What is Pneumocystis jirovecii Pneumonia?
Pneumocystis carinii pneumonia (PCP), now called Pneumocystis jirovecii
pneumonia, is a type of fungal infection that typically affect individuals with weaker immune systems. In severe instances, this infection can pose a real threat to life. Usually, individuals at high risk for PCP are those whose immune systems are compromised due to certain medical conditions, like cancer, HIV, organ transplant recipients, or people taking certain medical treatments that could suppress their immunity. Symptoms of this infection may include fever, cough, shortness of breath, and in critical cases, respiratory failure or difficulties in breathing.
PCP is believed to spread between people through the air. Interestingly, people with healthy immune systems can carry this fungus in their lungs without showing any symptoms, making them unintentional carriers. This means they can unknowingly spread the fungus to individuals with weaker immune systems. While this infection remains the most common and serious lung infection in individuals with AIDS, preventive measures and the use of antiretroviral therapy (anti-HIV medicine) have helped greatly reduce its occurrence.
What Causes Pneumocystis jirovecii Pneumonia?
Pneumocystis was initially believed to belong to a group of microorganisms known as protozoans. However, in 1988, it was re-categorized as an ascomycetous fungus, another kind of microorganism. Just to clarify, a protozoan is a single-celled organism that can cause various diseases in humans, while a fungus is a type of multi-cellular organism that includes mushrooms, yeast, and mold.
The categorization of Pneumocystis was a topic of discussion for a long time because its life cycle – the sequential series of changes undergone by an organism – resembled both a protozoan’s and a fungus’s.
To resolve this, researchers conducted detailed studies comparing this organism to others from plant, animal, fungi, and protozoan groups. They did this using something called ‘phylogenetic analysis’ of small subunit ribosomal ribonucleic acids. In simpler terms, they compared the genetic material of these organisms to understand how they are related.
After considering different factors such as the composition of the cell wall, the structure of important enzymes, and gene sequencing (the process of determining the exact order of the bases in a strand of DNA), they concluded with certainty that Pneumocystis is indeed a member of the fungi family.
Pneumocystis is a diverse genus – a group in biological classification – and includes several species. Among these are Pneumocystis carinii, which affects rats, and Pneumocystis jirovecii, which affects humans.
Risk Factors and Frequency for Pneumocystis jirovecii Pneumonia
Pneumocystis, a cause of pneumonia, first became prominent in Europe following World War II, particularly amongst premature and malnourished infants in orphanages. During the HIV (Human Immunodeficiency Virus) epidemic in the 1980s, more research was conducted on this organism. Today, it is known to affect patients globally and is transmitted from person to person through the air. Pneumocystis pneumonia (PCP) is mainly seen in individuals with weakened immune systems and is quite rare in those with fully functioning immune systems. Certain groups of people carry a higher risk of developing PCP.
- People suffering from cancer, especially blood-related malignancies.
- People who have undergone transplants, either of hematopoietic cells or solid organs.
- People undergoing treatment for certain inflammatory or rheumatologic conditions.
- People with any condition that results in defects in cell-mediated immunity.
The highest risk factor for PCP in patients without HIV is the use of glucocorticoids alongside immunosuppressive therapy. It has been found that 91% of first-time PCP patients had used glucocorticoids within a month of infection. PCP is prevalent amongst individuals infected with HIV and is often seen as an illness that defines the progression to AIDS (Acquired Immune Deficiency Syndrome).
At the start of the HIV epidemic, infection rates were as high as 20 in 100 people with CD4+ counts of less than 200 cells/µL. Since the introduction of primary prophylaxis and antiretroviral therapy in 1989, rates of PCP have been decreasing annually. For example, between 1992 and 1995, the rate of decrease was 3.4% per year and 21.5% per year between 1996 and 1998.
A 2016 study of HIV-infected people saw the incidence rate of PCP per 1000 person-years reduce from 29.9 in 1994-1997, to 7.7 in 1998-2002, and further to 3.9 in 2003-2007. Despite the significant reduction in the infection rate in the United States and other industrialized countries, PCP remains a leading cause of serious infection in those with weakened immune systems.
Signs and Symptoms of Pneumocystis jirovecii Pneumonia
Patients diagnosed with PCP, or Pneumocystis pneumonia, may show various signs of illness which are subtle or easily recognizable. This condition commonly affects patients with HIV, and they may display a gradual onset of symptoms like a dry cough, low-grade fever, and progressive difficulty in breathing. These symptoms usually develop over a few weeks. Non-HIV patients may experience similar symptoms, but these often progress more rapidly and can be accompanied by severe breathing difficulties.
Given that PCP is frequently linked to weakened immune systems, it becomes crucial to assess the patient for any underlying causes of immune deficiency. Recognizing their risk of contracting opportunistic infections like PCP helps in their treatment. History of HIV infection, current HIV treatments, and indications of an undiagnosed HIV infection such as fatigue, weight loss, muscle/joint pain, skin rash, and headache are important information to gather. It’s also essential to know if the patient has recently been on steroids or any other immune-suppressing therapies.
During physical assessment, no unique signs directly point to a Pneumocystis infection; however, certain findings suggest a respiratory infection such as pneumonia. You may hear crackling and dry, rattling sounds in the lungs, or you may notice faster, shallower breathing and increased heartbeat. Patients commonly present with a fever, and in cases of HIV patients, an oral yeast infection. Therefore, it’s recommended to conduct a thorough examination to look for any other signs that may indicate an underlying immune problem. In patients with HIV, shortness of breath during exertion, increased white blood cell count, and oral thrush is more likely to suggest PCP than other lung infections such as tuberculosis or bacterial pneumonia.
Testing for Pneumocystis jirovecii Pneumonia
To make a diagnosis of PCP, a type of lung infection, a doctor considers various aspects including the patient’s risk factors, lab results, and results from different types of imaging studies such as chest X-rays and CT scans. Doctors may also test sputum (the mixture of saliva and mucus coughed up from the lungs), bronchoalveolar lavage fluid (a sample of cells and other components from the lungs), or in some cases, conduct lung biopsies.
One typical laboratory test involves checking for levels of a protein called lactate dehydrogenase (LDH). If the level is high in patients with HIV, it might mean they have a PCP infection. However, for individuals with weak immune systems not due to HIV, raised LDH levels might not necessarily indicate PCP.
Another key substance tested for is beta-D-glucagon, found in the cell walls of most fungi, including Pneumocystis which causes PCP. If someone with risk factors for pneumonia is showing clinical signs and also has high beta-D-glucagon levels, PCP might be suspected and further tests initiated.
For people who have fast heartbeat, difficulty breathing, and low oxygen levels, an arterial blood gas test might be conducted to measure the oxygen level in the blood and assess disease severity. Patients with PCP often show an increased alveolar–arterial oxygen gradient, which indicates that oxygen isn’t moving from the lungs to the blood as it should be.
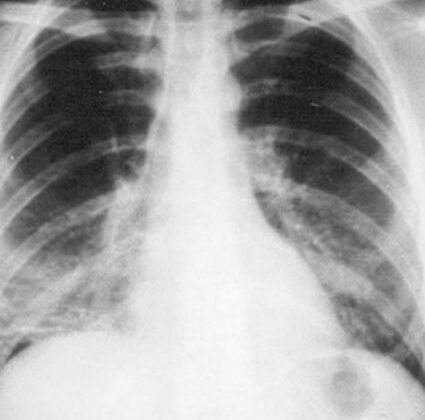
A chest X-ray can also be useful in diagnosing PCP, usually showing diffuse (spread out) bilateral (both sides involved) infiltrates (substances that have passed into the lungs) around the hilus (part of the lung where blood vessels and airways enter and exit). As the disease progresses, these infiltrates become more homogeneous or evenly spread. Other findings can also be indicative of PCP, including specific types of nodules or lobar infiltrates (spread-out substances in a lobe of the lung).
If PCP is suspected and the chest X-ray is negative, a chest CT scan might be done to look for certain changes, such as a ground-glass appearance or cystic lesions, which indicate damage to the lung tissue.
Pneumocystis, the fungus causing PCP, can’t be grown in a lab, so the disease is confirmed by looking for the actual organism in respiratory specimens such as sputum or bronchoalveolar lavage fluid. The organism can be identified using techniques like polymerase chain reaction assays (a test to detect genetic material of the disease-causing organism), dye staining, or fluorescein antibody staining (which identifies the organism by its reaction with a specific stain). However, these tests can only be done if the patient is stable and if obtaining the samples is not dangerous.
Sometimes a definitive diagnosis of PCP isn’t possible. For instance, HIV/AIDS patients might have more organisms in their samples, which makes diagnosing easier, while immunocompromised patients without HIV might have fewer organisms, making diagnosis tricky. Regardless, if PCP is suspected in high-risk patients, the doctor will treat them accordingly, even if a definitive diagnosis hasn’t been made.
Treatment Options for Pneumocystis jirovecii Pneumonia
If you are suspected to have Pneumocystis pneumonia (PCP), a type of lung infection, doctors won’t wait for test results to start treatment, especially if you have known risk factors or if your symptoms point to infection. Treatments for PCP have been largely studied in patients with HIV, but also apply to those without HIV.
The most effective treatment for PCP is a combined antibiotic known as trimethoprim-sulfamethoxazole (TMP-SMX), typically given for 21 days. If your case is mild, this can often be taken orally, unless you are unable to tolerate oral medications or your condition is severe. If a patient is allergic to TMP-SMX, but the allergy isn’t severe, doctors may recommend trying a slow introduction to the medicine. If the allergy is severe, other medications will be used instead.
For patients with sulfa allergies (allergic to TMP-SMX), there are alternatives for mild to moderate cases. These include atavaquone, taken orally with food, or a combination of other antibiotics such as trimethoprim with dapsone, or primaquine with clindamycin.
If PCP is severe, it might be necessary to use pentamidine, given intravenously, or a combination of primaquine and clindamycin. It’s important to note that patients who are unable to take oral medications can have intravenous pentamidine, but should be treated with care due to the potential side effects. Also, those with a deficiency known as glucose-6-phosphate dehydrogenase should be cautious if using dapsone or primaquine, as these can increase the risk of a certain type of anemia.
Glucocorticoids, a type of steroid, may also be used in treatment to improve clinical outcomes. This often applies to HIV-infected patients, especially if they have particular blood oxygen levels, or to those without HIV due to the potential severity of the illness.
For certain patients with immune system issues, such as those undergoing certain cancer treatments or organ transplants, preventative treatment, or “prophylaxis”, against PCP might be advised. The first choice for this preventative treatment is usually TMP-SMX. Alternative treatment options can be used for those with sulfa allergies, such as dapsone or atavaquone. Prophylaxis is usually unnecessary for patients taking pyrimethamine-sulfadiazine.
In patients with HIV, preventative treatments are recommended when certain markers in the blood are below standard levels. Likewise, pregnant patients should still receive preventative treatment for PCP, but some medications should be avoided during the first trimester due to potential risk for the unborn baby.
The success of the treatment can depend on several factors, including the severity of the disease and the presence of other infections. Regular monitoring is important to check that the treatment is working, and adjustments may be made if improvements are not observed within a certain timeframe. During all phases of treatment, it’s important to also look for and treat any other infections that may be contributing to the illness.
What else can Pneumocystis jirovecii Pneumonia be?
When a doctor is trying to determine if a patient has Pneumocystis jiroveci pneumonia, they’ll consider other health problems that have similar symptoms. These could include:
- Acute respiratory distress syndrome (a severe lung condition)
- Viral or bacterial pneumonia
- Tuberculosis (a lung disease caused by bacteria)
- Legionella pneumonia (a type of pneumonia caused by legionella bacteria)
- Mycoplasma infections (infections caused by a type of bacteria)
- COVID-19 pneumonia (a severe lung infection caused by the COVID-19 virus)
What to expect with Pneumocystis jirovecii Pneumonia
While most patients get better with suitable treatment, some unfortunately experience failure of their respiratory system. Among patients needing intense care or help breathing through a ventilator, the mortality rate can go as high as 60%. On a more positive note, patients with mild to moderate disease tend to fare better, with a fatality rate of less than 10%. However, for patients suffering from severe conditions, this rate increases to more than 20%
For patients who have HIV, there are certain factors that imply a less favorable recovery. These include being older, having a previous instance of PCP (a type of lung infection), the presence of the cytomegalovirus in fluid from their lungs, a high concentration of a particular enzyme in the blood known as lactate dehydrogenase, and a low count of CD4 cells which are a type of white blood cell that helps the immune system function.
Possible Complications When Diagnosed with Pneumocystis jirovecii Pneumonia
Pneumocystis jiroveci pneumonia can lead to a variety of complications, such as:
- Swelling of lymph nodes (Lymphadenopathy)
- Involvement of the bone marrow leading to severe decrease in red and white blood cells and platelets (pancytopenia)
- Affecting the digestive tract and thyroid gland
- Severe lung condition causing shortness of breath (Acute respiratory distress syndrome)
- Unable to breathe adequately (Respiratory failure)
Preventing Pneumocystis jirovecii Pneumonia
Patients who have previously been diagnosed with HIV should receive in-depth education about the progression of their disease and how certain cell count levels might necessitate preventative treatment. For those patients being cared for outside of a hospital, it’s important for them to know that if their symptoms get worse, or if they don’t notice any improvement after 4 to 7 days, they might need treatment through an IV (a tube inserted into the vein used for delivering medication). In such cases, they should return for a follow-up visit.