What is Viral Conjunctivitis?
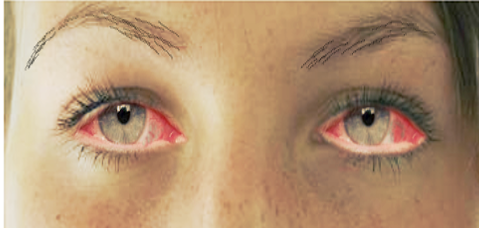
Conjunctivitis, often causing redness in the eye, is a common condition that can affect anyone regardless of their age or income level. The most usual type of conjunctivitis comes from a viral infection, causing up to 75% of all cases. Common symptoms of viral conjunctivitis include eye redness, enlarged blood vessels in the eyes, discharge from the eye, pain, sensitivity to light, and a false membrane forming over the eye.
This condition has a substantial impact on society and the economy because of the costs associated with doctor’s visits, diagnostic tests, treatments, and the time people have to take off work or school. Notably, one of the most significant expenses in any health care system is the prescribing of antibiotics in cases of viral conjunctivitis. In the United Kingdom, it is estimated that between 80% and 95% of patients with infectious conjunctivitis are treated with antibiotics.
Improving how well we diagnose viral conjunctivitis has been found to significantly decrease unnecessary antibiotic prescriptions, saving an estimated $430 million each year in the United States alone. Currently, more specific treatments for viral conjunctivitis are being tested in clinical trials.
Because the signs and symptoms of conjunctivitis can vary greatly, it’s important for doctors to take a careful medical and eye health history, particularly in patients whose symptoms are not typical or have been persistent for a long time.
What Causes Viral Conjunctivitis?
The conjunctiva is a thin, slightly see-through membrane like a protective layer that covers the white part of your eye, also known as the sclera. It begins at the edge of the clear front surface of your eye (the cornea) and covers both the sclera and the inner side of your eyelids. The part that covers the sclera is called the bulbar conjunctiva, and the part covering the inner eyelids is the palpebral conjunctiva.
The adenovirus, a type of virus that does not have an outer coating and carries its genetic information in double-stranded DNA, often causes viral conjunctivitis, also known as “pink eye.” This virus can also cause symptoms like a common cold, eye infections, and diarrhea, especially in kids. Children are usually more likely to get viral infections, while adults are more prone to bacterial infections. You can get viral conjunctivitis through physical contact, airborne particles, or communal places like swimming pools.
Viral conjunctivitis can spread easily for 10-14 days, and the best way to prevent passing it on is by washing your hands and avoiding touching your eyes.
Adenoviruses cause up to 90% of viral conjunctivitis cases. This infection often results in symptoms like a pink eye with high fever, sore throat, and swelling of glands near the ear in children. Specific types of adenoviruses can also lead to a serious eye infection. It can affect the cornea, leading to small damages in the eye surface and deposits underneath. These causes of discomfort can be managed with eye drops containing povidone-iodine and possibly other drugs.
Herpes can also cause conjunctivitis in both adults and children. The herpes simplex virus (HSV), causes pink eye in about 1.3 – 4.8% of cases. Treating these cases often involves the use of antiviral eye drops to reduce the virus and prevent further complications. Chickenpox and shingles can cause conjunctivitis either due to direct eye contact, touching skin rashes, or inhaling infectious particles.
Acute Hemorrhagic Conjunctivitis (AHC) is a highly contagious form of pink eye. Symptoms include the sensation of a foreign body in the eye, excessive tearing, swollen eyelids, blood inside the eye, and swelling of the conjunctiva. Some people may also experience fever, fatigue, and limb pain. It’s usually spread through hand-to-eye contact.
You also might have heard about COVID-19, the newest strain of the coronavirus, causing conjunctivitis along with fever, cough, and breathing problems. Studies show that 1% to 6% of patients show symptoms of pink eye related to COVID-19. Eye doctors are at a higher risk for catching COVID-19 because of their close contact with patients. To reduce their risk of infection, people should practice social distancing, wear masks, avoid crowded places, and regularly clean surfaces.
Risk Factors and Frequency for Viral Conjunctivitis
Conjunctivitis, also known as ‘pink eye,’ is a common issue that affects millions of people in America every year. Around 1% of all primary care doctor visits in the country are related to this condition. There are two types: viral conjunctivitis, which is the most frequent, and bacterial conjunctivitis, which is the second most common. It can be challenging for doctors to tell the difference between the two.
It is also common for antibiotics to be prescribed, sometimes without a strong reason. This could potentially result in unnecessary costs for the patient and an increase in bacteria that are resistant to drugs. Furthermore, workplaces and schools usually ask people with conjunctivitis to stay home until they’re no longer infectious, which may lead to additional financial pressure.
Signs and Symptoms of Viral Conjunctivitis
Viral conjunctivitis, or “pink eye,” is generally diagnosed by doctors based on symptoms and laboratory results. This type of infection can be recognized early on, allowing for proper treatment and avoidance of long-term issues.
People with viral conjunctivitis usually experience sudden sensations of having something in the eye, red eyes, itching, sensitivity to light, burning, and watery discharge from the eyes. Symptoms of bacterial conjunctivitis are similar, but also include a yellow-greenish liquid discharge from the eyes and crusting of the eyelids in the morning. Those with viral conjunctivitis often have a recent history of a cold or came into contact with someone who was sick. Vision usually stays about the same, although inflammation of the cornea can lead to decreased vision and light sensitivity. The inner surface of the eyelids may also show signs of inflammation. Sometimes, a thin layer of material can appear on the inside of the eyelids or whites of the eyes which, when removed, may cause bleeding.
In some cases, you can see small bumps without a central blood vessel on the inside of the eyelids. Although these bumps are common in patients with viral conjunctivitis, they do not necessarily mean you have a viral infection. Doctors will also feel the glands in front of the ears for signs of infection and differentiate between a viral and bacterial infection. For some viral infections, like herpes, small blisters may appear on the face or eyelids and vision can be affected.
- Sudden sensation of something in the eye
- Red eyes
- Itching
- Sensitivity to light
- Burning
- Watery eye discharge
- Decreased vision
- Light sensitivity
- Possible presence of small bumps on inner surface of eyelids
- Signs of inflammation
Additional symptoms like fever, fatigue, enlarged lymph nodes, and other general signs of being unwell can help differentiate viral conjunctivitis from other causes. Severe eye conditions, like inflammation of the uvea (the middle layer of the eye), inflammation of the cornea, and inflammation of the sclera (the white outer layer of the eye), can cause an unequal size of pupils and sensitivity to light. Certain systemic diseases, including skin and mucous membrane diseases, autoimmune diseases, and collagen vascular diseases, are also associated with conjunctivitis.
Testing for Viral Conjunctivitis
If your symptoms aren’t getting better and your infection lasts for longer than 4 weeks, you may need some lab tests. These tests might also be done if there’s an unusually high amount of discharge, you might have a certain disease like chlamydia or gonorrhea, or if you’re a newborn or have a weaker immune system. At the doctor’s office, they can do tests that can detect adenovirus, which causes conjunctivitis, with accuracy rates of 94% and 89%.
Normally, eye doctors, or ophthalmologists, can diagnose conjunctivitis based on your symptoms and an eye exam. They might confirm the diagnosis with additional testing.
For adenovirus testing, doctors have typically used cell culture. This is where they grow the virus in a lab setting. Although it’s considered the most reliable method for diagnosis and allows further study of the virus, it does have some downsides, like high cost and long waiting time for results. A common method of testing for viral conjunctivitis, which is conjunctivitis due to viruses like adenovirus, involves detecting the viral DNA – the virus’s genetic material – through a technique called polymerase chain reaction (PCR). The PCR method has been shown to be very accurate (93% sensitive and 97.3% specific) and is being used more commonly.
There’s a new rapid detection test for adenovirus, called the AdenoPlus assay. This test can identify 53 types of adenovirus and gives results in 10 minutes. Research shows that it’s highly accurate (around 92% to 98%) in detecting adenoviral conjunctivitis. However, it may not be as sensitive as PCR testing, so not all cases might be caught. As more treatments become available for viral conjunctivitis, this kind of rapid test may become increasingly useful.
Treatment Options for Viral Conjunctivitis
The treatment for viral conjunctivitis, often known as pink eye, aims to make the patient more comfortable because the virus tends to disappear on its own. The condition can last up to three weeks. As part of the treatment, patients may be advised to use artificial tears to soothe the eye and cool compresses on the surrounding area.
Ensuring good hand hygiene is crucial to stop the infection from spreading to someone else or the other eye. This includes washing hands frequently, not sharing towels or linens, and avoiding any direct eye contact.
If the patient has a thin layer or a false thin layer (termed medically as membrane or pseudomembrane) covering their eye, removing it can help improve comfort and prevent any scars from forming. This can be done using small tweezers or a cotton swab with a local anesthetic.
In some cases, topical steroids could be provided to ease symptoms, but they could extend the time a person is contagious. The patient should be aware that they could spread the virus even if they don’t have visible symptoms. Steroids should be given mainly to those patients who experience vision loss or extreme discomfort due to their condition.
Using povidone-iodine, a general disinfectant, is a new and promising treatment for viral conjunctivitis. It is an affordable and commonly available antiseptic solution that can help reduce the symptoms and recovery time. However, it will not work on any organisms that might have entered cells.
Topical corticosteroids should not be used by themselves for a type of viral conjunctivitis caused by the herpes simplex virus as it can extend the duration of the virus and the infection. When used with anti-infectives for conjunctivitis, corticosteroids have shown to be both effective and well-tolerated.
What else can Viral Conjunctivitis be?
Conjunctivitis, often called “pink eye,” is often caused by viruses or bacteria, or it can be due to an allergic reaction. However, if the treatment doesn’t seem to be working, the problem may actually be something else. Below are some conditions that can look similar to conjunctivitis:
- Uveitis: This is an inflammation of the eye caused by an autoimmune response. It might be a local response and happen for no clear reason, or it could be a symptom of a broader autoimmune disease like rheumatoid arthritis, lupus, or ankylosis spondylitis.
- Sjogren syndrome or Stevens-Johnson syndrome: These systemic autoimmune diseases can cause redness and discharge from the eye, which might look like conjunctivitis.
If a doctor suspects any of these conditions, they will likely suggest more tests. There are also more serious conditions that can be mistaken for conjunctivitis:
- Cavernous carotid fistula: This is when there’s an abnormal connection between the arterial and venous circulation in the eye, leading to dilation of the venous system. If it ruptures and bleeds, it could cause permanent eye damage or even death. It can look like conjunctivitis because it causes congestion of the eye’s vessels. Signs that it might be a fistula rather than conjunctivitis are if the eye is protruding or the globe of the eye is pulsing.
- Orbital cellulitis: This is an infection in the area behind the septum that includes the contents of the orbit. It can cause symptoms similar to conjunctivitis, but patients may also experience pain when moving the eye or restricted eye movements.
- Orbital hemorrhage: This is a situation where there’s a bleed in the eye, which is a medical emergency. The cause is generally traumatic, but it’s also possible for a bleed to happen spontaneously, particularly in patients taking blood thinners. Symptoms can include a protruding eye, tight eyelids, and redness of the conjunctiva.
What to expect with Viral Conjunctivitis
Most cases of virus conjunctivitis, or “pink eye”, get better on their own. However, in rare situations, a long-term infection can occur. The pink eye typically clears up in about two to four weeks. For a few people, they might experience symptoms like sensitivity to light, reduced vision, and experiencing glare as an issue.
Possible Complications When Diagnosed with Viral Conjunctivitis
- Small, pinpoint corneal inflammation
- A secondary bacterial infection
- Scarring of the eye’s conjunctiva
- Ulcers on the cornea
- Long-term infection
Preventing Viral Conjunctivitis
Most cases of pink eye, or viral conjunctivitis, are caused by adenoviruses. One way to prevent spreading it to others is through frequent hand washing, cleaning surfaces regularly, and keeping those with pink eye separated from others when possible. Since there isn’t a specific treatment for this type of pink eye, ways to feel better can include using artificial tears, applying a cold-compress to the eyes, and using antihistamine medications.
Using eye drops with antibiotics isn’t usually recommended because it can make bacteria more resistant. If there are membranes or pseudomembranes, which are like false membranes over the eye, they need to be removed to help decrease any discomfort and prevent scarring.
In some cases, if there’s a formation of a membrane and small infiltrations under the epithelium, which is the outer layer of the eye, causing light sensitivity and reduced vision, corticosteroid eye drops may be used. But this method should only be used under the guidance of a doctor.