What is Vancomycin-Resistant Enterococci?
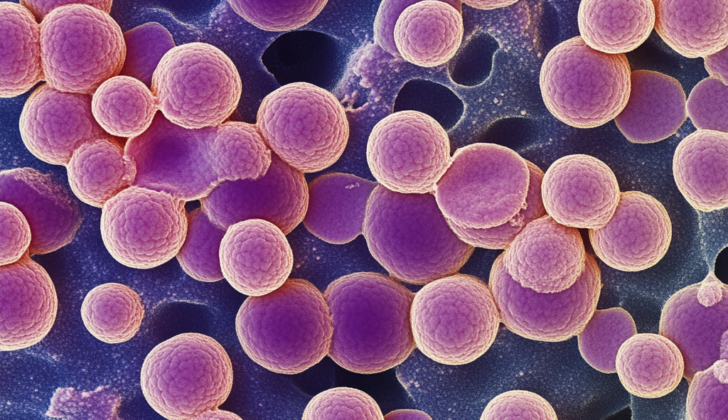
Antimicrobial resistance, or the ability of a microbe to resist the effects of medication, is becoming a serious issue for healthcare providers. A particular bacteria known as vancomycin-resistant Enterococcus (VRE) is becoming difficult to manage in hospitals. Enterococci are tiny organisms living in our digestive system that usually don’t cause problems. But, they can lead to several infections, like urinary tract infections, abdominal infections, bloodstream infections, or heart infections. They can also rarely cause infections in the brain, bones, joints, or lungs. Interestingly, VRE can often live in the body without causing an infection, making it harder to decide when and how to treat these infections. Despite these challenges, it’s been found that infections from VRE increase both the cost and chances of fatality when compared to Enterococcus bacteria that can be treated with vancomycin. With the rise of Enterococcus bacteria resistant to vancomycin, it’s important to use current treatments responsibly while also aggressively treating with specific antibiotics to manage this commonly encountered infection.
What Causes Vancomycin-Resistant Enterococci?
Enterococci are a type of bacteria that have evolved to become resistant to many antibiotics including aminoglycosides, B-lactams, tetracyclines, quinolones, and vancomycin. This resistance means that antibiotics are less effective or even ineffective in killing these bacteria. Enterococci have developed various means to resist antibiotics; for example, they can produce proteins with low attraction to B-lactams, create enzymes that break down these antibiotics, and reduce their ability to permeate the bacteria’s cell wall.
Specifically, the resistance to vancomycin, a type of antibiotic, arises from changes in the bacteria’s cell wall structure. Normally, this antibiotic binds to a specific sequence of two molecules (D-Ala-D-Ala) on protein precursors in the bacterial cell wall, inactivating or killing the bacteria. However, in resistant strains of Enterococci, this sequence is changed so that the antibiotic binds with less attraction, making it ineffective.
Different genes, identified by the alphabet from VanA to VanG, code for this resistance. Most common are the VanA and VanB genes, which are contained on small, independent, and transferrable DNA elements known as plasmids.
Resistance to aminoglycoside antibiotics, except for Streptomycin, mainly arises due to an enzyme called 2″-phosphotransferase-6′-acetyltransferase, which can deactivate the antibiotic. Streptomycin resistance, however, is due to the bacteria producing a different enzyme, streptomycin adenyltransferase, that inactivates the drug.
Risk Factors and Frequency for Vancomycin-Resistant Enterococci
The issue of vancomycin-resistant Enterococcus first became significant in the 1980s. This is believed to have derived from the use of a certain antibiotic known as avoparcin in livestock in Europe, and the increasing use of vancomycin in the United States. Throughout the 1990s and 2000s, it resulted in multiple epidemics in hospitals due to person-to-person spread. After being shed in feces, this bacteria is found on the skin and can spread via contact with infected surfaces.
From 2011 to 2014, various types of Enterococcus emerged as the second leading cause of healthcare-associated infections, according to the National Healthcare Safety Network. Specifically, E. Faecalis caused 7.4% of these cases. On top of this, Enterococcus was the most common cause of certain infections related to central lines used in medical treatment. It also ranked third for catheter-associated urinary tract infections, eleventh for pneumonia associated with ventilators, and second for surgical site infections. While the majority of Enterococcus cases are E. faecalis, most vancomycin-resistant Enterococcus cases are E. faecium. Resistance of E. faecium to vancomycin was as high as 83.8% for central line-associated bloodstream infections and 86.2% for catheter-associated urinary tract infections. In 2013, the CDC declared vancomycin-resistant Enterococcus as a “serious threat”, highlighting the need for better control and prevention.
There are many factors that can increase a person’s risk of colonisation and infection with vancomycin-resistant Enterococcus.
- The most commonly observed is previous antibiotic therapy, which may alter the natural flora in the bowel.
- Patients who have severe underlying illnesses or suppressed immune systems are also more likely to be at risk.
- The risk also increases with extended hospital stays or if admitted to long-term care facilities.
- Extended use of antibiotics is another risk factor.
- Being close to other patients with vancomycin-resistant Enterococcus also raises the risk.
Signs and Symptoms of Vancomycin-Resistant Enterococci
Vancomycin-resistant Enterococcus infection affects patients in different ways depending on its manifestation. Depending on where in the body the infection takes place, patients may experience a range of symptoms. The goal for healthcare professionals is to use the patient’s medical history and physical examination findings to determine the source and extent of the infection.
Enterococcus can cause several diseases. The most common is bacteriuria, although many consider this condition to result from colonization rather than infection. Other frequent causes of infection include bacteremia and endocarditis.
One of the major conditions caused by Enterococcus is urinary tract infection (UTI). Enterococcus often causes uncomplicated and complicated UTIs, especially those acquired in healthcare settings. Mostly, these infections are linked to urinary catheters and other urinary instruments. The severity of this condition can range from uncomplicated to complicated cystitis, or it may escalate to pyelonephritis, perinephric abscess, or prostatitis. It’s important to note that asymptomatic pyuria and bacteriuria should not be treated unless the patient shows signs or symptoms of UTI or sepsis.
Enterococcus is also commonly found in intra-abdominal and pelvic infections such as abscesses, wounds, or peritonitis. These infections are often part of a larger infection with other organisms. Moreover, intra-abdominal and pelvic abscesses often co-occur with enterococcal bacteremia, necessitating antibiotic coverage.
Bacteremia, which is a life-threatening condition, is another common manifestation of the infection. Hospital-acquired bacteremic infections usually result from urinary or intravascular catheters, while community-acquired bacteremia is usually due to bacteria moving from the gastrointestinal (GI) and genitourinary (GU) tract into the bloodstream. Infections due to Enterococcus faecium in the bloodstream often result in higher mortality because they are more resistant to treatment.
Enterococcus is the second most common cause of infective endocarditis, a severe infection of the heart’s inner lining. This condition often arises from central lines, GI or GU tracts following manipulation, damaged heart valve infections, or liver transplants. Community-acquired endocarditis can occur in patients without risk factors and typically presents subacutely with fevers and general body discomfort. Other infection signs may include fevers or a new heart murmur.
Less common sites of Enterococcus infection include the central nervous system; such as infections associated with neurosurgical interventions like shunts. Some may experience altered mental status and fevers. Enterococcus may also cause skin infections, including decubitus ulcers, osteomyelitis, and soft tissue abscesses. Pneumonia due to enterococci is very rare, but when it happens, it is often seen in severely weak and immunocompromised patients who have previously received broad-spectrum antibiotics.
Testing for Vancomycin-Resistant Enterococci
If your doctor thinks you may have an infection caused by vancomycin-resistant Enterococcus, they will first confirm if you have an underlying infection. After this, they will need to examine each possible source of infection.
Your doctor will collect samples from these potential sources, and send them to a lab before giving you any sort of “broad-spectrum” antibiotic that might be used to treat various types of infections. The lab will then culture these samples, by allowing bacteria to grow in a controlled environment.
This culture process helps determine the exact species of bacteria causing your infection and the specific type of drugs they are sensitive or resistant to. This is important to make sure the treatment prescribed to you works as expected.
In some labs, they usually don’t test for sensitivity to drugs like fosfomycin, daptomycin, nitrofurantoin, and chloramphenicol, but your doctor may request these tests depending on your condition.
Treatment Options for Vancomycin-Resistant Enterococci
Treating Enterococcus infections that are resistant to the antibiotic vancomycin can be a little challenging. This difficulty stems from the fact that the correct choice of antibiotics depends on the specific type of infection and the individual characteristics of the disease-causing organism. Given the condition’s complexity, doctors often base the decision to start treatment on their clinical judgement and response to earlier treatments.
Most Enterococcus infections are caused by a particular type, E. faecalis, which typically responds well to a group of antibiotics called beta-lactams and aminoglycosides. Given this, these types of antibiotics are often the first choice of treatment, unless test results suggest otherwise. On the other hand, strains of another type, E. faecium, are usually highly resistant to both beta-lactams and aminoglycosides. When these are not effective, two primary treatments that are likely to be used are antibiotics called linezolid and daptomycin.
If a highly susceptible strain of vancomycin-resistant Enterococcus causes the infection, then a more specific treatment can be provided. In urinary tract infections, for example, a high dose of the antibiotic ampicillin is usually given. If the infection is resistant to ampicillin, nitrofurantoin or fosfomycin are typically used. However, sometimes this type of infection is due to the presence of an urinary catheter, so removing it could be part of the treatment.
Linezolid could be used as well if the infection is not responding to other treatments or if the organism causing the infection is highly resistant to other antibiotics. Linezolid works by binding to a part of the bacteria, preventing it from forming necessary bonds for survival.
On the other hand, using the antibiotic daptomycin is another possible approach, but typically in high doses. Fusion of daptomycin with other drugs like ampicillin or ceftaroline could be an option in some cases.
If a patient is not able to tolerate linezolid or daptomycin, tigecycline might be used instead. It is a broad-spectrum antibiotic, meaning it can act against a variety of bacteria. Chloramphenicol could be used as well, but not typically as a first choice due to its high potential for adverse effects.
Treatment of this type of infections can be quite complex and may require consultation with an infectious disease specialist. But knowing the basics of how these infections are treated could be helpful for patients.
What else can Vancomycin-Resistant Enterococci be?
When we discuss serious infections that can occur in the body, the list includes:
- Bacterial sepsis (an extreme reaction to a bacterial infection)
- Hospital-acquired infections (infections you get while receiving healthcare)
- Infective endocarditis (infection of the inner layer of the heart)
- Peritonitis and abdominal sepsis (infections in the lining of your abdomen or in your abdomen)
- Pyogenic hepatic abscesses (pus-filled pockets in the liver)
- Septic arthritis (a painful joint condition caused by a bacterial infection)
- Uti and cystitis in women (urinary tract infections and bladder inflammation)
- Uti in men (urinary tract infection)
- Wound infection (infections of the skin or of surgical wounds)
Possible Complications When Diagnosed with Vancomycin-Resistant Enterococci
- Heart valve inflammation (Endocarditis)
- Inflammation of the colon (Colitis)
- Inflammation of the bones (Osteomyelitis)
- Body-wide infection (Sepsis)
- Lung infection (Pneumonia)
Preventing Vancomycin-Resistant Enterococci
Washing your hands properly and regularly, as well as maintaining good personal hygiene, is crucial. This involves keeping yourself clean and taking care of your body to prevent illnesses and infections.