What is Hypopituitarism?
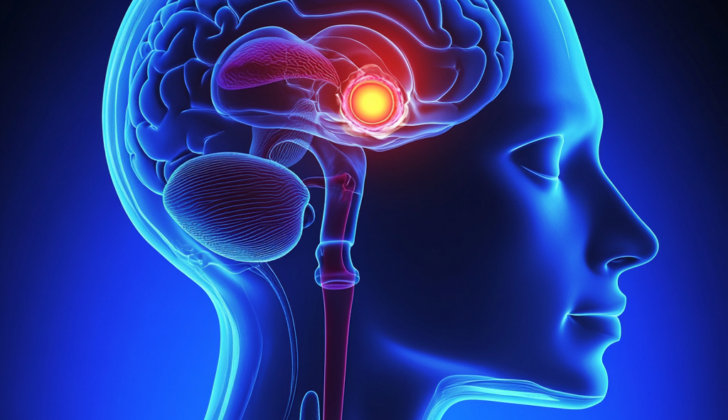
The pituitary gland has a crucial role in creating and releasing different hormones that assist in managing the body’s hormonal functions. This gland is structurally divided into two primary parts— the front (anterior) and the back (posterior).
The front part of the pituitary gland has the job of making and releasing several key hormones. These include the growth hormone (GH, which helps the body to grow properly), the thyroid-stimulating hormone (TSH, which controls the thyroid gland), the luteinizing hormone (LH, which regulates reproductive organs), the follicular-stimulating hormone (FSH, another hormone that controls reproductive organs), the adrenocorticotropin hormone (ACTH, which helps manage stress), and prolactin (PRL, which controls milk production).
The back part of the pituitary gland is in charge of storing and releasing two important hormones, including oxytocin (which plays a role in childbirth and breastfeeding) and antidiuretic hormone (ADH, also known as vasopressin, which helps the kidneys manage the amount of water in your body). These hormones are made by special cells in the brain called neurosecretory cells, located in an area known as the hypothalamus.
The activity of the pituitary gland is tightly controlled and involves a complex interaction between the hypothalamus and the front part of the pituitary gland. The hypothalamus makes and releases hormones, often referred to as tropic hormones, which directly influence the release of certain hormones from the front part of the pituitary gland. This interaction significantly affects different target organs and their respective functions.
A medical condition known as hypopituitarism occurs when the pituitary gland doesn’t produce enough of one or more hormones. This condition can increase the risk of death from cardiovascular and respiratory diseases. Because the symptoms of hypopituitarism can be subtle, it’s important to discover and manage the condition early to prevent additional health problems.
What Causes Hypopituitarism?
Hypopituitarism, or underactive pituitary gland, can occur from two main causes. First, issues with another part of your brain, the hypothalamus, which controls the pituitary gland’s function, and second, directly from problems within the pituitary gland itself. Tumors in the pituitary gland are a common cause, making up 61% of cases.
These tumors can produce an excess of one hormone, causing other hormones to be in short supply. For example, in a condition called acromegaly, there’s an overproduction of growth hormone, often causing other pituitary hormones to be in deficit due to a large tumor (macroadenoma).
While most pituitary tumors are benign (not cancerous), on rare occasions, cancers like breast, colon, and prostate cancers can spread to the pituitary gland. Other non-cancerous types of tumors, such as suprasellar meningiomas, gliomas, and craniopharyngiomas, can also cause hypopituitarism. Besides tumors, injuries to the pituitary gland, such as traumatic brain injuries, surgical injuries, or exposure to radiation can also lead to hypopituitarism.
Certain infectious diseases like tuberculosis, viruses, and other infections not related to tuberculosis, such as histoplasmosis and syphilis, can also lead to an underactive pituitary gland. Immune system disorders can also affect the pituitary, such as lymphocytic hypophysitis, which is an inflammation often seen after childbirth. This disorder responds well to steroid therapy.
New immune therapies involving what are called immune checkpoint inhibitors can also cause inflammation of the pituitary gland, a condition known as hypophysitis. This condition is characterized by a shortage of hormones produced by the adrenal glands. In rare cases, it can also lead to an underactive thyroid gland (hypothyroidism) or sex hormone imbalances (hypogonadism). These hormonal issues can often persist, leading to permanent changes even after stopping these medications.
Other diseases such as hemochromatosis, sarcoidosis, and histiocytosis can also lead to hypopituitarism by damaging the pituitary gland due to the abnormal buildup of substances or immune processes.
Traumatic brain injury can also cause hypopituitarism, which is now more widely recognized. It can cause a range of issues with the pituitary gland. While proper and timely diagnosis can be helpful, it is not always straightforward due to general symptoms overlapping effects of the injury.
Pituitary apoplexy is a medical emergency caused by a stroke or bleeding within the pituitary gland. This is often, but not always, associated with a tumor in the pituitary gland. Sheehan syndrome, another condition, arises from damage to the pituitary gland due to significant blood loss after childbirth.
Sometimes, the pituitary gland may be absent from birth, which is linked to facial abnormalities. Mutations in certain genes can cause this condition.
Empty Sella syndrome is a rare disorder where the pituitary gland becomes smaller or disappears, due to the enlargement or irregular form of a bony structure in the skull, the sella turcica. This syndrome can be due to several causes, such as treated pituitary tumors, head trauma, or a condition known as pseudotumor cerebri (also known as idiopathic intracranial hypertension), which raises pressure within the skull.
Lastly, Kallmann syndrome is a rare genetic condition causing a reduced or absent sense of smell and decreased production of sex hormones. This syndrome is often caused by a mutation in the Kal1 gene, especially in males.
Risk Factors and Frequency for Hypopituitarism
Hypopituitarism is considered as a rare disorder according to the National Institute of Health (NIH). There’s not much data available about how frequently it occurs. However, according to a study done in Northwestern Spain, it is found in 45.5 out of every 100,000 people.
Signs and Symptoms of Hypopituitarism
Hypopituitarism, a condition that occurs when about 75% of the pituitary gland is affected, can present subtly with mild symptoms or severely with a sudden onset of symptoms. It can occur due to various factors, such as Sheehan syndrome, pituitary apoplexy, pituitary infection, hypophysitis, and traumatic brain injury. This condition’s symptoms are often due to deficiencies in pituitary hormones, consequences of pituitary tumors, or characteristics of the underlying disease causing the condition.
- ACTH deficiency: Leads to adrenal insufficiency.
- TSH deficiency: Causes hypothyroidism.
- Gonadotropin deficiency: Results in hypogonadism.
- GH deficiency: Can lead to poor growth and short stature in children and fatigue and weakness in adults.
- ADH deficiency: Results in diabetes insipidus, causing excessive thirst and urination.
Visual impairments such as bitemporal hemianopsia are a common result of pituitary tumor mass effects, followed by unilateral defects. These visual disturbances can be accompanied by headaches. The physical examination might not show significant findings, due to the typically subtle presentation of hypopituitarism. However, there could be variable features present depending upon which hormones are involved, leading to conditions such as:
- Hypothyroidism: Symptoms might include a small and soft thyroid gland, dry and coarse skin, thinning hair and hair loss, delayed tendon reflexes, cold skin with reduced sweating, and non-pitting type edema.
- Adrenal insufficiency: Common symptoms include fatigue and low blood pressure when standing.
- Hypogonadism: In men, this can show as small and shrunken testes, while in women, it can result in the loss of underarm and pubic hair.
- Neurological and eye involvement: This can lead to a loss of visual sharpness, weakness in muscles that move the eyes, and bitemporal hemianopsia.
- Diabetes insipidus: Symptoms include increased salt in the blood, excessive urination, and diluted urine.
Testing for Hypopituitarism
Having a pituitary tumor can lead to it producing too much of a certain hormone which could cause symptoms tied to having high levels of that hormone. At the same time, other pituitary hormones might not be produced enough.
To find out what’s going on, doctors need to carry out certain tests.
Blood tests are often done first to look at the levels of hormones that the pituitary gland and other glands it controls produce. But these tests aren’t always helpful because many things can influence hormone levels, including the time of day, the season, and natural fluctuations in hormone release. So, if these levels are not revealing, doctors can perform dynamic function tests.
In a dynamic function test, a substance that usually prompts the release of the hormone being checked is given to you. The levels of this hormone in your blood are measured before and after this is done to see if your body is responding normally.
One of these tests is called the insulin tolerance test (ITT), and is known to be very reliable. In this test, you are first put on a fast overnight, then given an insulin dose that is calculated based on your body weight. This insulin dose should drop your blood sugar levels. Your hormone and blood sugar levels are then measured at specific times. After the test, you are given dextrose through an IV to bring your blood sugar levels back to normal, and you are monitored for an hour and a half afterward. Healthy results are when your cortisol levels go above 20 micrograms per deciliter and growth hormone levels are between 5 and 10 nanograms per milliliter. However, this test is not recommended for individuals with heart conditions or epilepsy because of its potential risks.
Another test called the ACTH stimulation test could be used if an ITT test is considered too risky due to the potential for severely low blood sugar. This test assesses how well the hypothalamus-pituitary-adrenal gland system is working. Instead of insulin, synthetic ACTH is injected into the patient. Cortisol levels are then measured before and after the ACTH is given. A normal response is indicated when cortisol levels go above 18 micrograms per deciliter.
There’s another kind of test, known as the combined test, in which several hormones related to pituitary output are stimulated at once, and hormone levels monitored. However, this test is not commonly required and thus not commonly used.
Imaging tests are also used to get a good look at the pituitary gland. The main choice for this is an MRI scan with a substance known as gadolinium that helps enhance the pictures. This helps doctors to spot any tumors. If there’s reason to think that a tumor in the pituitary gland is causing a condition known as hypopituitarism, then an examination of visual field defects may be needed. This is because large tumors can put pressure on the optic nerve which affects vision.
Treatment Options for Hypopituitarism
Treating hypopituitarism, a condition where the pituitary gland doesn’t produce enough of certain hormones, involves addressing the underlying cause of the condition. In some cases, surgery may be necessary to remove a mass affecting the gland. Furthermore, patients often need hormone replacement therapy to balance their hormone levels and reduce symptoms related to the condition.
If there is a lack of ACTH, a hormone that stimulates the adrenal glands to release corticosteroids, corticosteroid replacement is needed. Corticosteroids are a type of hormone that manages your body’s use of nutrients and helps your body respond to stress. Starting this hormonal replacement before thyroid hormone replacement can help avoid a serious condition called adrenal crisis, where the body can’t respond to stress properly. Hydrocortisone is usually used for this. It’s also important to avoid administering this medication at night, as it could cause insomnia. Some patients may require increased dosages during stressful times, surgery, or pregnancy.
If there is a lack of TSH, a hormone that stimulates the thyroid gland to release thyroid hormones, thyroid hormone replacement therapy is necessary. This therapy involves taking a synthetic thyroid hormone known as L-thyroxine. This is especially important for individuals who are older or have a heart disease. As TSH isn’t a reliable marker for these patients, they should regularly test their thyroxine levels, another type of thyroid hormone, to ensure effective treatment.
If there is a lack of FSH and LH, hormones that regulate the reproductive systems, men and women may require different types of hormone replacements. For men, testosterone replacement can be given. The prostate-specific antigen and hemoglobin levels need to be monitored frequently in these patients. For women, estrogen and progesterone hormone replacement can be given. Hormone levels across all axes (different hormonal systems) should be closely monitored, especially when a woman is seeking to get pregnant. Men who are looking to improve their fertility can use human chorionic gonadotropin (HCG) which can help enhance testosterone levels and improve semen quality.
For those with a GH deficit, a condition where the body doesn’t produce enough growth hormones, treatment can vary based on age. Children are often given synthetic growth hormone treatments, but the role of this therapy in adults is still uncertain. For these children, the goal of treatment is to ensure they reach their full height potential. Doctors will reassess after puberty to see if the therapy should continue.
For those with an ADH deficit, a situation where the body doesn’t make enough anti-diuretic hormone (ADH) which helps the kidneys manage the amount of water in your body, synthetic ADH can be used. This hormone helps to maintain the body’s water balance and control excessive urination. Keeping sodium levels in the normal range and monitoring urine-specific gravity (a measure of urine concentration) and osmolality (a measure of solute concentration in urine) helps evaluate the effectiveness of ADH replacement therapy.
What else can Hypopituitarism be?
When dealing with complicated medical cases, recognizing hypopituitarism can be difficult, particularly when hormone levels appear normal but the target organs are not responding as they should. Regardless, if adrenal insufficiency is suspected, it’s important to start treatment right away, even before concrete biochemical proof is found.
When a doctor is trying to figure out if a patient has hypopituitarism, they may also consider these possible conditions:
- Primary hypothyroidism
- Kallmann syndrome
- Pituitary macroadenomas (large growths on the pituitary gland)
- Hyponatremia (low sodium levels)
- Autoimmune polyglandular syndrome types 1, 2, and 3 (conditions where the immune system attacks the body’s own glands)
What to expect with Hypopituitarism
Patients who are stable and can stick to hormone replacement therapy typically have a good outcome. However, the death rates can increase for those who suddenly become very ill. The level of illness can vary and depends on the type of hormone that is deficient.
Hypopituitarism, a condition where the pituitary gland does not produce enough hormones, can have different effects on the body depending on how much the gland is affected. Certain health conditions that come from a sudden drop in the hormones produced by the pituitary gland may increase the risk of death. For example, a lack of the hormone ACTH can lead to an adrenal crisis, while a lack of the hormone TSH may result in a condition called myxedema coma, both of which could potentially lead to death.
Possible Complications When Diagnosed with Hypopituitarism
Hypopituitarism, or deficiency in pituitary gland hormones can lead to other health issues. For example, deficiency in human growth hormone (HGH), can lead to weight gain (obesity), raised cholesterol levels, and metabolic disorder. On the other hand, an absence of a hormone called estradiol, can increase the risk of developing osteoporosis.
Conditions Linked to Hormonal Deficiencies:
- Obesity
- Raised cholesterol levels
- Metabolic disorder
- Osteoporosis
Preventing Hypopituitarism
It is crucial for patients with certain conditions to understand that they will need to rely on hormone replacement therapy for the rest of their lives. Life’s stressful situations might mean an increase in the dosage of this therapy. Whenever they feel it’s warranted, they shouldn’t hesitate to seek immediate medical help. Keeping a steady check on their condition can help avoid getting too much or too little of the hormone replacement.
They should also always have some form of ID on them, like a medical alert bracelet or necklace. This ID should clearly state their medical condition so that if an emergency situation arises, medical professionals can quickly understand and respond to their needs. And if they are caught in an emergency situation, a 100 mg vial of a medication called hydrocortisone and a syringe should always be on hand, both at home and when traveling. These items can be used to quickly address their condition in an emergency. Taking these precautions can help them avoid complications and get the right care when they’re in critical need.