What is HIV Retinopathy?
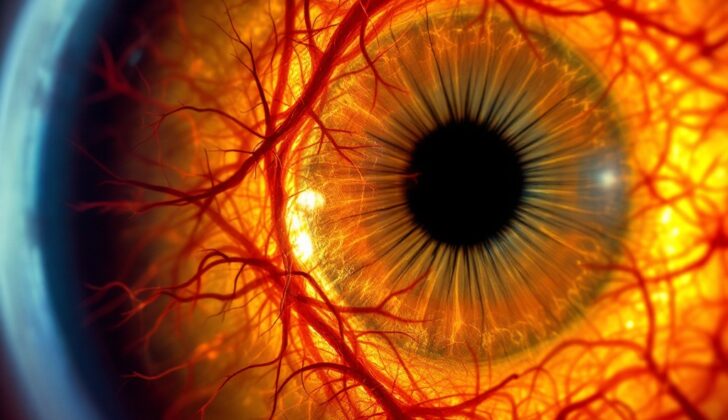
The Human Immunodeficiency Virus (HIV) is a type of virus that leads to a complicated multi-organ disease known as Acquired Immune Deficiency Syndrome (AIDS). Patients with HIV often have eye-related symptoms, which were first reported by a scientist named Maclean over 20 years ago. HIV retinopathy, a disease affecting the retina – the part of your eye that translates light into images – is quite frequent among HIV positive patients. It’s the leading cause of vision loss in these individuals.
What Causes HIV Retinopathy?
HIV is a type of virus that multiplies in certain types of white blood cells (CD 4 T lymphocytes) and can be passed from person to person through blood and other body fluids. If HIV isn’t treated, it generally progresses in three phases. Initially, there’s a stage of primary infection. Then there’s a period of clinical latency, which means the virus is present but not causing any symptoms. Finally, there’s a stage where the person can get various other infections or diseases, which is called AIDS. AIDS is officially present when a person has a disease that defines AIDS or when they have a count of CD4 T cells that is lower than normal (less than 200 per microliter).
Changes in the retina, the thin layer at the back of the eye that helps produce visual images, can occur in people with HIV/AIDS. This might be due to disease in the tiny blood vessels in the eye (microvasculopathy), other infections, or cancer. HIV microvasculopathy is considered to be the most common issue affecting the back of the eye and is seen in 40% to 60% of HIV-positive patients.
Another condition, cytomegalovirus retinitis, is one of the most common problems that can threaten sight for people with HIV/AIDS. However, its occurrence has been decreasing with the advancement in HIV medications, commonly known as HAART (highly active antiretroviral therapy).
Risk Factors and Frequency for HIV Retinopathy
According to the World Health Organization, as of December 2006, around 39.5 million people worldwide are infected with HIV. Research has shown that 5% to 25% of all HIV patients from developing countries may face blindness in their lifetime. Eye diseases, particularly those affecting the retina (the part of the eye sensitive to light) and choroid (the layer behind the retina), are very common amongst HIV patients and can lead to vision loss. With HIV patients living longer, it’s likely that the number of patients with opportunistic infections affecting the retina will increase.
There are also differences in the infections seen in HIV patients from developed and developing countries. CMV retinitis, a viral infection that can damage the eye’s retina, is less common in developing countries. On the other hand, HIV patients in these countries are more likely to become infected with toxoplasma, tuberculosis (TB), and the herpes zoster virus (HZV). These differences could be due to more exposure to these infectious agents, variations in HIV subtypes, and higher death rates early on in the disease in developing countries.
Signs and Symptoms of HIV Retinopathy
HIV can often lead to eye problems. One of the most common is something called microvasculopathy which affects 40% to 60% of people with HIV and is more common in people with low counts of a type of white blood cell called CD4. Microvasculopathy usually does not cause symptoms, but changes in the small blood vessels in the eyes can be seen during a checkup. These changes can include spots known as cotton wool spots towards the back of the eye, small bleeds, and changes in the shape of the blood vessels.
On the other hand, blockages in larger eye vessels are less commonly seen. If they do happen, it’s usually in combination with a viral infection in the retina, the light-sensitive layer at the back of the eye.
CMV retinitis is a viral infection of the eye that’s the most common type of eye infection seen in patients with AIDS. It used to be a leading cause of blindness in people with HIV/AIDS. This condition can take on three forms. The first, called the classical form, leads to large areas of dead tissue in the retina with hemorrhages, or bleeds, toward the back of the eye. These areas can merge and lead to more extensive damage. Patients may notice a loss of visual acuity or field. The second form, known as the indolent or slow-progressing variety, shows granular lesions around the edge of the retina with little or no bleeding. The third form, called frosted branch angiitis, involves more pronounced inflammation of the blood vessels. Vision loss in CMV retinitis can occur due to the disease affecting the central part of the retina or the optic nerve, as well as from complications such as retinal detachment and inflammation due to immune recovery. Treatment for HIV has changed the progression of CMV retinitis, leading to reductions in the overall number of this condition and signs not usually seen in traditional CMV retinitis, like inflammation in the front part of the eye and the vitreous, the clear gel that fills the eye.
Necrotizing viral retinitis leads to a whitening of the retina and bleeds, but the affected areas tend to be multiple, worsen quickly, and may be associated with skin lesions. There are two forms: ARN, which is associated with inflammation in the front part of the eye and vitreous, and PORN, which shows multiple, deep areas of inflammation in the retina, with minimal vitreous inflammation.
Eye inflammation due to infection with toxoplasma often involves both eyes and can affect multiple areas. It may also be associated with involvement of the central nervous system. The inflammation may look like CMV retinitis, but usually involves fewer bleeds and more pronounced intraocular inflammation.
Ocular syphilis involves inflammation in the front part of the eye or more widespread intraocular inflammation and is seen in 2% of patients. Another condition, Pneumocystis carinii choroiditis, is an opportunistic infection that appears as multiple, yellow spots in the choroid, the layer between the retina and the white of the eye, accompanied by a clear vitreous. Conditions involving the choroid, like cryptococcal and tuberculous choroiditis, may also be seen in patients with HIV.
Finally, patients with CMV retinitis who are on HIV treatment may suffer from a condition called immune recovery uveitis. This inflammation can lead to vision loss and is characterized by cataract, vitreous inflammation, swelling of the macula, swelling of the optic disc, formation of a fibrous membrane on the inner surface of the retina, and abnormal growth of fibrous tissue in the vitreous. It is a common cause of vision loss in people with AIDS who are responding to treatment for HIV. The severity of the inflammation depends on the patient’s immune function, the severity of CMV retinitis, the amount of CMV virus, and any previous treatment.
Testing for HIV Retinopathy
In terms of helping to understand how progression of HIV is affecting the eyes, there are several important tests and observations your doctor will likely use. These include simply talking to you about your symptoms and medical history, as well as eye examinations and monitoring levels of certain cells and particles in your blood.
One key factor that doctors often look for is the count of a type of cell in your body known as CD4 T-cell. They also now frequently examine something called the viral load. Both factors offer clues about potential eye problems related to HIV. A high viral load or low CD4 T-cell count can suggest that the eyes may be affected by HIV-related diseases.
Test of your vision, like how sharp it is at different distances (visual acuity) and how wide you can see (visual field), plus looking at how your pupils respond to light and how your eyes move, are also important for catching different infections or other HIV-associated conditions. The back part of your eye (the fundus) is specially examined for any changes.
The doctor can observe the fundus by conducting a dilated fundus examination. This involves using a special tool called an ophthalmoscope to look into the back of your eye, after widening (dilating) your pupils with special drops. If the doctor spots any problems in this check, they might then order further tests such as the VDRL or FTA-ABS tests, or tests for tuberculosis, to pinpoint the exact cause.
Treatment Options for HIV Retinopathy
HIV microvasculopathy is a condition that usually doesn’t show symptoms and typically doesn’t need any medical treatment.
If someone with HIV develops CMV retinitis, which is an inflammation of the retina caused by a virus, doctors would generally prescribe some specific medications. These medicines fight off the virus and help to treat this eye condition.
Necrotizing herpetic retinitis is a serious viral infection of the retina that also needs to be treated with antiviral medications, followed by a type of laser treatment after the infection clears up. This laser treatment can help prevent the retina from detaching, which can seriously harm your vision.
Furthermore, in the case of retinal choroiditis, which is an inflammation of the layer of blood vessels in the eye, doctors may prescribe a combination of specific medications. Interestingly, steroids, which are drugs that reduce inflammation, are not advised for treating this particular eye condition.
Pneumocystis choroiditis, a specific type of inflammation in the eye caused by a particular kind of fungus, can be treated with other medications. These medicines help your body fight off the fungus.
It’s also recommended that all patients with HIV take a medicine called fluconazole regularly to prevent a fungal infection called cryptococcosis, which can affect the brain and spinal cord.
If an HIV patient develops eye problems caused by tuberculosis or syphilis, there are specific drugs used to fight these conditions. Tuberculosis is treated with special anti-TB drugs, while syphilis is treated with penicillin.
What else can HIV Retinopathy be?
Here are some medical conditions that are related to the discussed topic:
- Cryptococcosis
- Cytomegalovirus (CMV) retinitis
- HIV encephalopathy
- Mycobacterium avium complex infection
- Microsporidiosis
- Progressive multifocal leukoencephalopathy
- Retinal or conjunctival microvasculopathy
- Varicella-zoster virus (VZV) retinitis