What is Whipple Disease?
Whipple disease is caused by a type of bacteria known as Tropheryma whippelii. This illness is systemic, meaning it impacts the whole body, not just one area. It can cause various problems including difficulties in absorbing nutrients from food through the digestive system (malabsorption). It can also impact other parts of the body, such as the heart and blood vessels (the cardiovascular system), the brain and nerves (central nervous system), and the joints.
The disease was first described by Dr. George Hoyt Whipple in 1907. Dr. Whipple was the first American to win the Nobel Prize in Physiology – science that deals with the way organisms, animals and humans function. He wrote about a 36-year old man who had difficulty absorbing nutrients from his diet, swollen lymph nodes in his abdomen (mesenteric lymphadenopathy), joint pains (arthralgias), and increased skin colour (pigmentation). Dr. Whipple called the condition “Intestinal Lipodystrophy.” He suspected that an infection was the cause, but the specific bacteria were only recognized in 1992.
Despite being noted for over a century, Whipple disease is still very rare. Most of what we know about the disease comes from individual case reports, rather than large-scale studies.
What Causes Whipple Disease?
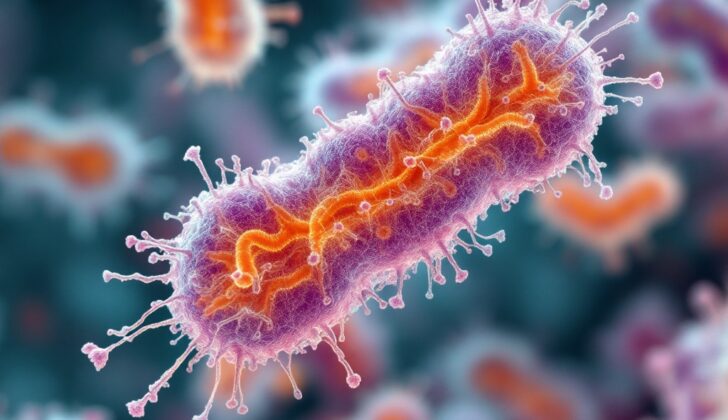
Tropheryma whipplei is a type of bacteria first identified in 1992. It was originally named Tropheryma whippelii, but in 2001, its name was changed to line up with the correct spelling of Dr. George Hoyt Whipple’s name. This bacteria is a kind of bacillus, which means it’s shaped like a small rod.
Troheryma whipplei is classified as gram-positive, meaning it holds onto a specific kind of stain when viewed under a microscope, which helps doctors identify it. Additionally, it’s ‘periodic acid-Schiff-positive’ (PAS), a term used when a substance in the bacteria turns a bright colour under a microscope after being treated with a particular chemical mix called periodic acid-Schiff.
When viewed under an electron microscope, Tropheryma whipplei appears to have a core enclosed within a shell-like structure called a plasma membrane. This is then surrounded by a cell wall with three layers. The inner layer has certain sugars, or polysaccharides, that also respond positively to the PAS treatment, turning colour under the microscope.
The outer layer of the bacteria’s cell wall looks similar to the plasma membrane and might originate from the host, or the person infected by the bacteria. This similarity to the host’s cells is thought to be why our bodies do not effectively produce antibodies in response to this infection. Antibodies are specialized proteins that, normally, help us fight off infections; thus, this bacteria is a bit elusive to our immune system.
Risk Factors and Frequency for Whipple Disease
Whipple disease is an uncommon condition that is mostly reported in North America and Europe. It is associated with a specific genetic trait known as the HLA B27 haplotype. Only about one to three in every one million people are affected by it. This disease typically begins to show symptoms around the age of 55. It is more common in men than women, with the ratio being 4:1. It’s thought that the bacteria causing the disease live in the soil, which could be why farmers get Whipple disease more often.
Signs and Symptoms of Whipple Disease
Whipple disease is a condition that affects many organ systems due to an infection and typically causes symptoms similar to other digestion-related diseases. The key symptoms experienced are weight loss, diarrhea (which may contain fat or be watery), aches in the joints, fever, and abdominal pain. In some cases, there may be hidden or visible bleeding in the gastrointestinal tract.
Swelling of the ankles, feet, or hands (peripheral edema) can also be a symptom due to the body losing protein and experiencing poor nutrition. Joint pains are typically migratory and involve large joints without causing damage. They usually occur before any intestinal symptoms appear. These joint attacks come on suddenly and may last for a few hours to days. Fever is also seen in some patients.
In about a third of the patients, the disease can affect the heart causing pericarditis (inflammation of the tissue surrounding the heart) and endocarditis (inflammation of the heart’s inner lining). However, these do not usually cause significant symptoms. In 25% of patients, the upper part of the heart muscle can be heard beating irregularly. In up to 10% of patients, rubbing sounds or symptoms of failing heart health can be detected.
A portion of patients may also experience symptoms related to the central nervous system such as signs of loss of voluntary control, lack of coordination, and rapid muscle contraction and relaxation. There have also been reported cases of difficulty moving the eyes. Some patients may also experience confusion, seizures, delusions, cognitive impairment, unusual body movements, excessive sleep, and problems with their muscles. After death, examinations have shown that the central nervous system is affected in the vast majority of patients, but symptoms are only seen in a small to moderate proportion of cases.
On physical examination, patients may show signs of swelling of the lymph nodes at the periphery, have dark spots on the skin around the eyes and cheekbones, rough skin, bleeding under the skin or bulging of the stomach. Other signs may include inflammation of the tongue, inflammation of the lips, gum disease, and signs of abnormal reactions to certain stimuli.
- Weight loss
- Diarrhea
- Joint aches
- Fever
- Abdominal pain
- Peripheral edema (swelling)
- Pericarditis and endocarditis (heart inflammation)
- Signs of central nervous system involvement
- Swelling of the lymph nodes
- Skin discoloration and roughness
- Bulging stomach
- Inflammation of the tongue, lips, and gums
Testing for Whipple Disease
Whipple disease is diagnosed by taking a small tissue sample from the intestine, also known as a biopsy, and finding the disease-causing bacteria. The diagnosis is usually confirmed when the biopsy reveals PAS-positive foamy macrophages, a type of cell that tries to fight the bacteria.
If the results are unclear or negative, doctors can also confirm Whipple disease by looking for two other signs:
- The presence of foamy macrophages in a biopsy tissue sample, revealed by a test known as PAS staining.
- PCR detection of T. whippelii, the bacteria that causes Whipple disease, or the specific genetic material of this bacterium, known as 16S rRNA.
- A positive result on a test using T. whippelii antibodies, called immunohistochemical staining.
However, it’s important to remember that after treatment for Whipple disease begins, tests for T. whippelii often come back negative. This means that even though the patient has the disease, the test might not show it – this is called a false negative. Particularly, this is a common scenario when antibiotics are given before comprehensive diagnostic testing.
Other common test findings in patients with Whipple disease include low levels of iron, folate or vitamin B12 (which can all lead to anemia), high number of neutrophils (a type of white blood cell), typically found in about a third of the patients. There can be slightly low lymphocyte count, known as mild lymphocytopenia. Exceptionally, there can be high count of eosinophils (a type of white blood cell) and low platelet count, a condition known as thrombocytopenia. Low albumin levels, with normal globulin levels, blood proteins, is also a frequent occurrence. There may be a prolonged prothrombin time, a test that measures how long it takes for your blood to clot. Finally, steatorrhea, or fatty stools, occur in about 93% of cases.
Treatment Options for Whipple Disease
Whipple disease is generally treated with antibiotics. This is because there’s a chance the disease can affect the central nervous system (CNS), which includes the brain and spinal cord. This can happen even if you don’t show any symptoms. Therefore, doctors usually recommend antibiotics that can penetrate the protective barrier between the brain and the bloodstream.
Typically, the treatment course begins with an initial phase where antibiotics like Ceftriaxone or Penicillin G are used. For those allergic to penicillin, another antibiotic called Meropenem can be used. This initial phase usually lasts two weeks.
After this, the maintenance phase begins, which usually involves an oral medication known as Trimethoprim-Sulfamethoxazole, and it’s taken for about twelve months. This long treatment period is necessary to prevent the disease from coming back.
However, it’s important to know that the disease can come back even years after treatment. If it does return, it often shows up first as symptoms affecting the CNS, like headaches or changes in mental function.
After the initial, more intensive antibiotic treatment, it’s generally necessary to continue taking oral antibiotics like Trimethoprim-Sulfamethoxazole for at least 12 months.
To make sure the treatment is working and the disease is fully treated, your doctor will check your body fluids regularly to see if the bacteria causing the disease are present. It might take 1-2 years to confirm that a cure has been achieved.
What else can Whipple Disease be?
When a doctor is trying to diagnose Whipple disease, they have to rule out several other conditions that might cause similar symptoms. These include:
- HIV
- Tuberculosis
- Inflammatory bowel disease with joint issues
- Connective tissue disorder
- Hyperthyroidism
What to expect with Whipple Disease
Whipple disease, when diagnosed and treated quickly, usually has a good outcome. Patients typically start to feel much better within two to three weeks after starting treatment. However, if Whipple disease isn’t treated, the prognosis isn’t good, meaning patients may not recover well or their health may worsen.
Possible Complications When Diagnosed with Whipple Disease
Whipple disease, if not diagnosed and treated, can become progressively worse over time. If left untreated, most complications are due to deficiencies in nutrition. This happens because the disease interferes with how the small intestine absorbs nutrients. There have also been a few cases reported where the disease has spread throughout the body, causing sepsis. If the disease progresses this far, irreversible brain damage and even death can occur.
List of Potential Complications:
- Nutritional deficiencies
- Disease spreading throughout the body (sepsis)
- Irreversible brain damage
- Potential death