What is Malaria?
Malaria is a dangerous disease caused by a parasite and spread by a type of mosquito called the Anopheles. It’s a serious global health issue, potentially threatening the health of two billion people each year. This includes people living in 90 countries where the disease is common and 125 million travelers. Malaria also leads to the deaths of 1.5 to 2.7 million people each year.
The parasite that causes malaria has a complex life cycle, which results in recurring fevers as a key symptom. Despite its severity, the disease can be resolved quickly with prompt treatment. However, severe complications can occur, such as cerebral malaria (affecting the brain), severe anemia (low red blood cell count), coma, or even death.
The choice of antimalaria medicine used for treatment and prevention depends on the type of parasite, where the patient is or has traveled, the parasite’s resistance levels, and the patient’s characteristics. It’s essential to note that dormant infections can reactivate, causing the disease to reappear years after the initial exposure.
What Causes Malaria?
The time it takes for symptoms to appear after becoming infected with malaria can vary depending on the specific type of malaria. Generally, it takes around 8 to 11 days for P. falciparum; 8 to 17 days for P. vivax; 10 to 17 days for P. ovale; between 18 to 40 days (and possibly up to several years) for P. malariae; and 9 to 12 days for P. knowlesi.
The malaria parasite has a specific life cycle that causes what’s known as “malarial paroxysm” – a pattern of symptoms that includes chills, followed by several hours of fever, then sweating, and finally, the body temperature returning to normal. Specifically, a P. vivax infection follows a 48-hour cycle. This pattern, however, is less commonly noticed today thanks to quick identification and treatment.
Risk Factors and Frequency for Malaria
About 40% of the world’s population lives in or commonly visits places where malaria is widespread. Among the five Plasmodia species that cause malaria, P. falciparum is responsible for the most severe cases and deaths, especially in Western and sub-Saharan Africa. Other species like P. vivax, P. ovale, P. malariae, and P. knowlesi can be found in South Asia, the Western Pacific, Central America, and Southeast Asia respectively. It is estimated that every year, there are around 500 million cases of malaria leading to 1.5 to 2.7 million deaths. Most of these fatalities, specifically 90%, occur in Africa.
- Children under the age of 5, pregnant women, and people who have not previously been exposed to the disease are at the highest risk of getting malaria. This includes refugees in Central and Eastern Africa, individuals traveling to high-risk areas who aren’t immune, and immigrants returning to their countries of origin.
- Out of the 125 million travelers who visit high-risk areas every year, between 10,000 and 30,000 end up contracting malaria. About 1% of these people die from complications of the disease.
- Climate change is expected to escalate the impact of malaria. It’s predicted that a rise in average global temperatures by 3 degrees Celsius could cause an increase in malaria cases by 50 to 80 million.
Signs and Symptoms of Malaria
Malaria is a disease that can have various symptoms and its seriousness can depend on a person’s history and current status. When diagnosing malaria, it’s important to know things like where the person lives, if they’ve traveled recently, and if they’ve been exposed to certain conditions. Doctors should also consider if the individual has HIV, is pregnant or recently was, or if they have any other health conditions including G6PD deficiency, sickle cell disease, anemia, blood or other cancers, and any previous bouts with malaria and how they were treated.
The most common symptom of malaria is fever that lasts a week or more. If someone has recently traveled to an area where malaria is common and has such a fever, it’s very likely they need to be evaluated for malaria. In adults, other symptoms can include headaches, weakness, stomach problems, respiratory issues, and muscle aches. For serious cases, individuals may experience jaundice, confusion, seizures, and dark-colored urine.
Malaria symptoms in children can often be more general or can mimic a stomach bug with symptoms like fever, tiredness, nausea, vomiting, stomach pain, and drowsiness. Children with malaria are more likely to develop an enlarged liver or spleen and severe anemia, but they are less likely to experience organ failure than adults are. In severe cases, children can have frequent seizures and may also have low blood sugar and a concurrent bacterial infection, but they are less likely than adults to develop fluid in the lungs or kidney failure.
Malaria can affect pregnant women in a range of ways, depending on their immunity status. Some women might show no symptoms, while others may have severe ones. The infection can harm both the mother and the unborn child, and can lead to higher infant death rates because of low birth weight caused by growth restriction in the womb, early labor, or both. The specific type of malaria caused by P. falciparum can lead to complications including anemia in the mother, low birth weight, miscarriage, stillbirths, and malaria in the newborn. Pregnant women in their second or third trimester are more likely to develop severe malaria with complications like low blood sugar and fluid in the lungs compared to non-pregnant adults.
Testing for Malaria
When trying to identify fever within stable patients that might have been exposed to malaria, several tests are carried out. These include complete blood count, metabolic panel, coagulation panel, blood culture, urinalysis, chest x-ray, and blood smears. For patients with signs of mental confusion, additional tests such as lactate level, arterial blood gas, and lumbar puncture (taking a sample of fluid from the spine) may be necessary. This is because mental confusion could be a sign of cerebral malaria, a serious complication involving the brain.
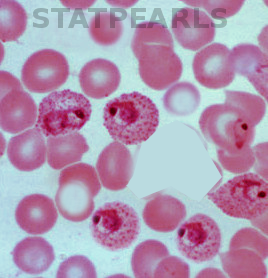
For those with malaria, the complete blood count test usually shows a low platelets count (thrombocytopenia) for about 60-70% of patients, and varying levels of anemia. Anemia is more common in adults and children, affecting 29% of adults and 78% of children. Malaria parasites invade red blood cells, causing them to burst and lead to anemia. The severity of anemia varies depending on the species of the malaria parasite.
Other test results for malaria patients could show liver cell injury and abnormalities in electrolyte levels (minerals and salts within the body necessary for nerve and muscle function). The liver damage is caused by parasite invasion while the electrolyte anomalies result from the release of intracellular contents and other damage like kidney injury and dehydration.
The gold standard or most trusted method for malaria diagnosis involves examining a blood sample under a microscope. This blood sample is applied on a slide and stained using a dye to make the parasites visible. It’s then examined under high magnification to avoid missing low level infections or delicate ring forms which are shapes of the parasite within the red blood cells. The type of malaria parasite is determined by observing and identifying specific appearances within the red blood cells.
It’s important to note that a first test resulting negative doesn’t entirely rule out malaria. This is because the infected red blood cells can be hidden within the blood vessels, and in such cases, the test should be repeated after 12 and 24 hours. Other methods for diagnosis include rapid diagnostic testing, microhematocrit centrifugation, and polymerase chain reaction which are all specialized tests to detect the presence of malaria parasites.
Treatment Options for Malaria
If you are diagnosed with malaria, your doctor will most likely treat you with medications designed to kill the malaria parasites in your body. You might need to stay in the hospital for at least a day, just to make sure your treatment is working well and you are responding positively. In severe cases, where the patient is notably unstable, particularly those with brain-involved malaria or substantial respiratory issues, intensive care may be required.
The treatment typically involves a combination therapy that targets both the liver and blood stages of the disease. Various antimalarial drugs may be used for this purpose, including chloroquine, hydroxychloroquine, primaquine, artemisinin-based combination therapy (ACT), and atovaquone-proguanil. Chloroquine and hydroxychloroquine are man-made forms of quinine, a naturally occurring compound that disrupts the growth of the malaria parasite. However, in South Asia in particular, the malaria parasite has developed resistance to these drugs, which is a concern for doctors.
Primaquine is another drug that is used to treat malaria. It is particularly useful against malaria caused by the types of malaria parasites P. vivax and P. ovale, due to its ability to eradicate liver parasites and prevent the malaria disease from recurring in the future. However, primaquine is not given to pregnant women and individuals with a lack of an enzyme called G6PD due to potential health issues. Artemisinins are active against all stages of the parasite’s life cycle.
Atovaquone targets a vital part of the malarial parasite’s cells, preventing them from producing energy and eventually killing them. Proguanil is typically given in combination with atovaquone, which makes the malarial parasites more susceptible to atovaquone’s effects. This combination medication is effective against both liver and blood stages of the malaria parasite’s life cycle.
Guidelines provided by the US Centers for Disease Control and Prevention (CDC) in 2019 recommend different treatment strategies based on the specific type of malaria parasite, the patient’s overall health condition, the patient’s age, and the specific regional strains of malaria that may be more or less resistant to certain medications.
In some regions where malaria is common, the disease-causing parasites have developed resistance to several common treatments, making the disease harder to treat. Because of this, complex treatment regimens involving multiple medications are sometimes required to treat malaria effectively, especially in these regions.
Each person’s treatment plan is tailored to their individual needs, taking into account factors like their overall health, the specific type of malaria they have, and whether they’re pregnant. Pregnant women with malaria require special treatment considerations to protect the health of both the mother and the unborn child.
Those with severe malaria infections – those causing instability in patients – require intensive medication and close monitoring, and their treatment plans are typically prescribed under the guidance of an infectious disease specialist.

What else can Malaria be?
When a patient comes in with an unidentified fever, there are many possibilities that doctors need to consider. What the likely cause is can depend heavily on where the patient lives or has been visiting, and on their age. According to a 2017 review, fever in people returning from travel could most often be due to protozoal malaria (77%). Other options include bacterial enteric fever like Salmonella enterica, typhi, or paratyphi (18%), and other types of infection (5%).
If a patient has a fever along with significant drowsiness or seizures, viral or bacterial meningitis or meningoencephalitis needs to be considered. In these cases the patient might need to have a lumbar puncture. Some fever-causing viruses include avian influenza, Middle East respiratory syndrome coronavirus, hemorrhagic fever like Ebola virus, Lassa fever, Marburg hemorrhagic fever, Crimean-Congo hemorrhagic fever, yellow fever, dengue, Japanese encephalitis, Rift Valley fever, hepatitis virus (A or B), viral gastroenteritis, and rabies.
Some bacterial causes of fever are anthrax, epidemic typhus, ehrlichiosis, leptospirosis, melioidosis, murine (endemic) typhus, spotted fever group rickettsioses, Q fever, and Yersinia pestis.
In children, the likely cause of fever can vary by region. Most often, it may be a viral or bacterial infection. As per a 2014 study involving children with fever in a tropical region, around 10.5% had malaria, 62% had a respiratory infection, 13.3% had a systemic bacterial infection (usually staphylococcus or streptococcus bacteremia), and 10.3% had gastroenteritis (viral or bacterial). Other conditions like urinary tract infection and typhoid may also be considered. Just like in adults, if the child is unusually drowsy, meningitis should be considered and tested for.
What to expect with Malaria
The length of untreated infection and when it might reoccur can change based on where you are and what kind of species the parasite is. P. falciparum and P. ovale infections can last between 2 to 3 weeks and may come back from 6 to 18 months later, often from a new infection. P. vivax infection can last from 3 to 8 weeks and may come back months or up to 5 years later. P. malariae infection can last from 3 to 24 weeks and may reoccur up to 20 years later.
A relapse means that you feel sick months to years after all the erythrocytic organisms, the main stage during which the parasite grows in your blood, are gone. This can be because of a new infection or because dormant parasites in your body have become active again.
Recrudescence is when you feel sick again within days to weeks of the severe phase of illness because of persevering parasites in your body. This happens because the treatment was not effective or not completed, or your body’s immune system did not successfully fight the parasites. This is more common with P. falciparum.
Getting appropriate treatment generally leads to complete recovery from the illness.
The two essential things that show the outcome for both adults and children are the level of consciousness that doctors can check with coma scales and the degree of metabolic acidosis. Metabolic acidosis is a condition that happens when there’s too much acid in your body. Doctors can assess it by checking your breathing pattern or, more accurately, by measuring the bicarbonate, base deficit, and plasma lactate in your body.
While 10 to 20% of people with severe malaria who get treatment die from it, this number goes up to approximately 50% in pregnant women.
Possible Complications When Diagnosed with Malaria
Malaria carries significant complications. These typically include cerebral malaria, severe malarial anemia, and a kidney disease known as nephrotic syndrome.
Cerebral malaria is responsible for the majority of deadly cases of malaria, usually linked to P. falciparum infection. It typically starts with slow mental degradation, bouts of aggression, headaches, and very high fevers. Afterward, symptoms may escalate to coma, acid build-up in the body, low blood sugar, potential seizures, and in severe cases, death. It mostly affects kids below 5 years old, with nearly a fifth of cases being fatal. The disease develops due to a set of events including red blood cells becoming infected with malaria and clustering together, arteries in the brain dilating, and a host of inflammatory reactions. This leads to a jam of blood cells, the reduction of blood flow in the brain, impaired blood-brain barrier, and an increase in brain size due to water retention.
An increase in brain size is the primary reason for fatality in cerebral malaria cases. In a study conducted in 2015, it was found that of Malawi’s children with cerebral malaria, 84% of those who died displayed highly increased brain size according to MRI scans. Those who survived showed relatively smaller initial brain sizes or decreased sizes over time.
Severe malarial anemia is a result of mechanisms involving TNF-alpha that lead to a decreased production and increased destruction of red blood cells. This can lead to “blackwater fever” where a patient suffers severe anemia, dark-colored urine, and kidney failure as a result of frequent P. falciparum infections treated with chronic quinine; it is considered rare and is believed to be related to a genetic condition (G6PD deficiency).
Nephrotic syndrome is a kidney disease linked to malaria due to the buildup of antigens and antibodies in the kidneys. This can cause decreased kidney function and kidney failure. This condition is common in P. malariae and P. knowlesi infections, possible in P. vivax, and rare in P. falciparum and P. ovale infections.
There are other potential complications associated with malaria, which include:
- Severe fever with abdominal pain and persistent vomiting leading to major dehydration, yellowing of the skin and eyes, and dark urine.
- A condition affecting adrenal gland function leading to their destruction due to congestion of parasites.
- Potential complications like severe breathing difficulties, systemic shutdown, diffusion of microscopic blood clots throughout the blood stream, fluid build-up in the lungs, coma, and death.
Malaria infection during pregnancy may result in the newborn weighing less than normal or, in some cases, the baby not surviving.
Preventing Malaria
If you are planning to travel to a place where malaria is common, it is recommended to visit a doctor who specializes in preventing diseases before you start your trip. The goal of this visit would be to learn more about protecting yourself from malaria. This mainly involves mosquito control and taking special medications when in areas with a lot of mosquitos.
Mosquito control involves preventing mosquito bites by using bed nets treated with insecticides, treating your clothing with a product called permethrin, and applying a chemical called DEET on your skin. There are also certain medicines you can take to help prevent malaria. These medicines include atovaquone-proguanil, doxycycline, and mefloquine.
Atovaquone-proguanil needs to be taken daily during your travel and for one week afterward. It works by preventing the liver stage of malaria. However, this medication is not approved for use during pregnancy. Another medicine, doxycycline, is taken daily during and for one month after your trip. It works by preventing the blood stage of malaria. It has the added benefit of protecting against other diseases like Rickettsial disease, Q fever, leptospirosis, and travelers’ diarrhea. However, it can cause stomach upset, increased sensitivity to sunlight, and a higher risk of yeast infections.
Mefloquine, on the other hand, needs to be taken weekly during and for one month after your travel. It also works by preventing the blood stage of malaria and can be safely used during the second and third trimesters of pregnancy. However, it carries a higher risk of affecting your mental health. The US military mainly uses doxycycline if it works effectively against the type of malaria in the area. Women who are pregnant for the first time or breastfeeding should take either chloroquine or mefloquine, as information on the safety of atovaquone-proguanil during pregnancy is not clear.