What is Pott Disease?
Tuberculosis (TB), a disease that affects the lungs, has been known since ancient times. It was first described between 1000 to 600 BCE as “Yakshama” in ancient Indian medical texts, as well as the Sushruta Samhita and Charaka Samhita. In 1779, Sir Percival Pott described a form of tuberculosis that affected the spine and caused a hunchback condition and neurological problems in European patients.
Throughout the 19th and 20th centuries, significant progress was made in diagnosing and treating tuberculosis. Scientists discovered the bacteria that cause the disease, known as Mycobacterium tuberculosis, they developed a vaccine called Bacillus Calmette-Guerin (BCG), and they made significant advancements in diagnostic tests and treatments, including surgical procedures. These advancements have greatly improved our ability to manage and treat tuberculosis, providing better protection against this serious illness.
However, tuberculosis has been making a comeback in developed countries, especially among people with weakened immune systems due to mass migration. This has presented a significant challenge worldwide. There’s also been a rise in cases of tuberculosis caused by bacterial strains resistant to multiple drugs in developing countries over the past few years. For these reasons, tuberculosis remains a major threat to public health globally.
What Causes Pott Disease?
Tuberculosis, often shortened to TB, is caused by bacteria from the Mycobacterium family. There are about 60 different types of these bacteria, but the one we usually see in TB is called M. tuberculosis. This type of bacteria is tricky because it grows slowly and likes areas with lots of air. There are other types of Mycobacterium bacteria that can affect humans like M. avium, M. bovis, M. microti, and M. africanum, but they are less commonly the cause of tuberculosis.
An interesting thing about TB bacteria is that they can lie dormant or “sleep” for a long time. But when conditions become favorable again, they wake up and start multiplying, usually around once every 15 to 20 hours.
Once someone is infected, the body’s response is to create a unique type of inflammation called a granuloma. This inflammation involves forming a mass made up of certain types of immune cells.
There are a few things that make someone more likely to get TB. These include being exposed to someone else with TB for a long period of time, having a weakened immune system (like in HIV, alcohol abuse, or drug abuse), living in crowded conditions, not getting enough to eat, living in poverty, and being in a lower socio-economic situation.
Risk Factors and Frequency for Pott Disease
Extrapulmonary TB (EPTB), a form of tuberculosis that affects areas outside of the lungs, makes up 3% of TB cases. Of these, 10% are cases of skeletal TB, and half of these affect the spine. According to data from the World Health Organization (WHO), 2016 saw 10.4 million new cases globally. Nearly half of these cases were found in South East Asia, with India accounting for 23% of all TB cases worldwide. Interestingly, the number of people moving between countries has risen from 173 to 244 million between 2000 and 2015. This increase in global movement has led to a resurgence of TB, even in developed countries.
- Extrapulmonary TB (EPTB) makes up 3% of all TB cases.
- Of EPTB cases, 10% are skeletal TB, with half of these being Spinal TB.
- The World Health Organization (WHO) reported 10.4 million new TB cases in 2016.
- Nearly half, or 46.5%, of the 2016 cases were in the South East Asia region.
- India accounted for 23% of global TB cases.
- The number of international migrants increased from 173 million to 244 million between 2000 and 2015.
- This rise in immigration is contributing to a resurgence of TB, even in developed countries.
Signs and Symptoms of Pott Disease
Spinal tuberculosis can cause various symptoms that depend on factors such as how severe the condition is, how long the person has been ill, and where the disease is in the spine. Symptoms can also vary depending on whether or not there are complications from the disease such as deformity and neurological deficits. For uncomplicated cases, patients typically experience back pain. Complicated cases often cause deformity, instability, and neurological problems. The back pain can be the result of an active tuberculosis infection (due to inflammation), destruction of bone, or instability in the spine. If the patient has bacteria present but is not showing signs of the disease, this is known as latent tuberculosis.
The term ‘cold abscess’ refers to an abscess that does not show clear signs of inflammation. In cases involving the cervical spine, these abscesses may be found in the retropharyngeal space, neck or axilla, among other spaces. They may present as pre- or paravertebral abscesses, or over the chest wall in cases involving the thoracic spine. In the lumbar spine, they may be located along the psoas muscle, and other regions.
Deformity caused by spinal tuberculosis can be classified into three main types: ‘knuckle’ for the involvement of one vertebra, ‘gibus’ for two vertebrae, and ’rounded kyphus’ for more than three vertebrae. These deformities are caused by the anterior column of the spine being more affected by tuberculosis, leading to an increasing kyphotic orientation, especially in the thoracic and thoracolumbar spine. Certain formulas have been proposed to predict the final kyphosis, a spinal disorder in which an excessive outward curve of the spine results in an abnormal rounding of the upper back. Correcting spinal deformity could significantly improve quality of life and prevent or decrease neurologic complications.
Neurological deficits caused by spinal TB can occur at both the active stage of the disease, due to compression, or during the healed stage. Initial compression in TB can lead to anterior spinal tract involvement and UMN-type motor deficit. Subsequently, the lateral spinal tracts and posterior column may be involved, leading to loss of crude touch, pain, temperature, and complete sensory loss.
- Stage 1: Deficit is only evident upon clinical examination
- Stage 2: The patient has UMN-type motor deficit with spasticity, but is still able to walk
- Stage 3: The patient is bedridden and spastic
- Stage 4: The patient is bedridden with severe sensory loss or pressure sores
- Stage 5: Similar to stage 4, but may also include bladder or bowel involvement, flexor spasms, or flaccid tetraplegia/paraplegia
Children, given their physical immaturity and greater flexibility of the spine, are more susceptible to severe deformation. It is recommended to continue monitoring children with Spinal TB until they reach skeletal maturity.
Atypical presentations of spinal TB can include disc prolapse, isolated abscess without skeletal involvement, pure intraspinal granulomas, skip lesions, concentric vertebral collapse, circumferential vertebral involvement, isolated posterior arch involvement, and isolated meningeal, neural or perineural involvement without any vertebral destruction.
Testing for Pott Disease
Tuberculosis or TB can be tricky to diagnose because its bacterium, Mycobacterium TB, doesn’t grow easily. Usually, doctors have to use a variety of lab tests and methods to properly diagnose the disease. These methods may include lab tests that check for the presence of certain immune cells, inflammation markers, and other molecular signs of TB. Doctors often have to combine the information from these lab tests with the patient’s symptoms and results from imaging tests to make a diagnosis.
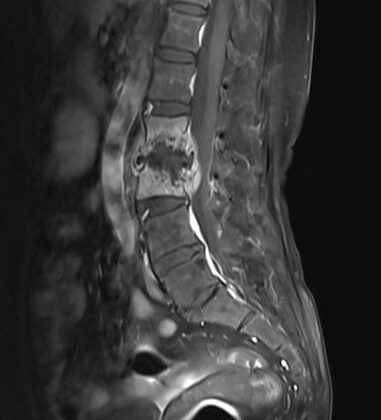
Imaging tests can include X-rays, CT scans, or MRIs. For example, an early-stage TB infection may not show up on an X-ray, but in later stages, the infection can cause specific changes in the spine that can be seen in these images. CT scans are very accurate at detecting these changes early in the disease. MRIs are especially helpful at showing how much the disease has spread into soft tissues and any abscesses that may have formed. Lastly, scans using a method called nuclear imaging can show how active the infection is in certain tissues. Unfortunately, none of these imaging methods can tell the difference between a TB infection and a cancer infection.
Among lab tests, the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are tests that measure inflammation in your body, which is often high during a TB infection. However, these tests alone are not very accurate. There are also tests to measure specific immune reactions to the TB bacterium, but these can’t tell the difference between current and past TB infections. A more accurate lab test is one that checks for acid-fast bacilli (AFB), which will appear red under a specific stain. However, it needs a high concentration of bacteria to be detectable.
Cultures of sputum or other samples are often used to grow and identify TB bacteria, but they can take up to 6 weeks to show results. A faster method is the molecular test or polymerase chain reaction (PCR) which can give results in a few hours and only requires a small number of bacteria. The Gene Xpert MTB/RIF is a version of this test that can also tell if the TB bacterium is resistant to the drug rifampicin.
Finally, looking at tissue samples under a microscope can help diagnose TB by identifying certain distinctive features of the bacteria. However, this test is not 100% accurate.
There are also tests that can detect latent TB, meaning a TB infection that is present but not causing any symptoms. One is the Mantoux test, in which a little TB protein is injected under the skin to see if an immune reaction occurs. However, this test is not highly accurate. There is also the interferon-gamma release assay, which measures the immune response to TB proteins, but this is also not useful in areas where TB is common.
Treatment Options for Pott Disease
Spinal tuberculosis (TB) can be classified into two types: uncomplicated and complicated. Uncomplicated spinal TB is generally treated with medicine, while complicated cases often require a combination of medication and surgery for effective treatment.
Medication, or chemotherapy, is the primary treatment for spinal TB. This involves the use of multiple drugs to fight the TB bacteria in its different stages or forms and to avoid resistance to any one drug. The medications are usually taken over a period of several months. Depending on the specifics of the TB infection, doctors might even recommend taking these drugs daily or every other day. The World Health Organization (WHO) and other health organizations recommend different combinations and durations of TB medications to achieve the best outcomes. If the first-choice (or “first-line”) medications are not effective or cause side effects, other “second-line” drugs can be used as alternatives.
A particular challenge in treating TB is drug-resistance. Multidrug-resistant TB (MDR-TB) is when the TB bacteria are resistant to at least two key TB drugs. Extensively drug-resistant TB (XDR-TB) is a more severe form of MDR-TB, involving resistance to several TB drugs, including both first- and second-line drugs. Extreme cases have also been classified as “totally drug-resistant” TB, where the TB bacteria are resistant to all known TB drugs.
In addition to medication, severe cases of spinal TB often require surgical treatment. Surgery may be needed for several reasons, such as lack of response to medication, recurrent disease, severe weakness, significant spinal deformity, debilitating pain, or instability of the spine. The goals of surgery are to drain abscesses (pockets of infection), remove infected tissues, stabilize the spine, and correct deformities.
Several different surgical approaches can be used to treat spinal TB. In some cases, a “front” or anterior approach is taken, where the surgeon operates on the spine from the front of the body. In other cases, a “back” or posterior approach is taken, where the surgeon operates on the spine from the back of the body. Sometimes, a combined approach is needed and the surgeon operates from both the front and back of the body. Minimally invasive procedures, which involve small incisions and specialized instruments, are also employed to treat spinal TB.
Even after TB has been successfully treated, surgery may still be needed in some cases. For example, patients with severe spinal deformities or instability might need a surgical intervention to correct these issues. The decision to perform surgery depends on several factors, such as the patient’s age, overall health, the severity and location of the spinal problem, and the doctor’s preference.
What else can Pott Disease be?
When doctors are trying to diagnose specific conditions, they need to weed out other situations that might seem similar. We call these alternatives ‘Radiological Differentials’ and ‘Differentials Based on Pathological Appearance’. Here are some examples:
Radiological Differentials
- Pyogenic and fungal infections
- Neoplastic conditions – These include both benign and malignant (cancerous) conditions, including primary tumors and spine metastases. Generally, spine metastases and primary spine cancers mostly affect the vertebral body (bones of the spine) while sparing the disc space. This differs from tuberculosis (TB) and other infections. Tuberculosis also often comes with soft tissue and surrounding abscesses, unlike most malignant tumors.
Differentials Based on Pathological Appearance
- Other conditions which are infections that form granulomas (masses) and might be mistaken for Tuberculosis. These include:
- Atypical bacteria like Actinomyces israelii, Nocardia asteroids, Brucella
- Fungi such as Coccidioides immitis, Blastomyces dermatitidis, Cryptococcus neoformans, Aspergillosis
- Spirochetes: Treponema pallidum which cause diseases like Syphilis
- There are other diseases that show non-caseating granulomas (masses without dead tissue) including Sarcoidosis, Wegener’s granulomatosis, Crohn’s disease, and leprosy.
What to expect with Pott Disease
The prognosis (or expected outcome) of Pott Spine — a form of spinal tuberculosis — is often divided into five stages characterized by changes in the spine’s shape and degree of damage:
* Stage I: Predestructive stage, when your spine is straighter than it should be, and there’s swelling or inflammation around the backbone (Lasts less than 3 months).
* Stage II: Early destructive stage, characterized by less space between the disks in your spine, and slight curving of the spine less than 10 degrees (Lasts 2 to 4 months).
* Stage III: Mild angular curving of the spine (Kyphosis); 2 to 3 vertebrae are involved and the curve is between 10 and 30 degrees (Lasts 3 to 9 months).
* Stage IV: Moderate angular curving of the spine (Kyphosis); 2 to 3 vertebrae are involved and the curve is between 30 and 60 degrees (Lasts 6 to 24 months).
* Stage V: Severe angular curving of the spine (Kyphosis); more than 3 vertebrae are involved and the curve is greater than 60 degrees (Lasts more than 24 months).
The sooner this condition is diagnosed and treated, the better the outcome may be. Complicated cases of Pott Spine (i.e., those associated with deformity, instability, or neurological deficit) have poorer outcomes compared to simpler ones.
Other factors affecting the outcome include age (older or younger age tends to have worse outcomes), weakened immune systems (e.g., HIV, alcohol, drug abuse), overcrowded living conditions, malnutrition, low income, and lower social status. Problems with medication compliance and tolerance can also lead to worse outcomes.
Poor outcomes are also more likely if the disease has spread widely across the vertebral column, if neurological symptoms have been present for a long time, or if they quickly worsened, and depending on the severity of the symptoms and the cause of compression in the spine.
Likewise, the risk of progression in deformity is higher if the patient is younger than 10 years, if the spinal curve is more than 30 degrees, if more vertebrae are affected, if one and a half vertebral bodies or more are lost, or if there’s evidence of instability in the spine.
Possible Complications When Diagnosed with Pott Disease
The effect of a treatment can hinge on several factors. These may include how the disease presents itself (with or without complications), individual outlooks based on clinical assessments and imaging, a patient’s adherence to their prescribed chemotherapy, the progression of the disease, and resistance to medications. Other personal considerations, like socio-economic circumstances, general health condition, and feeding habits, also play a crucial role.
Below are key complications and side effects that may arise:
- Abscesses: swollen areas within body tissue containing an accumulation of pus.
- Neuro deficits: limitations in the functioning of the nervous system.
- Spinal instability: a loss of spine’s natural ability to maintain its alignment.
- Spinal deformity (kyphosis): a curve in the spine causing a hunchback or slouching posture.
- Systemic TB disease: tuberculosis affecting the entire body.
Preventing Pott Disease
Educating patients is crucial when dealing with Tuberculosis (TB), both for individual patients and for the community’s wellbeing. It’s vital to understand that patients who can spread the disease need to be kept away from others. Even though TB that affects other body parts (like the spine) isn’t usually infectious, there’s a chance that it could still affect the lungs in some patients.
Patients need to understand the importance of following their prescribed medication schedule for a long period to completely get rid of the infection. A method named directly observed therapy could make it easier for TB patients to stick to their medication schedules. Wearing correct supportive braces can also lessen the spinal curvature changes in patients that are not treated with surgery.
For children with TB, parents should know that the disease could still cause changes to the body even after the infection seems to have healed. Children need to have regular check-ups till they are fully grown to monitor this.