What is Periodontal Abscess?
A periodontal abscess, while not as common as an endodontic abscess, is still a frequent dental emergency that needs immediate attention due to the sudden onset of pain. Essentially, a periodontal abscess is when pus builds up within the wall of a periodontal pocket, a space that can form around your teeth if you have gum disease. People who already have these pockets are more likely to develop this kind of abscess. The abscess can develop quickly, damaging the tissues around your teeth and showing very clear symptoms. If many abscesses form around a single tooth, it’s possible that nothing more can be done to save the tooth.
There are two main causes of this kind of abscess: one tied to periodontitis, or gum disease, and one not tied to periodontitis. The former usually happens because of worsening untreated gum disease or during the treatment of gum disease. The latter is often caused by foreign objects getting stuck, like a piece of dental floss, or issues with the root of the tooth itself.
To treat a periodontal abscess, dentists usually first drain the pus, then clean the area thoroughly, often recommending mouth rinses to keep the area clean and deter further infection. In some cases, antibiotics may also be prescribed.
What Causes Periodontal Abscess?
Periodontal abscesses can either be a direct result of gum disease or they can develop on their own without any signs of gum disease.
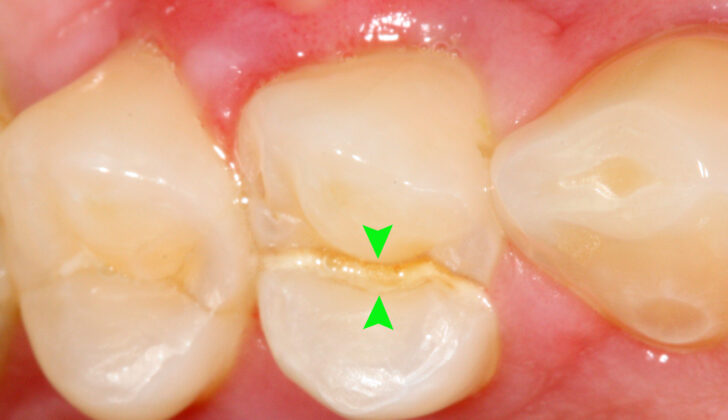
Certain things can increase the risk of getting a periodontal abscess. This includes teeth that have grown into the gum, grooves in the roots of the teeth, cracked teeth, and external root resorption, which is a condition where the body breaks down and absorbs the material that makes up a tooth.
If you have gum disease and are given antibiotics without having the diseased parts cleaned out, this can also cause periodontal abscesses. It’s thought that this happens because the antibiotics cause the bacteria below the gum line to change, leading to what’s called a superinfection.
The type of bacteria found in a periodontal abscess is generally the same as that in gum disease – mainly gram-negative anaerobic bacteria, which are types of bacteria that don’t need oxygen. The most commonly found bacteria in periodontal abscesses is Porphyromonas gingivalis, with it being found in 50 to 100% of all cases. Other bacteria that have been linked with periodontal abscesses include Prevotella intermedia, Prevotella melaninogenica, Fusobacterium nucleatum, Tannerella forsythia, and several others.
Risk Factors and Frequency for Periodontal Abscess
In a study throughout UK dental practices, it was found that the third most common type of mouth infection is the periodontal abscess. This makes up about 6-7% of all cases, following the periapical abscess (14-25%) and pericoronitis (10-11%).
Periodontal abscesses are more common in patients who already suffer from gum pockets. In a long-term study carried out in Nebraska, 51 patients with gum disease were observed over seven years. Out of those, 27 patients wound up with a periodontal abscess. Most of these abscesses formed in teeth that were subjected only to basic superficial cleaning. Some appeared in teeth that had undergone deep cleaning or treatment involving flap surgery.
- 23 abscesses developed in teeth treated with coronal scaling only.
- 3 abscesses developed in teeth that received root planing.
- 1 abscess developed in a tooth that needed treatment with flap surgery.
Of the 27 abscesses, the majority (16) started with probing depths greater than 6 mm.
Another important connection is seen between diabetes and gum disease. It seems that each condition can exacerbate the other. Notably, people who have diabetes might be more prone to developing periodontal abscesses.
Signs and Symptoms of Periodontal Abscess
For a patient suffering from periodontal abscesses, it is vital to inquire about their dental health history, such as if they’ve undergone any dental cleaning or have used antibiotics recently. Situation leading up to an abscess might include leftover tartar, the introduction of bacteria into gum pockets during dental cleanings, or an overgrowth of existing bacteria due to antibiotics. Asking patients about the history of any foreign object getting lodged in their gums could hint towards the cause of the abscess.
It’s also crucial to check the patient’s medical history for signs of diagnosed or undiagnosed diabetes, as this condition makes people more susceptible to developing dental abscesses. The patient usually complains about mouth swelling with or without pain. They might have pain that increases while biting, a loose feeling tooth due to the loss of the gum structure, and sometimes, a sensation of the tooth being raised. Discharge of pus from the gums usually upon probing, causing a bad taste, is often reported by patients.
The physical examination is critical in confirming the diagnosis. Common signs include signs of gum diseases like deep gum pockets, discharge of pus, loose teeth, and involvement of tooth roots. Other symptoms can include tenderness on pressing and hitting the tooth sideways. Clinicians might notice a bulge in the gums at the side of the tooth root. However, abscesses located deep in the gums are less visible. Generally, the tooth responds well to electric or thermal pulp testing as the cause is gum-based, not tooth-based.
Periodontal abscesses are classified based on their location, the duration of infection, and the number of abscesses. Location-wise, they are known as gingival, occurring only at the gum line and between gums, usually due to trapped foreign objects. Periodontal abscesses are deeper and often related to gum diseases, infecting deeper gum pockets and bone defects.
Time-wise, these abscesses are identified as either chronic or acute, each with distinctive symptoms. Acute abscesses cause pain, tenderness upon pressing, and pus formation. In contrast, chronic abscesses are typically tied to a sinus tract and have little or no pain.
Counting the number of abscesses can reveal two cases. Single abscesses are typically due to a local obstruction, and multiple abscesses are linked with systemic illnesses like diabetes or taking antibiotics for non-dental issues while having untreated gum diseases.
Testing for Periodontal Abscess
Periapical radiographs, a type of X-ray that provides a view of the entire tooth from the crown to the root, are key in checking the hard tissues surrounding the tooth. These can often show a widening of the periodontal ligaments (the structures that hold your tooth in place) and loss of bone around the tooth either in a horizontal or vertical direction.
Images might also show a dark area around the end of the tooth root, which usually indicates an endodontic abscess (an infection at the base of a tooth) or a combined periodontal-endodontic abscess, which is an infection that has spread from the gums to the bone at the base of the tooth. This combined abscess often leads to the loss of the bone surrounding the tooth, extending to the area of the infection.
One way for dentists to determine where the infection is originating from is to place a material called gutta-percha along the pathway of infection or into the gum pocket around the tooth. A radiograph can then be used to see where this material ends up.
In certain cases, a test using a high-powered microscope (a Darkfield microscopic examination) might be performed to differentiate between different types of abscesses based on the bacteria present in the infection. Positron Emission Tomography (a type of imaging test) can also be highly accurate in identifying abscesses in the mouth brought about by bacteria that grow in low-oxygen conditions.
Treatment Options for Periodontal Abscess
The treatment of a dental abscess usually happens in two stages: immediate management and long-term treatment after the immediate symptoms have been dealt with. The immediate treatment aims to relieve symptoms and prevent the spread of infection. This is done by draining the abscess, usually by cleaning the root surface via the affected gum pocket, or by making a small cut over the swollen area of the gum. This might require local anesthesia. The cleaning should include the removing of dead tissue and bacteria by scaling the gum pocket and using an antiseptic rinse. This process helps the body’s immune system to combat the infection.
Afterwards, patients are advised to do warm salt water rinses and to drink plenty of fluids to reduce swelling. The dentist will need to reassess the abscess to work out a treatment plan which usually includes gum therapy.
It might be necessary to remove the tooth if it’s severely affected by the abscess due to gum disease or damage caused by the abscess. If the cause of the abscess is a foreign object stuck in the gum or tooth, it needs to be removed by cleaning, and drainage through the gum line should be carried out. A warm saline rinse is then done. A follow-up appointment is usually arranged for one to two days after.
Antibiotics are generally recommended, in addition to mechanical treatment, for patients who have weakened immune systems or where the infection has spread to other parts of the body and caused symptoms like fever, tiredness, skin infection or enlarged lymph nodes. When doctors choose an antibiotic, they should consider the type of bacteria involved, the patient’s allergies, and any potential interactions with other drugs being taken by the patient. The antibiotics amoxicillin and clavulanic acid are often the first choice, and clindamycin may be used for those who are allergic to penicillin.
Patients who have multiple dental abscesses may need to be referred for further testing as this can indicate an underlying health issue like diabetes mellitus.
Surgery may be necessary for chronic dental abscess cases. This can include treatments like a gingivectomy (removal of gum tissue) or flap procedures, which aim to remove any leftover tartar and drain the abscess. These procedures are particularly used in abscesses related to deep vertical defects. Flap procedures have been suggested for abscesses that form after gum treatment, where the tartar is left under the gum line.
What else can Periodontal Abscess be?
A meticulous medical history and examination are important in distinguishing different mouth diseases. Here are some that could be mistaken for each other:
- Periapical abscess: This condition might be indicated by a history of tooth damage, wear, breakage, cavities, or deep repairs. Tooth tests with electric or heat stimulation could provide unclear or negative results. X-rays might show a dark area at the tip of the root if the patient has an intense flare-up of a chronic periapical lesion.
- Combined abscesses of tissues surrounding tooth root and within tooth: These can be categorized by the origin of the infection and can either be primarily from inside the tooth with secondary involvement in the surrounding tissues, primarily in the surrounding tissues with secondary involvement in the tooth’s interior, or a true combination. The correct diagnosis depends on a thorough history, examination, tooth tests, and x-rays. If the tooth tests show a positive result, it suggests the infection began in the surrounding tissues, a lack of response suggests it started inside the tooth.
- Pericoronal abscess: Abscesses from a tooth that’s partially emerged can often copycat a gum abscess. Doctors should check for healthy neighboring teeth with no increased gum pockets.
- Partial root fracture: These fractures can be spotted through visual inspection, increased movement, and soreness. X-rays from different angles can also help identify fractures. Any holes caused by tooth marrow treatments or holes resulting from tooth restorations can also be identified through x-rays.
- Squamous cell carcinoma: Doctors should be careful when examining and treating recurrent gum abscesses as there are instances where gum cancers copycat gum disease and its associated abscesses.
- Self-inflicted gum injuries: Habits like nail-biting and damage from items, such as pens and pins, can cause similar-looking lesions. A full history can rule this out and methods to deter these habits may need to be considered.
- Other less common differentials include a type of cyst linked to the tooth root, post-surgery infection, a type of benign tumor originating from teeth, cancer that’s spread from other parts of the body, a type of cancer affecting lymphocytes, a common benign skin lesion, bone infection, a type of benign jaw lesion, a type of benign tumor consisting of eosinophils, and an abscess that develops after surgery.
What to expect with Periodontal Abscess
Periodontal abscesses, a type of gum infection, can cause fast damage to the tissue that holds your teeth (periodontal ligament) and the bone that surrounds your teeth (alveolar bone). This kind of swift destruction can seriously affect a tooth’s survival chance, possibly leading to tooth loss. It’s especially problematic for individuals already dealing with moderate to severe loss of the tissue or “attachment” that keeps their teeth in place.
In a study looking back at tooth loss due to periodontal abscesses, it was found that nearly half of the teeth affected by this type of gum infection had to be extracted or removed during supportive treatments. Around half of them were successfully kept in place for an average of 12.5 years. Teeth experiencing furcation involvement—a condition where the areas of the tooth where the roots split become diseased—were more likely to be extracted compared to teeth without this issue.
In the case of teeth with continuous abscess formations, the outlook tends to be quite poor. The research points to worse results for teeth already wrestling with existing periodontal disease. Due to the speedy harmful effects of this disease, early detection and management are vital to improve the tooth’s chances of survival.
Possible Complications When Diagnosed with Periodontal Abscess
If a dental abscess is not treated, it can damage the supporting structure of the tooth, making the tooth’s future health less optimistic. This is especially important for people who have moderate to severe gum diseases. Often, teeth with gum abscesses may need to be pulled out in the future due to recurrent abscesses, pain, or increased tooth mobility. If left untreated, these gum abscesses can spread infection throughout the body. They can grow into swelling in the head and neck, cause enlarged lymph nodes, and even lead to sepsis, a life-threatening infection.
Common Consequences:
- Damage to the tooth’s supporting structure
- Removal of the tooth due to recurrent abscesses, pain, or increased tooth mobility
- Spreading infection throughout the body
- Swelling in the head and neck
- Enlarged lymph nodes
- Potential development of sepsis
Preventing Periodontal Abscess
It’s crucial that patients understand the key risks that can contribute to the development of periodontal abscesses – pus-filled sacs in the gums. Here’s what to know:
1. Dental cleanliness is key: Brushing your teeth twice a day along the edges of your gums and flossing or using other tools to clean between your teeth can help control the buildup of plaque and bacteria.
2. Controlling diabetes: Patients should understand that there is a two-way link between gum disease and diabetes – this means that controlling your diabetes can also help prevent gum disease. It can be helpful to coordinate with your general doctor to manage this.
3. Stop smoking: Advising patients to quit smoking can significantly lower their risk of gum disease, mouth cancer, and overall health. Also, being aware of a family history of gum disease (though it can’t be changed) can encourage patients to maintain good dental hygiene and seek dental care early and more often.