What is Prolactinoma?
Prolactinomas are tumors that grow in the pituitary gland of your brain, that produce a hormone called prolactin. This type of tumor is the most common type that forms in the pituitary gland, accounting for nearly 40% of all cases. Prolactinomas can induce multiple different symptoms, which can be caused by the size of the tumor or because they are producing too much prolactin. These tumors are categorized based on their size: micro prolactinomas are smaller than 10mm, macroprolactinomas are larger than 10 mm and giant prolactinomas are larger than 4 cm. It’s important to understand that an elevated prolactin level is not always due to a prolactinoma; other factors, such as pregnancy, certain medications, an underactive thyroid (hypothyroidism), and effects by other pituitary tumors should be considered in assessing the situation.
What Causes Prolactinoma?
The exact reasons why Prolactinoma, a type of benign tumor that develops in the pituitary gland, develops is not well known. It appears to occur when pituitary gland cells that produce the hormone prolactin multiply due to some cell mutations.
There’s a certain gene, known as Pituitary tumor transforming gene (PTTG), which often shows up in higher amounts and sometimes appears to have mutations in people with this condition. This doesn’t necessarily mean it causes the condition, however.
Another component which has been found to have mutations in people who get pituitary gland tumors, especially prolactinoma, is a receptor for something called fibroblast growth factor 4 (FGF4), a protein which is involved in a variety of biological processes.
While most prolactinomas happen spontaneously and aren’t connected to any known risk factors, some can occur in families or as part of genetic syndromes. Examples of these include familial isolated prolactinoma and multiple endocrine neoplasia type 1 (MEN1).
In fact, between 15 to 60% of people diagnosed with MEN1, a disorder affecting the body’s endocrine glands, may also have a pituitary gland tumor and most of these tumors are prolactinomas.
Risk Factors and Frequency for Prolactinoma
Prolactinomas, a type of pituitary adenoma, make up around 40% of all clinically identified tumors in the pituitary gland. These are more frequent in women than in men, with the highest occurrence in women aged 25 to 34 years. Interestingly, the size of these tumors varies by gender. About 60% of men with prolactinomas have larger tumors (macroprolactinomas), while 90% of the women present with smaller ones (microprolactinomas).
- Prolactinomas make up around 40% of all identified pituitary gland tumors.
- The average occurrence of prolactinomas is about 10 per 100,000 in men and 30 per 100,000 in women.
- The highest prevalence of prolactinomas is in women aged 25 to 34 years.
- About 60% of men with prolactinomas have larger tumors, called macroprolactinomas.
- On the other hand, 90% of women with prolactinomas present with smaller tumors, known as microprolactinomas.
Signs and Symptoms of Prolactinoma
Prolactinomas, or tumors that affect the pituitary gland, can cause a variety of symptoms. Some people might not experience any symptoms and the tumor is found through brain scans for other conditions. Otherwise, these tumors can cause issues due to their size or because of an excess of the hormone prolactin (hyperprolactinemia).
The problems that can arise from the mass effect of the tumor include:
- Headaches
- Changes to vision, such as blurry sight or even visual loss
- Weakness in the muscles that control eye movement, particularly in the case of invasive tumors or pituitary apoplexy
- Rare cases of seizures, fluid buildup in the brain (hydrocephalus), and bulging eyes (unilateral exophthalmos)
- Pituitary apoplexy: this is an emergency situation caused by internal bleeding within the pituitary tumor. Symptoms can be severe headaches, vision changes, and a general loss of pituitary function (panhypopituitarism).
Hyperprolactinemia, or an excess of prolactin hormone, can lead to different symptoms in men, women, and children.
In males:
- Decreased sexual drive
- Impotence
- Issues maintaining an erection
- Low sperm count due to secondary hypogonadism
In females:
- Irregular or absent menstrual periods
- Difficulty conceiving, loss of sexual drive
- Unusual milk production even when not pregnant or nursing (galactorrhea)
In children and teenagers:
- Failure to grow at the expected rate (growth arrest)
- Delay in the onset of puberty
- Absence of the first menstrual period in girls (primary amenorrhea)
Both sexes can also experience bone thinning (osteopenia), as well as emotional issues like anxiety, depression, fatigue, and emotional instability. Interestingly, about 10% of prolactinomas can also produce growth hormone, which can result in abnormally large growth in childhood (gigantism) or adults (acromegaly).
Testing for Prolactinoma
To identify causes of high prolactin levels in the blood (hyperprolactinemia), your doctor needs to conduct a detailed medical history review and physical examination. Your doctor will check for symptoms like abnormal milk production, changes in body size, irregular periods, issues related to sexual function like impotence, and fertility problems. You may also need a visual field test performed by an eye specialist, especially if a large pituitary gland tumor (macroadenoma) is suspected.
Various conditions and factors can cause hyperprolactinemia. They can be classified into physiological (normal body processes) and pathological (disease or medical condition related) causes.
Normal body processes that could increase prolactin levels include:
– Pregnancy: hormonal changes during pregnancy can increase prolactin.
– Nipple stimulation in breastfeeding women: this natural response can increase prolactin.
– Stress: prolactin levels can temporarily spike due to stress.
Disease or medical conditions that could cause high prolactin include:
– Problems with the hypothalamus (the part of the brain that controls pituitary gland function), like certain brain tumors or medical conditions like sarcoidosis or a history of brain radiation treatment.
– Issues with the pituitary gland itself, like a prolactin-producing tumor (prolactinoma), hormone-related disorders (like acromegaly or Cushing’s disease), or inflammation of the pituitary gland (lymphocytic hypophysitis).
– Certain medications, such as some antipsychotics, antidepressants, anti-nausea drugs, blood pressure medications, and painkillers.
– Low thyroid hormone levels (hypothyroidism).
– Sometimes, the cause of high prolactin may not be identified, a condition known as idiopathic hyperprolactinemia.
Treatment Options for Prolactinoma
When doctors want to test for high prolactin levels in your blood, they will also run additional tests. This includes a full metabolic panel, a thyroid-stimulating hormone (TSH) test, and a pregnancy test for women who can still have children. Other hormones related to the pituitary gland (a small gland at the base of the brain) can also be checked. This will help to exclude any under-activity of the pituitary gland or other tumors.
Sometimes, patients can have very high prolactin levels but the tests may show them as lower than they actually are. This is called the “Hook effect.” If your doctor thinks this might be a case, they will repeat the test with diluted blood samples.
There can also be a situation where the test shows high prolactin levels, but actually, the prolactin level is low. This can happen when you have a type of prolactin that is larger than normal called macroprolactin. If you don’t have symptoms but the prolactin level is high, this macroprolactin test can be helpful. The lab can do a special process on the blood sample to separate the macroprolactin before testing for prolactin.
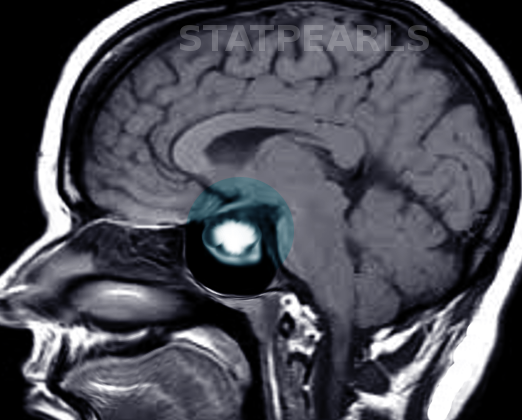
To better see the size and location of any potential masses causing the high prolactin levels, your doctor will prefer to use an MRI scan with a contrast agent called gadolinium. This will give a more detailed image of the area in and around the pituitary gland. If the tumor is near or pushing against the part of the brain responsible for vision, you might also have to undergo a vision test.
If you have a larger prolactin-producing tumor (macroprolactinoma) and it doesn’t cause any symptoms, your doctor might only monitor you. However, if it shows any symptoms or if you have a smaller tumor that gives symptoms, you should be treated with medication that mimics the action of dopamine – a hormone in our brain. The goals of treatment are to shrink the tumor, restore vision if it’s affected, stop abnormal milk production, and restore fertility or sexual function. The drug Cabergoline is preferred due to its success rate in reducing prolactin levels and aiding in tumor shrinkage.
Remember that most of the times these tumors are treated only with medications. The need for surgery or radiation therapy is reserved for cases where medical therapy isn’t enough.
Out of all the pituitary gland tumors, prolactin-producing ones are mainly treated with medications. In women, if amenorrhea (absence of menstruation) and bone thinning are the only symptoms, birth control pills can be used. If more treatment is needed, doctors will use dopamine-mimicking medications.
Two commonly used dopamine-mimicking drugs are Cabergoline and Bromocriptine. A third one, Pergolide, was withdrawn from the market due to concerns about valvular heart disease and a fourth one, Quinagolide, is not available in the United States. These medications help to suppress the production, release of prolactin, and reduce growth of the prolactin-secreting cells, thereby reducing the size of the tumor. They might cause some side effects such as nausea and dizziness.
Bromocriptine is preferred during pregnancy if neededas it has been studied more compared to Cabergoline. It is also cheaper but might produce more side effects like nausea, vomiting, nasal congestion, and low blood pressure when standing up.
If the Dopamine-like medication is successful in both reducing the prolactin level to normal and causing the tumor to become invisible on MRI, they can be slowly stopped after a minimum of two years of treatment.
If the treatment is not working well, and you are not trying to conceive, hormone replacement could be an option. For women, this involves estrogen and for men, testosterone therapy (if no fertility is desired) or human chorionic gonadotropin (if fertility is desired) should be started.
If all else fails, surgery may be needed and this will most likely be a transsphenoidal surgery where the tumor is removed from the base of the brain through the nose and sinus cavity. This can be an option for patients not responding to medical therapy, women with a large tumor who wish to be pregnant, or for stubborn tumors not responding to the medication Cabergoline. After surgery, if there are residual tumor leftovers, radiation therapy may be considered.
What else can Prolactinoma be?
There are several different conditions that might be responsible for certain symptoms that are being experienced. These conditions might include:
- Pregnancy
- Hypothyroidism (an underactive thyroid)
- Renal failure (kidney failure)
- Stimulation of the breasts
- Pituitary tumors (tumors on a small gland in the brain)
Possible Complications When Diagnosed with Prolactinoma
Possible effects include impaired vision due to pressure in the brain, cranial nerve damage, or a sudden and severe situation known as pituitary apoplexy. In some cases, people might face fertility problems or osteoporosis. Surgical procedures may also lead to complications such as loss of vision, leakage of cerebrospinal fluid (CSF), or a permanent condition known as hypopituitarism. Additionally, seizures can occur.
Effects and Complications:
- Impaired vision due to pressure in the brain
- Cranial nerve damage
- Pituitary apoplexy
- Fertility problems
- Osteoporosis
- Vision loss due to surgery
- Leakage of cerebrospinal fluid (CSF) after surgery
- Permanent hypopituitarism due to surgery
- Seizures