What is Amebic Meningoencephalitis?
Free-living amebas are tiny, disease-causing organisms found mainly in freshwater bodies like lakes and rivers. They do not need a host to live and multiply. There are four main types of these amebas that pose a threat to humans: Naegleria (specifically Naegleria fowleri), Acanthamoeba (there are several species), Sappinia (specifically S. pedata), and Balamuthia (specifically Balamuthia mandrillaris). These amebas tend to cause infections in the brain and nervous system. However, Acanthamoeba, in particular, is known to cause both eye infections, known as keratitis, and widespread infections in the body.
These amebas can cause two different types of serious illnesses. The first is called primary amebic meningoencephalitis (PAM), and the second is granulomatous amebic encephalitis (GAE). The symptoms of PAM are very similar to those of bacterial meningitis, while the symptoms of GAE can mimic a brain abscess, inflammation of the brain, or meningitis. These amebic infections are extremely dangerous and often deadly. Even with treatment using antibiotics, the death rate from these infections is over 90%.
What Causes Amebic Meningoencephalitis?
Primary amebic meningoencephalitis (PAM) is an infection of the brain caused by a microorganism called Naegleria fowleri. This microorganism likes very warm conditions – it lives in temperatures above 86 degrees Fahrenheit and can even survive in temperatures up to 113 degrees Fahrenheit. You can find it in soil and warm fresh water sources, like ponds, lakes, rivers, streams, hot springs, and swimming pools that haven’t been treated with chlorine.
People usually become infected by swimming, diving, waterskiing, surfing, or exposure to hot springs. Also, using tap water to rinse the nasal passages can increase the risk of getting this disease.
Another related disease is called Granulomatous amebic encephalitis (GAE), an ongoing infection of the brain that’s caused by several types of Acanthamoeba. These tiny organisms can be found in the soil, salty water, sewage, and humidifiers. This suggests that they thrive in several types of environments and are more likely to cause infection.
Risk Factors and Frequency for Amebic Meningoencephalitis
PAM and GAE are extremely rare diseases, appearing only about 3.7 times per year around the globe. PAM seems to be more frequent in warmer areas, like the southern US and is usually seen in the hotter spring and summer months. This timing might be because people are more likely to join in activities involving water during these months. The average age of people affected by PAM is 12 years, but it can range from as young as eight months to as old as 66 years. There seems to be a higher chance for males to get the disease, as they make up 79% of the cases.
Signs and Symptoms of Amebic Meningoencephalitis
PAM, or primary amoebic meningoencephalitis, usually displays itself suddenly with high temperature, intense headache, sensitivity to light, feeling sick, vomiting, unusual behavior, seizures, and changes in mental condition. Often, people with PAM have a recent history of having been in warm, still water such as bathing or swimming in the last 1 to 9 days. A peculiar symptom associated with PAM is a change in sense of smell and taste. When a doctor does a physical examination, there might be signs of meningitis and problems with the cranial nerves. The disease can progress fast, putting high pressure on the brain which may lead to dangerous conditions like brain herniation and eventually death.
The Granulomatous Amebic Encephalitis, or GAE, however, has vastly different symptoms. GAE appears as a slowly developing disease, taking weeks to months to manifest. Symptoms include continuous headaches, low fever, sight problems, abnormal behaviour, and specific neurological issues. As the disease progresses, the patient experiences high pressure in the brain, seizures and can fall into a coma, leading to death. In patients with HIV, GAE can show up as specific neurological lesions similar to toxoplasma encephalitis.
Testing for Amebic Meningoencephalitis
The main way of diagnosing PAM, a type of brain infection caused by amoeba, is by taking a sample of cerebrospinal fluid (CSF) which surrounds the brain and spinal cord, through a process called a lumbar puncture. For diagnosing GAE, another type of brain infection also caused by amoeba, examination of brain tissue is necessary. Unfortunately, these types of infections are often not diagnosed until an autopsy is performed after the patient’s death.
Some lab findings that may suggest an infection include a high white blood cell count and a high opening pressure of the CSF. The count of white cells in the CSF may range from 300 to 26,000 cells/mm, with a specific type of white cell, polymorphonuclear cells, being the most common. Red blood cells are usually found in the CSF, and as the infection worsens, the fluid may become bloody. Other typical findings include low glucose levels and high protein levels in the CSF.
Definite diagnosis is achieved through observing motile trophozoites, which are a stage in the life cycle of the amoeba, under the microscope in a sample of CSF. Special stains like Giemsa or trichrome can aid in identifying the trophozoites. Alternatively, laboratory tests for the genetic material of the specific amoeba in CSF, biopsy, or tissue samples can also confirm the diagnosis.
To diagnose GAE, brain tissue showing both trophozoites and cysts, another stage in the life cycle of the amoeba, is required. Examination of the brain tissue will typically reveal inflammation around blood vessels, and the CSF may show a small increase in total cells present, predominantly lymphocytes, another type of white blood cell. It can also indicate high protein concentration, and low or normal glucose concentration. In rare cases, Acanthamoeba trophozoites can be seen in the sediment stained from CSF.
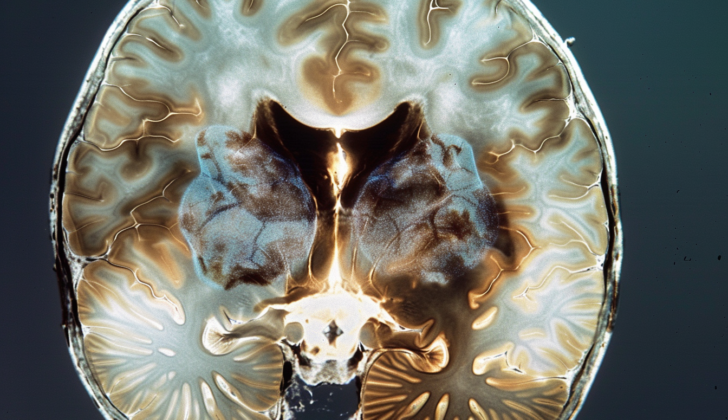
If there are clinical signs of localized involvement of the central nervous system (CNS) or increased pressure inside the skull, a head CT scan or MRI should be done before performing a lumbar puncture. MRI of the brain can reveal single or multiple abnormal tissue growths with a ring-like appearance. A CT scan could expose a buildup of fluid within the brain, thickening of the protective coverings of the brain, abnormal growths that resemble a tumor, single or multiple lesions, or abnormal tissue growths that exhibits ring-like enhancement. Upon examining the brain after death, it’s common to observe significant swelling and bleeding.
Treatment Options for Amebic Meningoencephalitis
Granulomatous amoebic encephalitis (GAE) is a very rare disease, and because of this, it’s difficult for doctors to determine the best way to treat it as there aren’t many clinical trials. Currently, a mixture of different medications is used. Authorities such as the Centers for Disease Control and Prevention suggest using several medicines together, such as pentamidine, sulfadiazine, flucytosine, and fluconazole or itraconazole. There are also other medication combinations that doctors might recommend. In some cases, removing brain lesions, or abnormal growths, can also be helpful.
Primary amoebic meningoencephalitis (PAM) is another condition for which the best treatment is unknown. Treatment duration can vary widely, from 9 to 30 days. The medication amphotericin B, given through a vein and directly into the spine, is often recommended. However, because PAM is a very severe disease with a high chance of death, doctors usually use several medications at once. These may include rifampin, fluconazole, miltefosine, azithromycin, and posaconazole. The latter has been shown to be effective in animal studies, and might replace fluconazole in the future, but more research is needed to confirm this.
There’s only been one reported case of GAE in a human caused by the amoeba Sappinia (specifically, S. diploidea). In this case, the person affected was a healthy farmer. His symptoms started with a headache, vomiting, blurry vision, and eventually losing consciousness after having a sinus infection. Doctors discovered a small, abnormal growth in his brain that turned out to be full of amoebas. It is thought that he breathed in the amoeba, causing his illness. He was treated with a combination of flucytosine, itraconazole, a medicine given via a needle into his veins called pentamidine isethionate, and azithromycin. Thankfully, this treatment led to his full recovery.
What else can Amebic Meningoencephalitis be?
The symptoms of PAM (Primary Amoebic Meningoencephalitis) are very similar to the symptoms of acute bacterial meningitis, and the results of cerebrospinal fluid (CSF) tests also show similarities. That’s why it’s very important to get a patient’s detailed background and medical history, especially if bacterial meningitis is suspected but the tests are negative and the patient’s condition doesn’t improve.
The list of conditions that a doctor would think about when diagnosing GAE (Granulomatous Amebic Encephalitis) includes the following:
- Bacterial brain abscesses
- Tuberculosis
- Nocardia (a type of bacterial infection)
- CNS aspergillosis (a type of fungal infection)
- Cryptococcosis (a type of fungal infection)
- Histoplasma (another type of fungal infection)
- Toxoplasmosis (a type of parasitic infection)
- Cysticercosis (a type of parasitic infection)
- CNS lymphoma (a type of cancer)
When these conditions are suspected, appropriate tests should be done to confirm the diagnosis.
What to expect with Amebic Meningoencephalitis
PAM, also known as Primary Amoebic Meningoencephalitis, is known to have a very high mortality rate. Some research studies have shown that it can be as close to all cases, or 99%. On average, from when symptoms start showing, it would take about 5.3 days before it gets life-threatening (this can differ, though, sometimes it only takes 1 day, sometimes it takes up to 12). And generally from the time of exposure to the life-threatening stage, it tends to take around 9.9 days (again, it can range, possibly from 6 days to 17).
Possible Complications When Diagnosed with Amebic Meningoencephalitis
Possible Severe Consequences:
- Hallucinations
- Seizures
- Coma
- Death
Preventing Amebic Meningoencephalitis
To prevent primary amebic meningoencephalitis, a brain inflammation caused by the Naegleria parasite, it’s important to follow these key steps:
- Avoid jumping or diving into still freshwater.
- Consider using nose plugs or holding your nose closed if you need to dive or swim in freshwater.
- Try to keep your head above water when swimming in freshwater, hot springs, and other untreated warm bodies of water.
- Avoid stirring up the bottom sediment when doing water-related activities.
- Use boiled, filtered, or sterilized water for rinsing your nose or sinuses instead of tap water.
In order to avoid Granulomatous Amebic Encephalitis (GAE), a severe brain infection, and keratitis, an inflammation of the eye’s cornea caused by the Acanthamoeba parasite, please consider:
- Changing your contact lenses at the recommended intervals.
- Always remove your lenses before any activities involving contact with water.
- Ensure to always wash your hands with soap before handling your contact lenses and follow the manufacturer’s instructions for cleaning them.