorta can also contribute to high blood pressure. Patients using diuretics or those suffering from heart failure, cirrhosis, or nephrotic syndrome can experience hypovolemia (decreased volume of blood plasma). Still, no specific physical signs can confirm hyperaldosteronism. However, long-term high blood pressure can lead to left ventricular hypertrophy, causing an abnormal heart sound.
The risk of hyperaldosteronism can increase due to several factors. These include:
- A family history of high blood pressure or heart diseases.
- Diagnosis of high blood pressure before the age of 40.
- Lower than normal levels of potassium in your blood.
- Unexpected discovery of a tumor on an adrenal gland in someone with high blood pressure that is hard to manage.
- Resistant hypertension, which doesn’t improve despite the use of three or more standard high blood pressure medicines, including a diuretic.
Testing for Hyperaldosteronism
Regular screening for hyperaldosteronism (a condition where your adrenal glands produce too much of the hormone aldosterone) is recommended in certain individuals who have recently been diagnosed with high blood pressure. Special attention is given to those with early-onset high blood pressure, low potassium levels, persistent or tough-to-manage high blood pressure, sleep apnea, or an adrenal mass. Since many cases of hyperaldosteronism go undetected, routine screening can be crucial.
Unfortunately, screening for hyperaldosteronism isn’t performed as frequently as it should be, leading to frequent misdiagnoses. This can be caused by several factors including a general lack of awareness of the condition, complexity of confirmatory tests, lack of standardized screening protocols, and varied symptoms.
Screening for hyperaldosteronism usually involves a straightforward blood test checking levels of a hormone called renin and aldosterone. If these hormones are at certain levels, it could suggest hyperaldosteronism. Depending on your results, further testing might be performed.
When it comes to lab results, the ratio of aldosterone to renin in your blood can indicate hyperaldosteronism. However, this test can vary depending on certain factors such as your position while taking the test, time of the day, and certain medications you are taking among other factors.
It’s worth noting, low potassium levels used to be a classic symptom of hyperaldosteronism, but it’s now recognized as a relatively rare occurrence. So, even if your potassium levels are normal, you can still have hyperaldosteronism.
The diagnosis path for primary hyperaldosteronism, a more common form of the condition, often involves checking the activity of the hormone renin in your blood. If you have lower levels of renin combined with high aldosterone levels, that could indicate primary hyperaldosteronism.
The process is different in diagnosing secondary hyperaldosteronism, which is caused by factors not related to your adrenal glands. In this case, both your renin concentration and activity levels would be elevated compared to primary hyperaldosteronism.
Once you’ve been diagnosed with primary hyperaldosteronism, the emphasis shifts to determining whether the cause is from one adrenal gland (unilateral) or both (bilateral), as this impacts the treatment approach.
The process for confirming a diagnosis of hyperaldosteronism can vary and might not always be necessary. However, this usually includes measuring the aldosterone levels in your blood, collecting a 24-hour urine sample for aldosterone excretion levels or conducting a suppression test where certain medications are given that are expected to lower aldosterone levels.
Differentiating between primary and secondary hyperaldosteronism can be done by checking renin levels, as primary hyperaldosteronism suppresses renin production.
Diagnostic imaging, such as a CT scan, can come in handy when determining the cause of primary hyperaldosteronism. However, it’s important to bear in mind, this tool comes with some limitations and can’t always reliably distinguish between slightly different conditions.
In some cases, you might need to undergo a procedure known as adrenal vein sampling. This helps distinguish between a unilateral or bilateral adrenal issue. This is a complex process and can be challenging to interpret.
Validating hyperaldosteronism might even require genetic testing, especially for young patients or those with a family history of the disorder.
To sum up, the evaluation for hyperaldosteronism is a multi-step process that starts with differentiating between primary and secondary forms of the condition. The presence of this condition often requires further testing, as the source seldom stops at the initial diagnosis. This helps to differentiate between unilateral disease, which is treated surgically, and bilateral disease, which is managed with medical therapy.
Treatment Options for Hyperaldosteronism
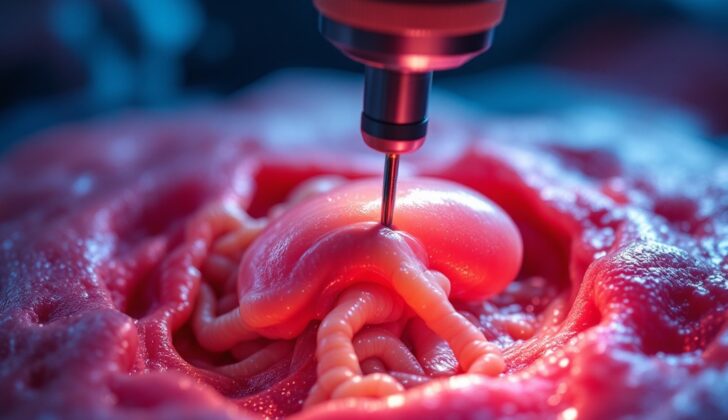
If you have primary hyperaldosteronism, a condition caused by a problem in one of your adrenal glands, your doctor will likely recommend surgery as the best treatment plan. Modern techniques such as robotic or laparoscopic surgery are typically favored, as they tend to result in fewer complications and shorter hospital stays than traditional open surgery. Removal of the entire adrenal gland is usually preferred because it’s more effective at relieving symptoms.
Before the operation, you may be given a medication called spironolactone to help control your blood pressure for about 4-6 weeks. Even after the surgery, you might continue to have high blood pressure. However, about two-thirds of patients can eventually achieve stable, normal blood pressure after a year or so.
People who get surgery usually do better in the long term than those who just receive medication. They tend to have better control of their blood pressure and maintain healthier levels of potassium in their bodies. However, if your blood pressure remains high after surgery, you might need to consider other potential causes or issues like another health condition, or damage from chronic hyperaldosteronism.
If you’re not a good candidate for surgery, your doctor might recommend medications such as spironolactone or eplerenone. There is also a less invasive treatment option called adrenal ablation that can be considered for some patients. This procedure involves a catheter and can successfully treat about 75% of patients.
If you have primary hyperaldosteronism caused by problems in both adrenal glands, or bilateral hyperplasia, medication is often the treatment of choice. Spironolactone or eplerenone are typically used. Amiloride, a type of medication that helps your body keep potassium while getting rid of sodium, might also be used.
Combination therapy, which includes medications, lifestyle changes like reducing salt intake, avoiding alcohol, quitting smoking, regular exercise, and maintaining a healthy weight is usually the most effective treatment plan. In some cases, additional medications or even surgery may be recommended.
If you have secondary hyperaldosteronism, the best treatment is to manage the underlying disease that is causing the symptom. This could include ACE inhibitors or angiotensin receptor blockers to control blood pressure, reducing your salt intake, and possibly taking potassium supplements or medications to help manage the condition.
What else can Hyperaldosteronism be?
There are many conditions that can seem similar to hyperaldosteronism. Some of these include essential hypertension, Liddle syndrome, syndrome of apparent mineralocorticoid excess, congenital adrenal hyperplasia, primary glucocorticoid resistance, Cushing syndrome (hypercortisolism), aldosterone-producing renin-responsive adenomas, diabetes insipidus, and excessive licorice intake. There are also conditions that share some similar symptoms:
- 17-Alpha-hydroxylase deficiency may closely mimic hyperaldosteronism. Patients usually present with underdeveloped sexual organs, and gene testing may be needed to conclusively diagnose this condition.
- Chrétien syndrome is a rare disorder caused by excessive secretion of a hormone from a pituitary tumor, leading to what is often termed adrenocortical hypertension.
- Congenital adrenal hyperplasia is usually associated with a family history of hormone deficiencies and presents itself with low aldosterone levels.
- Ectopic ACTH syndrome is characterized by high levels of a hormone that can’t be reduced with high-dose medications, and these patients often have an underlying tumor.
- Essential hypertension usually presents with a normal PAC/PRA ratio.
- Excessive licorice intake can inhibit the kidney’s conversion of one hormone to another, leading to a hormone excess, which behaves like hyperaldosteronism.
- Liddle syndrome, a rare genetic disorder, presents with low aldosterone levels and usually first shows symptoms in childhood. It’s often referred to as pseudohyperaldosteronism due to symptoms that seem like a mineralocorticoid excess disorder.
- Primary glucocorticoid resistance presents as low aldosterone levels, elevated ACTH and cortisol, and frequently features a family history of the syndrome.
- Syndrome of apparent mineralocorticoid excess features high blood pressure, low aldosterone levels, high levels of a hormone in the urine, and a hereditary disposition. It can also be related to excessive licorice consumption.
Hyperaldosteronism and hypercortisolism, also known as Cushing syndrome, share similar symptoms due to their connection with abnormal adrenal gland function. Both conditions are three times more common in women than men and are usually diagnosed in patients between 25 and 50. They most often present with high blood pressure, low potassium, and high sodium levels.
In hyperaldosteronism, patients usually have very high blood pressure that doesn’t respond well to typical treatments. Hypercortisolism is less common, and those with the condition often have less severe hypertension. Hypercortisolism can be suspected based on symptoms like weight gain, muscle weakness, thin arms and legs, a round face, a fat pad at the base of the neck, easy bruising, thin skin, acne, excessive hairiness, and purple stretch marks.
What to expect with Hyperaldosteronism
Hyperaldosteronism is a condition that, when treated, has survival rates ranging from 90% to 95% over a 10-year period, according to some studies. The most common health issue connected with hyperaldosteronism relates to the heart. However, the overall death rates for those with this condition does not significantly deviate from that of the general public.
If a related condition called hypokalemia continues, it could lead to symptoms like weakness, paralysis, constipation, and producing too much urine. Primarily, hyperaldosteronism and hypokalemia can negatively impact insulin secretion, raising the chances of developing diabetes.
About two-thirds of patients tend to have normal blood pressure levels after undergoing surgery on the adrenal gland. However, the time for improvement could last up to a year. By the end of 5 years after surgery, about half of the patients maintain normal blood pressure without needing medication.
If hyperaldosteronism is not treated, it can lead to serious health issues and death primarily caused by uncontrolled high blood pressure and irregular heart rhythms.
Possible Complications When Diagnosed with Hyperaldosteronism
Hyperaldosteronism, a condition involving too much aldosterone hormone, often leads to serious heart-related complications. This condition is associated with an increased risk of dying from heart-related problems. The symptoms brought about by hyperaldosteronism can range widely. They include irregular heartbeat, enlargement of the left side of the heart, high blood pressure, heart attack, and stroke. In addition, if hyperaldosteronism persists over a long period, it can cause fibrosis, which is a condition where heart tissues thicken and scar.
Common Complications:
- Increase in heart-related mortality
- Irregular heartbeat (atrial fibrillation)
- Enlargement of the left side of the heart (left ventricular hypertrophy)
- High blood pressure (hypertension)
- Heart Attack (myocardial infarction)
- Stroke
- Fibrosis (scarring) of heart tissues in long-term cases
Recovery from Hyperaldosteronism
Cutting down on salt intake to less than 100 milliequivalents per day, stopping alcohol and tobacco use, maintaining a healthy body weight, and doing regular aerobic exercise can all help improve recovery after surgery and contribute to overall health.
Preventing Hyperaldosteronism
Doctors should explain to patients about their health situation in a clear and easy to understand manner. They will also stress why it’s significant to stick with the treatment plan over the long term. This plan could include changes to what they eat, like limiting the amount of salt they consume. It’s also really crucial that patients take any prescribed medications exactly as directed by their doctor.