What is Schistosomiasis?
Schistosomiasis, also known traditionally as bilharzia, is a disease caused by parasitic worms from the Schistosoma species. It’s estimated that this disease affects around 230 million people worldwide, with a further 700 million people being at risk. The three main types of this worm that affect humans are Schistosoma japonicum, S. haematobium, and S. mansoni. These worms cause two main forms of schistosomiasis: one affects the intestines and the other affects the urinary and reproductive systems.
Schistosoma haematobium causes the type of schistosomiasis that affects the urinary and reproductive systems. The name comes from a symptom of the disease – bloody urine. This specific worm is known to cause bladder cancer, making it the second biggest cause of this type of cancer globally. It’s also known to contribute to infertility and increases the risk of getting HIV. But, it often goes undiagnosed.
Schistosoma haematobium is common in certain parts of Africa and the Middle East. These parasites have a complicated life cycle that involves both snails and humans. They spread when people come into contact with contaminated water in areas where this disease is common, making it hard to control and get rid of.
What Causes Schistosomiasis?
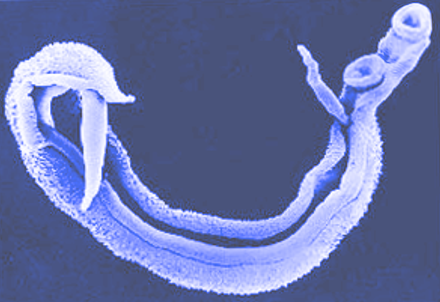
Schistosoma haematobium is a type of tiny parasite (a blood fluke) which belongs to a group called the trematode. This group is part of the larger Digenea subclass.
This specific parasite closely associates with the veins around the bladder and other related reproductive organs. Its lifecycle is pretty complicated. It involves two hosts – a snail species called Bulinus that lives in freshwater areas, and a main host which is usually a human.
The places where this parasite can be found are determined by where these specific snails live. Therefore, occurrence of the diseases caused by this parasite, like schistosomiasis, are also bound by the areas these snails inhabit.
Risk Factors and Frequency for Schistosomiasis
Schistosomiasis is a disease that affects many countries. According to the World Health Organization (WHO), out of the 78 countries that report schistosomiasis cases, it’s a recurring problem in 52. This disease had a lower mortality rate of 0.3 for every 100,000 people in 2016. There was a significant decrease in deaths from 55,000 in 2000 to 24,000 in 2016.
The most common type of this disease affects the urinary and genital organs, and it is caused by a specific species called Schistosoma haematobium. This species is most commonly found in sub-Saharan Africa and parts of the Middle East, particularly in tropical and subtropical areas. The disease frequently impacts communities that lack safe drinking water and proper sanitation.
The chronic version of urogenital schistosomiasis is most common, while the acute form, also known as Katayama fever, is not as widely recognized. In affected areas, people usually get their first infection around the age of 2, and the number of worms in the body typically increases for the next 10 years. The disease is most common in children aged 5 to 14 years in regions like Kenya, likely because of their frequent contact with water. Adults who frequently come in contact with water due to their daily activities also often remain infected.
In areas where the disease is endemic, almost every person tests positive for the infection. Statistics show that 60% to 80% of school-age children and 20% to 40% of adults remain actively infected. In these regions, up to 65% of patients diagnosed with a specific type of bladder cancer, squamous cell carcinoma, were found to have urogenital schistosomiasis concomitantly.
Signs and Symptoms of Schistosomiasis
Urogenital schistosomiasis is a condition that you should consider if you live in or have traveled to places where it is common and experience symptoms like painful or bloody urination, trouble urinating, abnormal vaginal discharge, or pain or bleeding after sex. Men may also notice blood in their semen.
Acute cases of schistosomiasis are less common but are more likely to happen in travelers who haven’t built up immunity. Symptoms don’t usually point directly to the disease and can include stomach issues, fever, fatigue, or trouble breathing. It’s a good idea for anyone returning from areas where the disease is common to get checked out because about 25% of people who don’t show symptoms still develop chronic schistosomiasis.
If you don’t receive treatment for about 3 to 4 months, you could start having trouble urinating or bloody urine due to sores and inflammation in your bladder and urinary tract. Over time, inflammation and egg deposits from the disease can lead to growths and “sandy patches,” which are egg deposits that look like sand, that are visible during medical exams. The disease can get worse and cause fibrosis (scar tissue) and calcification in the bladder wall, which can lead to blockage, bacterial infection, and bladder cancer.
The number of worms in your body depends on how many times you’ve been exposed and how many cercariae (larval stage of the worm) were present each time. This puts women who take care of household chores like clothes washing in areas where the disease is common at higher risk for increased infection rates and severe disease.
- Severe pain during urination
- Bloody urination
- Trouble urinating
- Abnormal vaginal discharge
- Pain or bleeding after sex
- Blood in semen
About 75% of women affected by S. haematobium, a type of schistosomiasis, experience involvement of the genital tract, a condition known as female genital schistosomiasis (FGS). FGS happens when schistosome eggs deposit in the genital tract, causing bleeding, abnormal blood vessels, and “sandy patches” on the vulva, perineum, or cervix. For women who could get pregnant, FGS is a leading cause of miscarriage, ectopic pregnancy, painful or irregular menstruation, and bleeding between periods, as well as low birth weight and poor birth outcomes due to inflammation and infection of the placenta. Because of lesions and inflammation, men and women with urogenital schistosomiasis are also at a higher risk for HIV and other sexually transmitted infections (STIs).
Testing for Schistosomiasis
If your doctor suspects you might have a condition called urogenital schistosomiasis, they may conduct a simple urine test. Diagnosing this condition can be challenging as it requires finding and identifying eggs of the parasite in urine. This can be difficult because the amount of eggs released can change daily.
In addition to this, your doctor can use other testing methods, such as serology, which looks for antibodies in your blood, or PCR, a technique used to amplify the DNA of the parasite. However, these tests are not always reliable in areas where the infection is common because they can’t tell the difference between a current infection and a past one.
Using a combination of different tests, including urine tests, blood tests, and serology can give a more reliable result. Unfortunately, there is no definitive lab test to tell how many worms are in your body, making treatment harder to plan in a cost-efficient way.
Doctors can also identify the eggs of the parasite under a microscope. They are relatively large, oval-shaped structures. They notably have a structure called the terminal spine, unlike other types of similar parasites.
Your doctor may also use different types of imaging, like ultrasound, x-ray, IV pyelogram, cystoscopy, and colposcopy, to identify the infection. Ultrasound is becoming the go-to imaging technique in measuring the extent of the disease, but it uses a lot of resources. It can show abnormalities in the bladder due to the disease, such as irregularities, water retention in the kidneys, polyps, and tumors. An x-ray can reveal distinct calcifications due to scarring in the bladder. Computed tomography can also be helpful in diagnosis.
In women, the disease often presents with symptoms similar to sexually transmitted infections or infertility, leading to misdiagnosis. It’s the World Health Organization’s view that lack of awareness among health professionals is mostly to blame. To diagnose the disease in women, doctors can use a speculum examination and visually inspect the cervix and vagina for characteristic lesions such as “sandy patches”, overgrowth of blood vessels, and fragile tissue. A colposcopy and camera can improve visualization.
The presence and prevalence of a specific type of snail, Bulinus and S. haematobium, can be used to identify and monitor areas with a high prevalence of the disease. This can also help monitor how the disease spreads to areas where it’s less common.
Treatment Options for Schistosomiasis
Schistosomiasis, a type of worm infection, is usually treated with an anti-worm medication called praziquantel. This medication is effective in killing mature worms, preventing them from releasing eggs and causing new urinary tract issues. For best results, treatment should start about four to six weeks after exposure to the parasite.
While there has been some resistance from various Schistosoma species (the parasites that cause schistosomiasis) to praziquantel, such resistance has been minimal in S. haematobium, a specific species of these parasites. Also, praziquantel is considered generally safe for pregnant women.
If a case of urogenital schistosomiasis (schistosomiasis affecting the urinary and genital organs) is identified, it’s likely other individuals using the same water source may also be infected. Therefore, mass treatment efforts have proven successful in many communities and countries. For instance, Egypt saw significant success with a praziquantel mass treatment program launched in 1997. Before the mass treatment, many villages had prevalence rates of the disease ranging from 10% to over 30%. Following treatment, most of these villages saw their disease prevalence decrease to less than 3%.
What else can Schistosomiasis be?
The potential causes for certain urinary and reproductive health issues could be numerous. These can range from infections, sexually transmitted diseases to various other conditions including:
- Urinary tract infection
- Glomerulonephritis (a type of kidney inflammation)
- Sexually transmitted infections (such as gonorrhea, chlamydia, HSV, etc.)
- Cancer in the urogenital system
- Other causes leading to infertility
- Epididymitis (inflammation of the tube at the back of the testicle)
- Other parasitic infections such as S. mansoni and S. japonicum, clonorchiasis and trichinosis
- Renal tuberculosis (a form of tuberculosis affecting the kidneys)
What to expect with Schistosomiasis
During the early stages of chronic infection, the right use of a drug called praziquantel can reduce symptoms and prevent long-term swelling and the formation of granulomas, which are clusters of immune cells. However, damage to the urinary and genital areas may be only partially reversible, depending on the amount and kind of tissue damage. These areas can also experience ongoing issues as a result of the damage.
One study of 527 women found that treatment with praziquantel didn’t significantly reduce the occurrence of “sandy patches,” a visible issue seen with a procedure called colposcopy, which is a close examination of the cervix. Symptoms including bleeding when touched and irregularities in blood vessels also remained after the treatment.
The chance of recovery also depends on the likelihood of being re-exposed to the infection and the need for further treatment.
Possible Complications When Diagnosed with Schistosomiasis
As mentioned previously, there are several potential health issues that could arise from complications, including:
- Female infertility and spontaneous abortion
- Increased likelihood of sexually transmitted infections, including HIV
- Potential urinary tract obstruction that can cause chronic kidney disease and end-stage renal failure
- Bladder cancer
Bladder cancer that develops from chronic urinary tract obstruction is most often a squamous cell carcinoma, as opposed to the more common form of bladder cancer, transitional cell carcinoma. This complication is caused by a combination of chronic irritation, constant cell rebuilding and the resulting DNA and tissue damage.
People with an infection called schistosomiasis, especially those with a specific type called S. haematobium, become more susceptible to prolonged infections from various Salmonella species, including Salmonella typhi. Chronic inflammation caused by these conditions can lead to additional health problems:
- Anemia of chronic diseases
- Malnutrition
- Stunted growth in children
Preventing Schistosomiasis
Schistosomiasis, a type of disease, tends to affect people who live in poor conditions, don’t have access to good healthcare and don’t have good hygiene habits more frequently. One of the challenges in dealing with this disease is that many people are not aware of how common it is and what its symptoms are, making it hard to identify and treat the disease.
We can educate people about not urinating in freshwater lakes, as this can reduce the chances of the disease spreading. This is because a specific life stage of the parasite (called miracidia) needs to infect snails in the water to continue its life cycle, and this can only happen within a certain time frame.
If we want to get rid of this disease, we’ll have to use a multi-pronged approach. This might involve holding education sessions for the public and setting up mass treatment programs. Unfortunately, this approach will be costly and time-consuming, particularly for countries where the disease is commonly found. Many of these countries struggle with poverty, making it even harder to allocate resources towards fighting this disease.












