What is Nontoxic Goiter?
Goiter is the term used when the thyroid gland grows larger than normal. This can happen without any issues in how the thyroid functions, known as a nontoxic goiter. It’s not caused by inflammation or diseases that cause uncontrolled cell growth. The goiter might grow uniformly or might have localized growth. If it gets very big, it can extend into the space behind the breastbone. Because this space is limited, the goiter could potentially press on the upper part of the windpipe, voice box nerves, and food pipe.
Problems with the supply or breakdown of iodine always cause nontoxic goiter. The thyroid gland usually weighs about 25 grams, isn’t physically large and is shaped like a butterfly. It’s located near the front of the neck, in front of the voice box and windpipe. It’s made up of a right lobe and a left lobe connected in the middle. This middle part rests against the second and the third rings of the windpipe, with the lobes extending on either side. It goes from the thyroid cartilage at the top to the fourth windpipe ring at the bottom.
This gland secretes thyroid hormones when it’s stimulated by the thyroid-stimulating hormone (TSH) produced by the pituitary gland in the brain. These hormones (known as T4 and T3) are vital for the body’s energy use and metabolism. The thyroid also produces a hormone called calcitonin, which helps regulate calcium levels in the body. When the body doesn’t produce enough thyroid hormone (due to a lack of iodine in the diet, for example), more TSH is released. Over time, this can lead to an increase in the cells in the thyroid gland, leading to an increase in its size.
What Causes Nontoxic Goiter?
A nontoxic goiter is an enlargement of the thyroid that isn’t harmful or cancerous. It can either appear evenly spread out across the area (diffuse) or have multiple distinct lumps (multinodular). There are a few reasons why this might happen:
– Changes in your body’s hormones, such as during puberty or pregnancy might lead to it.
– A lack of iodine in your diet could also be the reason as iodine is essential for the production of thyroid hormones (this is often seen in areas where there isn’t enough iodine in the food and water).
– Sometimes, there’s a problem with the thyroid’s development (this can happen sporadically).
– Certain foods or drugs like cabbage, or medicines containing para-aminosalicylic acid could interfere with how your body uses iodine and lead to a goiter.
– Exposure to radiation could also trigger your thyroid to enlarge.
– If your pituitary gland releases too much thyroid-stimulating hormone (TSH), it could cause your thyroid to grow.
– Your body’s immune system might mistakenly attack your thyroid leading to a goiter (a condition called autoimmune thyroid disease).
– Infections could also lead to a swelling of the thyroid gland.
– A type of condition called granulomatous disease can lead to inflammation and growth of the thyroid.
Risk Factors and Frequency for Nontoxic Goiter
The thyroid hormone is produced from iodine, which we get from the food we eat. Iodine comes from the soil, but in areas with lots of rain or mountains, iodine can get washed away, leaving the soil and food grown there lacking in iodine. People living in these iodine poor areas are more likely to develop a condition called goiter, a swelling of the neck resulting from an enlarged thyroid gland. However, research has shown that providing iodine supplements, such as in table salt, can significantly reduce goiter.
In the United States, goiter that is not caused by a toxic condition and develops sporadically is very common, with a rate of occurrence of about 5%. In people aged 60 or older, about 5% to 6% have noticeable, or palpable, lumps called nodules in their thyroid, while about 50% of the same age group has non-detectable, or nonpalpable, nodules found only during an autopsy.
Worldwide, a massive 2.2 billion people suffer from some form of iodine deficiency, with a majority living in iodine-deficient areas. The severity of iodine deficiency is directly linked to the prevalence of goiter. Thus:
- With no iodine deficiency, about 5% of people will develop goiter.
- With mild iodine deficiency, the rate of goiter increases to between 5% to 20%.
- With moderate iodine deficiency, the rate is between 20% to 30%.
- With severe iodine deficiency, over 30% of people will develop goiter.
Goiter is between 1.2 to 4.3 times more common in women than in men, and those with lower socioeconomic status are more at risk. This is likely due to decreased iodine intake. Both sporadic goiter due to abnormal formation and endemic goiter typically occur during childhood, with the thyroid gland enlarging as individuals age. It should be noted that there is no racial correlation to developing a goiter.
Signs and Symptoms of Nontoxic Goiter
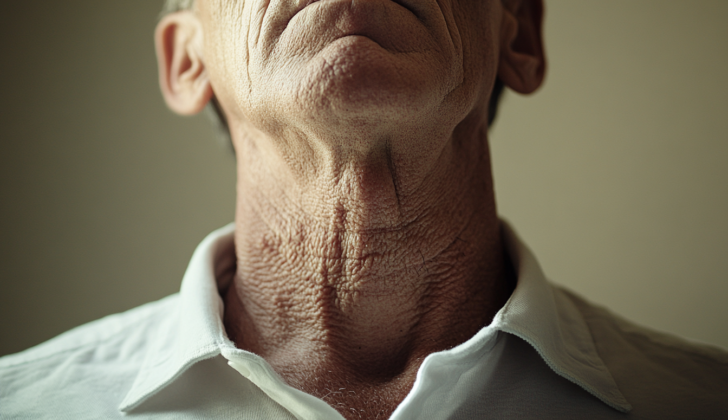
Non-toxic goiters, or swellings in the thyroid gland, often do not cause noticeable symptoms. Sometimes, these swellings are found unintentionally by the person or someone else. Certain individuals might experience issues such as trouble swallowing, difficulty breathing, or voice changes due to the goiter pressing on the nearby laryngeal nerves. Large thyroid swellings can also put pressure on neck veins, causing facial redness and discomfort. Pain is uncommon, but it can happen if there’s bleeding in a goiter nodule and sudden changes in the swelling size.
During a physical examination, a goiter appears as a lump in the middle of the neck that may be smooth or bumpy and moves while swallowing. It could potentially push the windpipe to one side or extend towards the chest. The presence of swollen lymph nodes in the neck could be a sign of cancer, so further testing would be needed. If the person has voice changes or if surgery is being considered, the vocal cords must be examined.
- Lump in the middle of the neck
- Goiter moves when swallowing
- May push the windpipe to one side or extend towards the chest
- Swelling could be seen in the neck’s lymph nodes
- Vocal cords must be examined if voice changes or surgery is considered
When asked to raise their arms during an examination, the goiter might move into the chest inlet, leading to symptoms like noisy breathing, difficulty breathing, or swelling of neck veins. This is called the Pemberton maneuver.
Testing for Nontoxic Goiter
Your doctor may need to perform several tests if they suspect you have a thyroid problem. Initial tests typically check if your body is producing too much, too little, or just the right amount of thyroid hormone. This is checked by measuring the levels of TSH, free T4, and T3 in your blood.
Next, an ultrasound might be done to look at any nodules, or small lumps, that might be present in your thyroid. Certain features of these nodules, such as being less reflective on ultrasound (hypoechogenicity), having tiny calcium deposits (microcalcification), having more blood vessels than usual (hypervascularity), and solid parts of complex nodules, could be signs of a problem. In such situations, your doctor might recommend a test called fine needle aspiration cytology, where a small sample of the nodule is taken using a fine needle. This test is guided by ultrasound to ensure accuracy.
A chest x-ray can also be helpful to look at a type of goiter (an enlarged thyroid) that grows behind your breastbone (retrosternal goiter). They also check if your windpipe (trachea) has been pushed to one side (tracheal deviation). If more detail is needed about these conditions, your doctor might recommend a CT scan or an MRI, which are more detailed types of scans.
Tests that use a small amount of radioactive material (radionuclide scanning) can be used to look at both the structure and function of your thyroid.
In addition, there are other tests that might be used to evaluate patients with an enlarged thyroid. These can include tests that check how well your lungs are working (pulmonary function tests), tests that check the flow of liquid when you swallow (barium swallow studies), and tests that record the rate of airflow (flow volume loops).
Before any operation on your thyroid, your doctor may also check your vocal cord movement using a tool called a laryngoscope. This helps to ensure the surgery doesn’t cause any damage to your voice.
Treatment Options for Nontoxic Goiter
A nontoxic goiter is a type of thyroid condition that develops slowly and often doesn’t present any symptoms. In most cases, it doesn’t require treatment and doctors will just keep an eye on it for any changes. Some people might suggest using medicine to treat a nontoxic goiter, but this approach is often debated because it usually doesn’t show much improvement, especially in goiters that have been present for a long time.
There’s one type of medication, called levothyroxine, that can sometimes help shrink a goiter. However, if the doctor prescribes this medication, they’ll need to monitor the patient closely to make sure that they don’t develop other health problems, such as abnormal heart rhythms, hyperthyroidism (which means the thyroid is too active), or bone thinning. It’s also important to note that if the goiter is functioning independently (referred to as “autonomous”), doctors usually don’t recommend levothyroxine treatment.
Surgery can be considered as a treatment in cases where the goiter is causing uncomfortable or harmful symptoms, or leading to complications. For instance, if a goiter is growing behind the breastbone (a condition known as “retrosternal goiter”), doctors often recommend surgery to remove it – even if the patient isn’t experiencing any symptoms – because waiting for symptoms to appear could make the surgical procedure more complex. That being said, doctors should thoroughly evaluate the patient’s overall health before surgery. During an emergency surgery for an active goiter, the patient would need medications like beta-blockers and antithyroid medications, as well as a higher dose of corticosteroids, a type of stress hormone. The patient would be closely monitored during and after surgery. A common issue after goiter surgery is low calcium levels, also known as hypocalcemia.
Besides surgery, another treatment option is radioiodine ablation, which uses radioactive iodine to shrink the goiter. However, this procedure can come with more complications compared to other treatments.
What else can Nontoxic Goiter be?
In simple terms, when a doctor sees a patient with a swollen thyroid (also known as a goiter), they need to figure out why it’s happening. It’s crucial for them to rule out the possibility of it being a symptom of cancer. The types of thyroid cancer that they need to consider include:
- Papillary thyroid cancer
- Follicular thyroid cancer
- Medullary thyroid cancer
- Thyroid lymphoma
Anaplastic thyroid cancer is another type, but it’s usually obvious because it shows up as a very large, hard lump that doesn’t move.
Aside from cancer, there are other causes of goiters the doctor needs to consider and rule out. These include different types of inflammatory conditions affecting the thyroid such as:
- Hashimoto thyroiditis
- De Quervain thyroiditis
- Riedle thyroiditis
All these conditions can appear similar to a non-cancerous goiter, so they need to be considered when making a diagnosis.
Surgical Treatment of Nontoxic Goiter
Thyroidectomy, a surgical procedure to remove the thyroid gland, is typically the primary treatment for non-toxic goiter when it starts causing notable symptoms or complications. This operation is generally safe and well-tolerated by most patients, including those with reduced physical function. It should ideally involve the removal of almost all, if not the entirety, of the thyroid gland.
One of the main benefits of this procedure is that there’s a very low chance of the goiter coming back. However, it’s important to bear in mind that like any surgery, thyroidectomy can have potential complications. These can occur during or after the surgery such as injuries to the recurrent laryngeal nerve (which controls the voice box) and hypoparathyroidism (a condition where low levels of parathyroid hormone lead to abnormal calcium/potassium balance in the body).
Furthermore, patients who have their entire thyroid gland removed will need to take thyroid supplements for the rest of their lives. This is required to replace the hormones that the thyroid gland would normally produce, which are necessary for regulating the body’s metabolism among other functions.
What to expect with Nontoxic Goiter
A non-toxic goiter is a harmless enlargement of the thyroid gland that only leads to cosmetic issues. However, if the goiter is large, it could potentially put pressure on the windpipe (trachea), voice box nerves (laryngeal nerves), and the food pipe (esophagus). But don’t worry, most benign goiters have a very good chance of recovery.
It is important to note, though, that a small proportion of benign goiters could cause overactivity of the thyroid gland known as hyperthyroidism, and some might even turn into cancer. So, life long monitoring is advisable.
Interesting to note, people who have pressure on their windpipe because of goiters, once surgically removed, the narrowing of the windpipe reverses and improves their lung function. So, the surgery not only removes the goiter but also can enhance their ability to breathe.
Possible Complications When Diagnosed with Nontoxic Goiter
Large goiters can lead to several health problems:
- Hyperthyroidism, also known as Job Basedow phenomenon
- Compression of the windpipe
- Potential to turn into a form of cancer
- Bleeding in the neck
- Possibility of getting infected
Preventing Nontoxic Goiter
People should ensure they are getting enough iodine in their diet. This is generally not a problem in the US as our salt often has iodine added to it. Patients who have had a part of their thyroid gland removed (known as lobectomy) will need treatment with a medication called levothyroxine. After thyroid surgery, doctors will keep an eye on the patient for 3-4 months to ensure their thyroid gland is producing enough hormones, a condition known as hypothyroidism.