What is Hypothyroidism (Hypothyoid)?
Hypothyroidism is a condition where the body does not have enough thyroid hormone. The reasons and symptoms for this condition can vary. Hypothyroidism is mainly split into two types: primary and secondary. Primary hypothyroidism happens when the thyroid gland doesn’t produce enough thyroid hormone. Secondary hypothyroidism, which is less common, happens when the thyroid gland is working fine but there is a problem with the pituitary gland or hypothalamus. If left untreated, hypothyroidism can increase the risk of illness and death. In the United States, the most common cause is an autoimmune thyroid disease called Hashimoto thyroiditis. Worldwide, however, the major cause is not having enough iodine in the diet.
Symptoms can range from none at all, with people only discovering they have the condition through routine blood tests, to severe symptoms known as myxedema coma. Traditional symptoms like feeling cold, puffiness, decreased sweating, and skin changes may not always be present. Doctors usually use a serum TSH level test first to check for primary hypothyroidism. Classic signs in blood tests are high TSH levels and low free T4 levels. Fortunately, hypothyroidism can be easily diagnosed nowadays using simple blood tests and can be treated with thyroid hormone from outside the body.
What Causes Hypothyroidism (Hypothyoid)?
Hypothyroidism, a condition where the body doesn’t produce enough thyroid hormones, can be split into two types: primary and secondary (or central). Primary hypothyroidism is when the thyroid gland itself isn’t able to make enough thyroid hormone, whereas secondary hypothyroidism is less common and develops when other parts of the body, like the pituitary gland or hypothalamus, aren’t working correctly.
If we talk about the main causes of primary hypothyroidism, they can change depending on where in the world you are. In places where there isn’t a lot of iodine, the lack of this nutrient often leads to primary hypothyroidism. In areas where there’s enough iodine, the most common causes are autoimmune diseases, with an inflammatory condition known as Hashimoto thyroiditis being the top one in the United States.
Beyond this, there are many other reasons someone might develop primary hypothyroidism. For example, some women can develop a condition known as postpartum thyroiditis after giving birth, which can lead to temporary or, in rare cases, permanent hypothyroidism. Similarly, treatments like radioactive iodine for Graves disease can lead to permanent hypothyroidism in the majority of patients. Other less common causes include a disease known as subacute granulomatous thyroiditis, genetic conditions, or the side effects of certain medications.
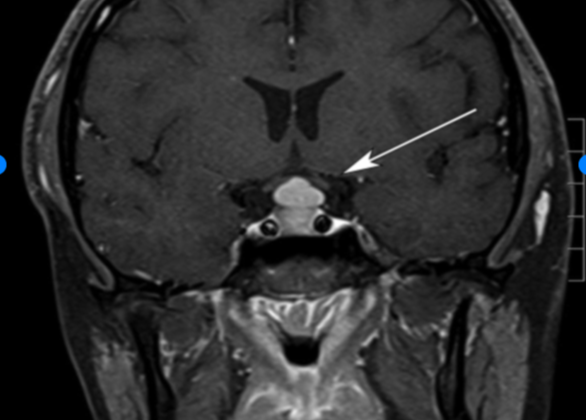
If we talk about secondary or central hypothyroidism, this condition stems from problems in the body’s hormone control center – the hypothalamic-pituitary axis. Several factors can cause issues here, like tumors, specific syndromes, radiation therapy to the brain, or certain medications.
Risk Factors and Frequency for Hypothyroidism (Hypothyoid)
The National Health and Nutrition Examination Survey, or NHANESIII, found that overt hypothyroidism, a condition related to the thyroid gland, affects 0.3% of individuals who are 12 years old and above in the US. Meanwhile, subclinical hypothyroidism, which is a mild form of the condition, affects 4.3% of the same group. Certain factors increase the risk of having thyroid issues, such as being female and getting older. Additionally, the presence of certain antibodies can also indicate a higher chance of getting this condition. The study also found that women who were born small and had a low body mass index during childhood have a higher risk of developing hypothyroidism.
Signs and Symptoms of Hypothyroidism (Hypothyoid)
Hypothyroidism is a condition that often shows mild and vague signs, making it difficult to diagnose. Sometimes, people experience traditional symptoms like cold intolerance, puffiness, decreased sweat, and changes in skin. However, these might not always show up. Other symptoms to watch out for include dry skin, voice changes, hair loss, constipation, fatigue, muscle cramps, sensitivity to cold, sleep issues, abnormal menstrual cycles, weight gain, and unexpectedly producing breast milk. It’s important to disclose complete medical, surgical, medication, and family history to your medical caregivers. It’s also helpful to share any experiences of adverse pregnancy or problems with your newborns.
Sometimes, less common symptoms can point to hypothyroidism. These can include depression, anxiety, psychosis, cognitive issues (such as memory loss), abdominal fluid buildup (ascites), muscle breakdown (rhabdomyolysis), fluid around the heart (pericardial effusion), carpal tunnel syndrome, sleep apnea, low sodium levels (hyponatremia), high cholesterol levels, heart failure, prolonged heart rhythm measurements (QT interval), amongst others. If you have Hashimoto disease, a type of hypothyroidism, you might experience a full feeling in your throat, painless thyroid enlargement, or periodic neck pains or sore throat.
While diagnosing hypothyroidism, doctors often find that the thyroid examination results are normal. However, a thorough physical examination could offer clues. Signs of hypothyroidism can be quite subtle but can include a range of symptoms:
- Enlarged thyroid gland
- Weight gain
- Slow speech and movement
- Dry skin
- Coarse and brittle hair
- Pale or yellowish skin
- Unemotional facial expressions
- Enlarged tongue
- Slow heartbeat
- Fluid around the heart
- Prolonged ankle reflex relaxation time
Testing for Hypothyroidism (Hypothyoid)
When testing for an underactive thyroid, also known as hypothyroidism, doctors usually start by checking the levels of your thyroid-stimulating hormone (TSH) in your blood. Classic signs of hypothyroidism in your lab results would be high levels of TSH and low levels of free T4, another important thyroid hormone. However, in some cases, only the TSH levels might be high with free T4 levels within normal limits, indicating a condition known as subclinical hypothyroidism.
Your doctor may also check for certain antibodies in your blood that might suggest an autoimmune thyroid disease. If you have subclinical hypothyroidism and those antibodies are present, your risk of developing full hypothyroidism increases. In fact, research has shown that about half of these patients would likely progress to primary hypothyroidism within 20 years.
Besides thyroid hormones, your doctor may also look for other changes in your blood. These can include high cholesterol, high muscle enzymes, high liver enzymes, and possible anemia. Other tests could be included based on the severity of your condition.
If your hypothyroidism is suspected to be caused by issues with your pituitary gland or the hypothalamus in your brain, known as central hypothyroidism, doctors will primarily rely on free T4 levels rather than TSH for diagnosis. Unlike in primary hypothyroidism, ultrasound or imaging of the neck is not typically suggested for this type of hypothyroidism.
In a hospital setting, doctors might check TSH levels if they suspect a problem with your thyroid. Sometimes, patients who are sick but do not have thyroid disease might show some variation in their TSH levels. However, if TSH levels are extremely high, hypothyroidism is likely.
While there isn’t a standard rule for screening the public for thyroid disorders, the American Thyroid Association suggests that it be done every five years, beginning at age 35. It is especially recommended for:
- Women aged 60 and above,
- Pregnant women,
- People who’ve had irradiation of their head or neck,
- People with autoimmune disorders or type 1 diabetes,
- People with the presence of certain thyroid antibodies,
- People with a family history of thyroid disorders.
Treatment Options for Hypothyroidism (Hypothyoid)
Hypothyroidism is usually treated with a medication called levothyroxine. The patient typically takes between 1.6 to 1.8 micrograms per kilogram of their body weight per day. Older patients and those with a heart condition called atrial fibrillation might require a smaller starting dose, which is then increased gradually as necessary.
Levothyroxine is usually taken 30 to 45 minutes before breakfast or at least 3 hours after dinner, according to what is most suitable for the patient. The absorption of levothyroxine can be affected by some diet supplements and medicines, so there should be at least a 4-hour gap between consuming these and taking levothyroxine. Some commonly used medications, such as proton pump inhibitors, can also decrease the absorption of levothyroxine. It’s important for some patients to stick to the same brand of levothyroxine, as slight variations in dose can affect certain patients.
In cases where the patient can’t take medicine by mouth or if severe hypothyroidism is suspected, intravenous (IV) levothyroxine can be used in the hospital. This is usually 50-75% of the oral dose. This particular method is mainly reserved for severe situations due to the high cost of the IV formulation.
Liquid and gel capsule forms of levothyroxine are used when a patient has trouble absorbing the tablet form. To monitor how well the treatment is working, blood tests should be performed every 4-8 weeks until the desired hormone levels are reached. If they remain stable, testing can be done less frequently.
Aside from monitoring hormone levels, it’s also important to check for signs of heart issues such as angina and a specific type of irregular heartbeat called atrial fibrillation, especially in patients with pre-existing heart disease. Those treated with high levels of levothyroxine for a prolonged period might need osteroporosis screenings as well.
In cases where a patient’s symptoms persist in spite of having the right hormone levels, a more detailed health assessment might be necessary. For patients who don’t respond to standard treatment, a combination of hormones T3 and T4 might be considered, but there’s a potential risk of heart rhythm problems.
Treatment’s goal is to alleviate hypothyroidism symptoms, improve the patient’s well-being, and normalize hormone levels. However, because the symptoms aren’t exclusive to hypothyroidism, the patient might have another condition if symptoms persist after hormone levels have been normalized.
Furthermore, levothyroxine can make co-existing adrenal gland problems worse. It’s important to test and treat these cases of adrenal insufficiency while waiting for the results. Severe hypothyroidism can occur alongside adrenal insufficiency, so ensuring it isn’t present is crucial. If a patient has confirmed adrenal insufficiency, thyroid tests should be reconsidered after treatment for adrenal insufficiency.
What else can Hypothyroidism (Hypothyoid) be?
Hypothyroidism, a condition where your thyroid is underactive, can be difficult to diagnose because its symptoms are often mild. These might include feeling tired or having trouble focusing, which could also be caused by conditions such as iron deficiency anemia, sleep apnea, depression, or diseases affecting your joints. Here are some other conditions that might be considered when diagnosing hypothyroidism:
- Euthyroid sick syndrome (a thyroid condition often seen in critically ill patients)
- Goiter (an enlarged thyroid)
- Myxedema coma (a severe complication of hypothyroidism)
- Anemia (low iron in your blood)
- Riedel thyroiditis (a rare type of thyroid inflammation)
- Subacute thyroiditis (inflammation of the thyroid after a viral infection)
- Thyroid lymphoma (a rare thyroid cancer)
- Iodine deficiency (low iodine levels in your body)
- Addison disease (a disorder where your adrenal glands don’t produce enough hormones)
- Chronic fatigue syndrome (a disorder characterized by extreme fatigue)
- Depression (a mood disorder causing persistent feelings of sadness)
- Dysmenorrhea (painful menstrual periods)
- Erectile dysfunction (difficulty getting or keeping an erection)
- Familial hypercholesterolemia (an inherited disorder characterized by high cholesterol levels)
- Infertility (difficulty getting pregnant)
Because the symptoms of hypothyroidism can overlap with many other conditions, it’s essential for doctors to carefully consider these different diagnoses.
What to expect with Hypothyroidism (Hypothyoid)
If hypothyroidism is left untreated, it can lead to serious health risks and even death in severe cases. For children, untreated hypothyroidism can cause serious mental development issues. In adults, it is a major cause of heart failure. However, with the right treatment, most patients can expect a good outcome, with symptoms often disappearing within a few weeks or months.
Possible Complications When Diagnosed with Hypothyroidism (Hypothyoid)
A severe form of hypothyroidism, known as myxedema coma, is a critical medical emergency. Quick spotting and quick treatment in an intensive care unit (ICU) are critical, but even with these, death rates can be as high as 25% to 60% in some cases. This condition often shows up as mental confusion, abnormal body temperature, seizures, low sodium or sugar levels, irregular heartbeats, heart failure, breathing failure, and fluid buildup.
People are more likely to experience a myxedema crisis if they don’t take enough thyroid medication, stop their treatment, have undiagnosed hypothyroidism, or have another illness like a widespread infection. In the ICU, supportive care would include the management of fluids and body salts, aid with breathing, and using medications to increase blood pressure, as well as tackling low body temperature and any existing illnesses.
For treating this condition, healthcare providers initially use an injectable form of the hormone cortisol in high doses, followed by an injection of synthetic thyroid hormone. Once the patient starts to improve, the treatment is switched to an orally taken synthetic thyroid hormone. This initial stage involves using steroids because these patients might also have a deficiency of adrenal hormones, which can lead to a crisis if the thyroid hormone deficiency is addressed without tackling the adrenal one. This happens because replacement of the thyroid hormone can turn up the body’s metabolism. While waiting for test results for adrenal deficiency, treatment with steroids must begin.
- Quick response
- Treatment in intensive care unit (ICU)
- Managing fluids and salts in the body
- Support with breathing
- Medications to increase blood pressure
- Addressing low body temperature
- Dealing with other illnesses
- Initial treatment with injectable cortisol
- Injection of synthetic thyroid hormone
- Oral synthetic thyroid hormone
- Starting steroids treatment while waiting for test results
If the treatment works, the patient’s heart, lung, and mental functioning should improve. Also, the lab results should get better, including an increasing level of free T4, a type of thyroid hormone, which should be checked every one to two days at the start of the treatment. In some cases, a low-dose of another synthetic thyroid hormone can be considered until the initial improvement. The TSH, a hormone that stimulates the thyroid gland, may not show these changes because it can take up to four weeks to return to normal; hence, it may not be helpful. A consultation with an endocrinologist is always a good consideration.