What is Epidural Abscess?
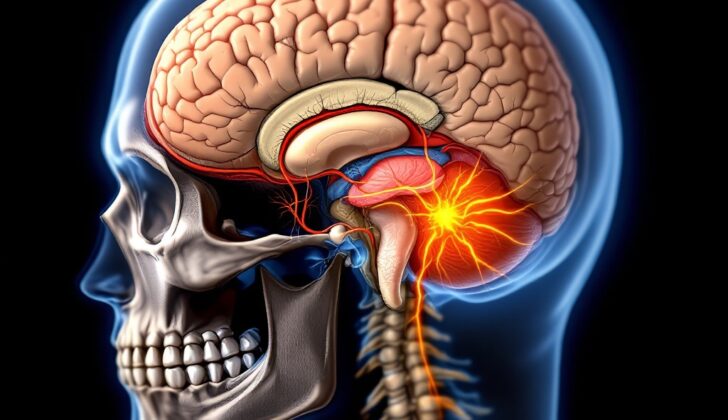
An epidural abscess refers to an infection occurring within the brain or spinal cord’s epidural space. This space is not normally present; it exists under the skull’s inner lining known as the dura mater.
Under typical conditions, there is no room between the dura and the skull. Yet, issues like infections, inflammation, or tumors can increase intracranial pressure, which in turn separates the bones from the tissue and creates an epidural space. This space can harbor blood, pus, or an abscess. It can extend the full length of the spine below the foramen magnum (a large opening in the base of the skull). The epidural space contains two sections: one true space behind and to the side of the spinal cord filled with fat and arteries, and another potential space at the front where the dura sticks to the back of the vertebral body.
Epidural abscesses can develop due to infections in the spinal or cranial epidural space. Intracranial epidural abscesses occur as a complication of brain surgery, trauma, or infections related to ear, nose, and throat, or other neck and chest procedures. Spinal epidural abscess can manifest acutely or chronically, affected by different clinical and laboratory findings, bacteria types, physical brain and spine details, and diseases.
Acute spinal epidural abscess is usually present for less than two weeks and is accompanied by fever and signs of body-wide inflammation, typically originating from a blood-borne source. This stands in contrast to the subtle, feverless, and longer-lasting chronic abscess which generally arises from a spread of vertebral osteomyelitis, which is an infection in the spine. Both types involve back and nerve root pain, but acute versions often present with increased white blood cells count in the blood and cerebrospinal fluid (the fluid around the brain and spinal cord), unlike the chronic version. Acute abscesses usually appear behind the spinal cord while chronic ones are commonly found in front of it. From a physical viewpoint, acute abscesses are filled with pus and fluid while chronic ones are characterized by tissue overgrowth.
What Causes Epidural Abscess?
IEA, or intracranial epidural abscess, typically begins with an external opening, often in the sinuses or ears. Certain bacteria, such as Streptococci (usually the kind that doesn’t need oxygen, known as anaerobic, like Peptostreptococcus), and other similar bacteria like Cutibacterium, which is naturally found on the skin, are commonly involved. Other causes can be gram-negative bacilli, which are a group of bacteria that can cause various infections, or fungi, and they usually start in the sinuses.
IEA can also happen as a complication after a brain surgery. The most likely causes in this case are staphylococci, especially a type called Staphylococcus aureus, and gram-negative bacteria. Infections can also spread from skull bone infections or from monitoring devices placed on the baby’s skull during birth.
Bacterial SEA (spinal epidural abscess) are the primary cause of this condition. Other forms of abscess in the spinal epidural space caused by tuberculosis, fungi, and parasites typically develop more slowly than bacterial ones. Besides fungal infections called candida, these causes are often found in tropical and subtropical regions of the world with limited healthcare resources.
Risk Factors and Frequency for Epidural Abscess
SEA, or spinal epidural abscess, isn’t common, with only 0.2 to 1.2 cases occurring for every 10,000 hospital admissions. It’s frequently seen in people with certain health conditions like diabetes, chronic kidney disease, alcohol dependence, those with a weakened immune system, and people who use intravenous drugs. SEA is nine times more likely to occur than IEA, or intracranial epidural abscess, and it’s typically a more sudden onset.
While IEA is not common, it is still the third leading cause of specific types of brain infections, right behind brain abscess and subdural empyema. In the past, it often resulted from infections in the head and neck region, such as sinusitis, mastoiditis, and ear infections. However, these days, it mostly happens due to complications after having brain surgery.
- SEA incidence is between 0.2 to 1.2 cases per 10,000 hospital admissions.
- It’s often seen in individuals with diabetes, chronic renal failure, alcoholism, immunosuppression, or intravenous drug use.
- SEA is nine times more common than IEA and usually more sudden.
- IEA is rare but is still the third most common brain infection, after brain abscess and subdural empyema.
- IEA used to be caused by head and neck infections like sinusitis, mastoiditis, and otitis but is now primarily due to complications from neurosurgical procedures.
Signs and Symptoms of Epidural Abscess
A spinal epidural abscess, or SEA, often presents with vague symptoms initially, making it hard to diagnose until it starts affecting the nervous system. Usually, patients with a SEA can feel tenderness around their spine that worsens over time. As the condition progresses, they may begin to experience radiating pain, usually a few days after the initial onset of tenderness in the spine. Around 90% of patients starts to develop such radiating pain. It’s also likely for a patient to have a fever and other nonspecific symptoms like fatigue, headaches, irritability, or vomiting.
Historically, the progression of symptoms in SEA has been divided into four overlapping stages by a researcher called Heusner in 1948:
- Spinal ache or back pain
- Root or radicular pain
- Weakness
- Paralysis
The time it takes to progress from backache to neurological issues can vary significantly. If untreated, severe backpain can turn into radiating pain in just 3 to 4 days and quickly cause spinal cord dysfunctions in the next 4 to 5 days. Swift surgical intervention may be needed at this stage as the condition can progress into complete paralysis within hours.
When we talk about Intracranial Epidural Abscesses (IEA), they can cause signs and symptoms either due to the infection itself, or due to a slow rise in pressure within the skull. Common symptoms include fever, headache, sluggishness, nausea, vomiting, and a sensitivity to light. IEAs are often complicated by surgeries or other invasive procedures. So anyone with a fever and headache, especially if they’ve recently undergone an operation on their brain, head, or neck, should be evaluated for this condition. It becomes even more crucial when there are other potential sources of infection around the head and neck, like sinusitis or persistent ear infections.
Testing for Epidural Abscess
Lab tests for patients with these conditions may not show specific results. Patients could have a mild increase in their white blood cell count and a higher level of C-reactive protein, a substance produced by the liver in response to inflammation. Blood tests could reveal the presence of bacteria in spinal epidural abscess (SEA) but not in intraspinal epidural abscess (IEA). Traditional X-rays of the spine might be unhelpful in diagnosing SEA, since there may not be any visible destructed bone tissue.
Furthermore, other imaging techniques – like bone and gallium scans (which show how your bones are functioning), or computed tomography (CT, a type of X-ray that takes images from different angles and uses computer processing to create cross-sectional images of bones, blood vessels and soft tissues inside body) – might be ambiguous and could lead to delays in identifying the condition accurately.
The reliable way to diagnose SEA used to be myelography – a type of imaging test that involves injecting a special dye into the area around the spinal cord and nerves. However, these days this test has been largely replaced by Magnetic Resonance Imaging (MRI), which uses a magnetic field and radio waves to produce detailed pictures of the body’s internal structures. MRI is just as sensitive and specific as a CT scan combined with myelography.
For IEA, both CT and MRI scans can help make a diagnosis, with the MRI providing more detail. Nowadays, a procedure called CT-guided needle aspiration is commonly used all over the world for both SEA and IEA. This involves using a CT scan to guide a needle to aspirate, or draw out, fluid or cells from the spinal area for testing.
Treatment Options for Epidural Abscess
Spinal Epidural Abscess (SEA) is a serious condition that can rapidly progress to severe spinal cord dysfunction within a matter of hours. An immediate diagnosis and treatment are critical. This treatment usually involves surgery to relieve pressure on the spinal cord and drain the abscess, which can be thought of as a pocket of pus. For most cases, this is the standard procedure. Efforts are also made to treat any existing infections that may have led to the abscess. The treatment regimen usually includes intravenous (through-the-vein) antibiotic therapy targeted at the likely causative organisms, including certain types of staphylococci, streptococci, and rod-shaped bacteria.
Generally, surgeons treat abscesses located at the back of the spinal cord by performing a procedure called a posterior laminectomy. This involves removing part of the vertebrae to access the infected and inflamed tissue, which is then drained and rinsed with a saline solution. A drainage system is typically left in place post-surgery to continue the rinsing process until the infection completely clears. Antibiotics used may include a third-generation cephalosporin like ceftriaxone, combined with an antibiotic that specifically targets staph bacteria, like rifampicin, nafcillin, or fosfomycin. The typical course of antibiotic treatment lasts 4 to 6 weeks, or 6 to 8 weeks if there’s an associated bone infection.
For extensive abscesses located at the back of the spinal cord, CT-guided needle aspiration may be used as an alternative to surgery in select cases. This approach may be suitable when there are no major symptoms of spinal cord compression or neurological damage. However, it’s essential to proceed with caution when considering non-surgical approaches.
Like most abscesses, Intracranial Epidural Abscesses (IEA) typically require a combination of drainage and antibiotic therapy for treatment. The abscess can be drained either via surgery involving small holes in the skull (burr holes) or a more extensive operation (craniotomy). If the abscess affects the protective layer of the brain (the dura), techniques using grafts or other materials to block the flow of pus may be useful.
Antibiotics should ideally be started soon after samples for laboratory testing have been taken. However, choosing the right antibiotic can be challenging due to the relative rarity of the condition. Therefore, physicians often start treatment with antibiotics that are effective against bacteria that commonly cause infections of the ear, sinuses, or other areas of the head and neck. This regimen may include third-generation cephalosporins, vancomycin, and metronidazole, and changes may be made based on lab results. The antibiotic treatment typically lasts 6 to 8 weeks and involves only intravenous agents, as oral ones may not reach sufficient levels in the cerebrospinal fluid (the fluid surrounding the brain and spinal cord) to be effective.
In some children with sinus-related IEA, it may be possible to manage the infection without cranial drainage procedures. The treating physician might choose this route if an effective sinus drainage procedure is possible and the abscess is not showing signs of increased pressure inside the skull, a potentially life-threatening condition.
What else can Epidural Abscess be?
Doctors need to consider the possibility of Spinal Epidural Abscess (SEA), a serious condition, when evaluating patients who have sudden or worsening back pain, fever, and tenderness in the spine area. This condition might not always show typical symptoms, especially in children who may show unusual features. In patients who have had the condition for a longer period, fever and other overall symptoms may not be as noticeable. It’s been noted in studies that half of the patients with SEA are initially misdiagnosed.
Intracranial Epidural Abscess (IEA), a related condition, can mimic symptoms of other issues in the brain, such as:
- Primary or secondary brain tumors
- Abscesses
- Bruising (hematomas)
- Infection in the space between the brain and its outer covering (subdural empyema)
Doctors also need to consider meningitis, inflammation of blood vessels, and giant cell arteritis (an inflammation of the lining of your arteries) when making a diagnosis.
What to expect with Epidural Abscess
If both IEA (Iliac Endarterectomy Aneurysm) and SEA (Spinal Epidural Abscess) are correctly and quickly diagnosed, and managed in a timely manner, the patients’ outcomes are usually very positive.
Possible Complications When Diagnosed with Epidural Abscess
An epidural abscess, while rare, is a serious infection that could lead to life-altering neurological complications. Fortunately, these complications can often be avoided or reversed with timely diagnosis and treatment.
As soon as a spinal epidural abscess (SEA) is diagnosed, medical professionals should adopt an urgency similar to treating critically ill patients. However, even with immediate action, some patients may still experience severe neurological complications. These complications could be due to pressure on the spinal cord or a localized blood clot (septic thrombophlebitis) causing tissue death from a lack of blood (ischemic necrosis). Although pressure on the spinal cord is a more common cause, blood clot-related issues can lead to sudden worsening in patients who were previously stable.
Doctors seldom rely solely on antibiotics for treatment because some patients’ neurological conditions may worsen regardless. These complications can develop suddenly and without notice. The resulting muscle weakness or potential paralysis might not be reversible, even with immediate surgery.
Key Points:
- Epidural abscess is a severe infection that can lead to life-altering neurological complications
- Early diagnosis and treatment can prevent these complications
- Upon diagnosis, immediate and urgent treatment is necessary
- Complications can be due to pressure on the spinal cord or a blood clot causing tissue death
- Doctors typically use more than just antibiotics for treatment
- Complications can develop suddenly and may not be reversible, even with surgery