What is Thyroiditis?
Thyroiditis refers to a condition where the thyroid gland, a small organ located in the neck that releases hormones, gets inflamed. Different types of thyroiditis are classified based on how quickly symptoms appear, the root cause, and the specific symptoms shown by the patient. Autoimmune disease, a condition where the body’s immune system attacks its own cells, is the most frequent cause of thyroiditis. Specifically in the United States, a type of autoimmune disease known as Hashimoto thyroiditis is the leading cause of hypothyroidism, which is a condition where the thyroid does not produce enough hormones. Thyroiditis can lead to temporary or permanent conditions of hypothyroidism and hyperthyroidism, the latter being a situation where the thyroid produces too many hormones.
What Causes Thyroiditis?
Thyroiditis is a condition where the thyroid gland becomes inflamed. This can be due to auto-immune disorders like Hashimoto’s thyroiditis or Graves’ disease, infections, use of certain medications such as amiodarone, lithium, or interferons, or a condition called Riedel’s thyroiditis that causes scarring of the thyroid gland.
Thyroiditis can be painful, including forms caused by infections or trauma, or it can occur without pain, such as with autoimmune, postpartum (after childbirth), and drug-induced thyroiditis. These various types of thyroiditis can be categorized into acute (sudden), subacute (somewhat sudden), and chronic (long-term) forms.
Acute thyroiditis is often caused by a bacterial infection in the thyroid gland. This usually occurs in elderly people, those with long-term illnesses, and those with a weakened immune system. It is normally caused by bacteria like Staphylococcus or Streptococcus, but can also be caused by other types of bacteria and even fungi, especially in people with a weakened immune system. In children, it could be caused by abnormal structures in the throat called pyriform sinuses. This type of thyroiditis is rare due to the thyroid’s strong natural defenses, which include a robust blood supply and drainage system.
Subacute thyroiditis, also known as granulomatous thyroiditis, is believed to be caused by viral infections. It often comes after a person has an upper respiratory tract infection and is somewhat related to their genetic makeup, though the exact connections are still not fully understood.
Chronic thyroiditis, including conditions like Hashimoto’s thyroiditis and postpartum thyroiditis, appear to be linked to a person’s genetic makeup and certain viruses as well, which trick the body into attacking the thyroid gland. However, most people with these conditions have normal thyroid function despite having high levels of these misleading antibodies.
Postpartum thyroiditis occurs when a woman’s immune system mistakenly attacks the thyroid gland after childbirth. Additionally, certain medications can cause an inflammation of the thyroid gland. For example, amiodarone can lead to hypothyroidism, or low thyroid hormone levels, especially among people with underlying thyroid conditions or pregnant people since it interferes with the thyroid’s ability to produce hormones.
Other drugs, known as checkpoint inhibitors that are used in some cancer treatments, can also cause hypothyroidism by leading to an inflammatory response in the thyroid gland. Lithium, a medication used for mood disorders, can decrease the amount of thyroid hormone released, eventually leading to enlargement of the thyroid gland and sometimes a condition called goiter.
Riedel’s thyroiditis, a rare type of the condition, signifies progressive scarring within the thyroid gland. The exact cause remains unknown, but it may be linked to another condition known as IgG-4 related sclerosing disease, which also causes scarring of body tissues. This thyroid scarring may or may not be linked to scarring in other parts of the body.
Risk Factors and Frequency for Thyroiditis
Hashimoto thyroiditis is widely recognized as the biggest contributor to hypothyroidism, a condition where the thyroid gland doesn’t produce enough hormones. On the other hand, Graves disease takes the lead as the key cause of autoimmune hyperthyroidism, a condition where the thyroid gland produces too many hormones, in the United States.
- Consuming a lot of iodine could raise the risk of getting Graves disease.
- Interestingly, having an insufficient amount of iodine could help prevent autoimmune thyroiditis, the inflammation of the thyroid gland.
Signs and Symptoms of Thyroiditis
Thyroiditis is an inflammation of the thyroid gland, which can be acute (short term), subacute (medium term), or chronic (long term). The symptoms and causes of these types differ significantly and can sometimes be hard to distinguish.
Acute and subacute thyroiditis often have symptoms similar to an upper respiratory tract infection. Additional signs such as fever and neck pain may suggest acute infectious thyroiditis. In some cases, a recent history of radiation treatment on the neck or usage of radioactive iodine may cause this type of thyroiditis. During a physical exam, the thyroid gland of person with acute thyroiditis is usually tender and inflamed.
Chronic thyroiditis has many possible causes, and a detailed personal and family medical history is crucial in diagnosing it. This may include evaluation of current medications to identify any potential drug-induced thyroiditis or presence of autoimmune diseases in the family. Symptoms indicative of chronic thyroiditis can include problems swallowing, a choking sensation, or voice changes. These may be due to a large goiter (an enlarged thyroid), a large thyroid nodule, or Riedel thyroiditis. A physical exam can further confirm chronic thyroiditis, specifically examining the thyroid for any enlargement, tenderness, palpable nodules, or texture abnormalities.
Possible symptoms of drug-induced thyroiditis may include weight gain, fatigue, constipation, and dry skin in patients on specific medications, like amiodarone. It’s important to note that drug-induced thyroiditis can have minimal physical symptoms. Additionally, drugs such as checkpoint inhibitor immunotherapy can cause hypothyroidism, with symptoms like fatigue and weight gain. However, these symptoms may be mistaken for secondary hypothyroidism, as this drug can also cause hypophysitis.
Autoimmune thyroiditis and Hashimoto thyroiditis usually present as a painless goiter, an enlarged thyroid gland. Postpartum thyroiditis typically occurs after childbirth, with possible symptoms like rapid heartbeat, restlessness, and diarrhea. Patients with Riedel thyroiditis may have a fixed, hard, painless goiter. In most cases, these patients maintain normal thyroid function, but they can develop hypothyroidism.
Testing for Thyroiditis
To check if a patient has hyperthyroidism or hypothyroidism, a hormone test called Thyroid-stimulating hormone (TSH) would be done. The presence of autoimmune thyroid disease (a condition in which the body’s immune system attacks the thyroid) can be confirmed by checking specific antibodies in the blood. Tests like Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) can help detect infection in the thyroid gland.
An ultrasound is the most common way to look at the thyroid gland. This can show if the thyroid has inflammation (swelling) and can also detect growths in the thyroid gland (nodules). The characteristics of these nodules can help doctors figure out if they are harmless or cancerous.
A thyroid uptake and scan is a special test that can help distinguish between different types of thyroid inflammation in patients who may have thyrotoxicosis (overactive thyroid caused by excessive thyroid hormones) with low TSH and could have elevated levels of T4 and T3 hormones. A low uptake in the scan could indicate destruction thyroiditis (a type of thyroid inflammation like Hashimoto thyroiditis or infectious thyroiditis), while normal or increased uptake suggests production thyroiditis (like Graves disease).
The scan can also be used to differentiate production thyroiditis into either Graves disease (which would show increased uptake throughout the thyroid) or toxic adenoma (which would show a ‘hot’ nodule with increased uptake).
A procedure called fine-needle aspiration is done to test suspicious thyroid nodules for cancer. Generally, if a nodule is less than 10 mm, it can be monitored without this procedure.
In cases where infectious thyroiditis (a type of inflammation caused by infection) is suspected, tests include a thyroid ultrasound, blood cultures, and a fine-needle aspiration. Patients with radiation thyroiditis will likely have a history of radiation exposure or treatment with radioactive iodine, which assists in diagnosis.
There are different kinds of thyroid inflammations, including subacute thyroiditis, which is strongly linked with HLA-35. In this, ESR and CRP (blood tests used to check inflammation) and white blood cell count are usually quite high. The iodine uptake in these patients is usually low.
Chronic Thyroiditis (also known as Hashimoto’s thyroiditis) detection involves tests for specific antibodies and thyroid function tests which usually show high TSH and low T3 and T4 hormones. Certain medications may also induce thyroid inflammation, and baseline TSH should be obtained at the commencement of such treatments. If symptoms of thyroid dysfunction develop, thyroid ultrasound with iodine uptake scan can be done to distinguish between drug-induced destructive inflammatory thyroiditis and Graves disease.
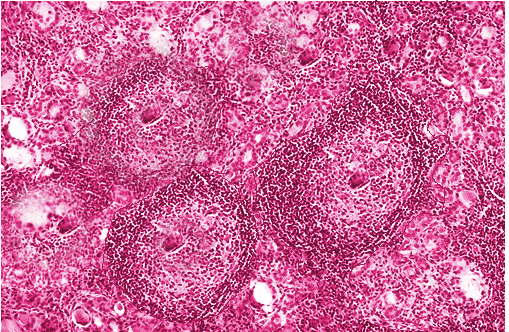
Postpartum thyroiditis after recent childbirth often presents similar symptoms to Graves’ disease, i.e., overactive thyroid, but can be differentiated using a 24-hour iodine uptake scan. Sometimes a Biopsy (collecting a small sample of tissue for testing) might be necessary for definitive diagnosis, especially with Riedel thyroiditis.
Treatment Options for Thyroiditis
Acute thyroiditis is an inflammation of the thyroid gland, which is located in your neck. The treatment for this condition will depend on the type of thyroiditis you have.
If you have suppurative thyroiditis, which is an infection of the thyroid, you can generally be treated without surgery. Antibiotics are used to treat the infection, and non-steroidal anti-inflammatory drugs (NSAIDs – a type of painkiller) can help to control severe neck pain and inflammation. If necessary, for example if an abscess (a pocket of infection) has formed, a surgical procedure may be required to drain the abscess.
When thyroiditis is caused by radiation treatment, the treatment is generally symptomatic, meaning it aims to relieve your symptoms. NSAIDs or prednisone (a type of steroid medication) can be used in severe cases. If you have radiation-induced thyroiditis, you are also at increased risk of developing hypothyroidism (a condition where your thyroid doesn’t produce enough hormones), so your doctor will monitor your thyroid function with blood tests.
Subacute thyroiditis is often self-limiting, which means it will resolve on its own. NSAIDs are often recommended to control pain. If symptoms of thyrotoxicosis (a condition caused by an excess of thyroid hormone) are severe, corticosteroids (anti-inflammatory medications) and beta-blockers (medications that reduce heart rate and blood pressure) can be used. Usually, the hypothyroid phase of this condition is mild and does not require treatment.
Chronic thyroiditis includes conditions like Hashimoto’s thyroiditis and Graves’ disease, both of which are autoimmune disorders where your body mistakenly attacks your thyroid. If you have Hashimoto’s thyroiditis and your thyroid function is normal, you may not need treatment but you should be monitored over time. Graves’ disease can be treated with medications such as methimazole or propylthiouracil, depending on individual factors. More permanent treatments for Graves’ disease include radioactive iodine treatment and thyroidectomy (surgical removal of the thyroid).
Postpartum thyroiditis, which occurs after childbirth, usually resolves on its own, and 80% of patients return to normal thyroid function. If your thyroid function is low, levothyroxine medication can be used and monitored with regular blood tests.
Amiodarone is a medication that can cause both hypothyroidism and hyperthyroidism. If diagnosed with hypothyroidism, you may continue to take amiodarone along with levothyroxine. If you’ve been diagnosed with hyperthyroidism type I, treatment is typically with beta-blockers and methimazole. For type 2 thyroiditis, the use of glucocorticoids (steroids) is recommended to alleviate hyperthyroid symptoms.
Lithium, a medication used in the treatment of mental health disorders, can cause thyroiditis. If this happens, treatment is usually to continue lithium and start treatment with levothyroxine. Lithium can also cause hyperthyroidism and Graves’ disease due to goiter formation (enlargement of the thyroid gland).
Riedel thyroiditis, a rare form of thyroiditis, is typically treated with surgery.
What else can Thyroiditis be?
When it comes to diagnosing symptoms of thyroiditis, there are several alternative conditions that need to be ruled out by your doctor. These could be:
- Bleeding into a thyroid cyst (acute hemorrhage)
- Thyroid nodule
- Thyroid cancer
- Tonsillitis (inflammation of the tonsils)
- Acute pharyngitis (inflammation of the back of the throat)
What to expect with Thyroiditis
Thyroiditis, which can involve any problems with your thyroid, generally has a good outlook. However, if you have a long-standing under-active thyroid (known as hypothyroidism), the condition can make you more likely to develop a severe type of swelling called myxedema coma. This condition is more common among older people and tends to have a high risk of causing death. Also, even when receiving treatment for an underactive thyroid, many patients may still experience ongoing symptoms. These lingering symptoms can negatively impact a person’s quality of life.
Possible Complications When Diagnosed with Thyroiditis
: Myxedema coma is a serious medical emergency, typically seen in older patients, characterized by pronounced hypothyroidism. Symptoms include low body temperature (hypothermia), low sodium in the blood (hyponatremia), and slow heart rate (bradycardia). Treatment needs to start immediately as soon as the condition is suspected, even before lab results are available. Steroids are usually given first, followed by thyroid hormone replacement therapy in order to prevent a potential adrenal crisis, which can arise if there is underlying adrenal insufficiency.
On the other hand, thyroid storm is a life-threatening condition that is usually triggered by a stressful event in a person who already has severe hyperthyroidism, like Graves’ disease. Symptoms can include high fever (hyperpyrexia), fast heart rate (tachycardia), agitation, and even psychosis, all backed by lab results showing low thyroid-stimulating hormone (TSH), and high levels of thyroid hormones (T4 and T3). The condition requires immediate recognition and treatment as it can be fatal. The Burch-Wartofsky diagnostic criteria help with early detection of a thyroid storm. The usual treatment involves beta-blockers, thionamides, and glucocorticoids. Iodine and cholestyramine can also be used on occasion.
Infectious thyroiditis, an infection of the thyroid, can lead to the formation of an abscess and ultimately a systemic infection (septicemia) if not treated quickly.
Patients with Hashimoto thyroiditis are at higher risk of developing thyroid lymphoma and carcinoma. Therefore, sudden growth or the emergence of new nodules in the thyroid should be a cause for concern.
Common Conditions and Symptoms:
- Myxedema coma
- Hypothermia
- Hyponatremia
- Bradycardia
- Thyroid storm
- Hyperpyrexia
- Tachycardia
- Agitation and psychosis
- Infectious thyroiditis
- Potential for abscess and septicemia
- Hashimoto thyroiditis
- Potential for thyroid lymphoma and carcinoma
Preventing Thyroiditis
Thyroiditis happens when your thyroid gland, which is responsible for producing a hormone called thyroxine, gets swollen. This hormone plays a key role in governing how our body uses energy. Any swelling or inflammation in this gland can cause it to produce either too much or too little of this hormone, leading to various symptoms. You might feel tired, gain weight, or feel depressed. Some people might even feel their heart beating faster, lose weight, or get anxious among other symptoms.
It’s important to discuss with your doctor about the most suitable treatment plan for you, as the treatment will depend on the specific type of thyroiditis that you have. Your doctor will need to conduct regular check-ups and laboratory tests to track the progress of your treatment and manage the condition effectively.












