What is Acute and Chronic Thermal Burn Evaluation and Management?
Thermal burns, or burns caused by heat, are a major cause of health problems and deaths around the world. These burns can result in long-term injuries and can severely affect a person’s mental wellbeing and financial situation. However, with the right treatment, it’s possible for someone to recover both physically and emotionally. Once you’ve read this article, you should have a basic understanding of how to take care of burns, how burns affect the body, and the teamwork needed from healthcare professionals to effectively care for a burn patient after surgery.
What Causes Acute and Chronic Thermal Burn Evaluation and Management?
Thermal burns happen when body tissue comes into contact with a source of heat. If that heat source is really hot or the contact lasts a long time, the burn can be more serious and affect more deeply into the skin. There are three main types of thermal burns.
The first type is flash and flame burns, which happens when someone is exposed directly or indirectly to a source of fire. This can happen when something that can catch fire, something that helps things burn, and a source of heat are all together. Also, if you’re exposed to open flames in an enclosed space, you may inhale some of the fire, causing injuries.
The second type is a scald burn. These are due to contact with very hot liquids. Specifically, burns from hot oils or grease can be deeper than they first seem.
The last type of thermal burn is a contact burn. This happens when the skin directly touches something very hot. People with conditions like epilepsy or habits such as alcoholism are more likely to have this kind of burn because those conditions or habits can make them unable to react to such dangers in time.
Risk Factors and Frequency for Acute and Chronic Thermal Burn Evaluation and Management
According to the World Health Organization, thermal burns result in about 6.6 million injuries and 300,000 deaths globally each year. Most of these deaths, about 95%, sadly happen in poorer countries due to lack of access to proper healthcare and education. In these areas, open fires for cooking, heating, and lighting are common, making burns more frequent. The 2014 global fire statistics revealed that burn injuries from fires significantly impact the economy – it’s estimated that direct losses make up 0.02-0.22% of a country’s average Gross Domestic Product (GDP), while indirect losses can total up to 0.95%.
- Two-thirds of fire-related costs were due to burns suffered by males.
- The number of deaths due to burns per 100,000 people varied from 0.02 in Singapore to 2.03 in Finland. The United States had a mid-range rate of 1.11.
- Flame and flash burns were responsible for the majority of burns in adults admitted to the hospital.
- For children, the majority of burn admissions were due to scalds.
Signs and Symptoms of Acute and Chronic Thermal Burn Evaluation and Management
It’s important to gather a comprehensive history for patients with thermal burns. This should include not only the usual medical, social and surgical history, but also specific details related to the burn injury. Understanding how the burn occurred gives clues about the burn’s depth and whether there’s a risk of related traumas or injuries from inhaling smoke or hot air. Certain patterns of burns or differences between what the patient tells you and what you see could suggest abuse, particularly in children and older adults.
Medical professionals should also ask about the amount and type of fluid the patient received to stabilize their condition. The presence of conditions that could affect healing of the burn (like diabetes), or that could put the patient at risk during treatment (like heart disease), is also important to know.
A thorough physical examination from head to toe is vital for identifying all burn injuries and signs of any other injuries, like inhalation injury. The depth and extent of the burns provide crucial information for determining the required treatment.
- Superficial burns cause redness and mild to moderate pain without blisters.
- Superficial partial burns have blisters and a wet, pink skin layer that turns white briefly when pressed. This type of burn is often very painful.
- Deep partial burns are less painful and result in a white, waxy layer of skin without blisters.
- Full-thickness burns result in painless, dry, leathery skin that may be black.
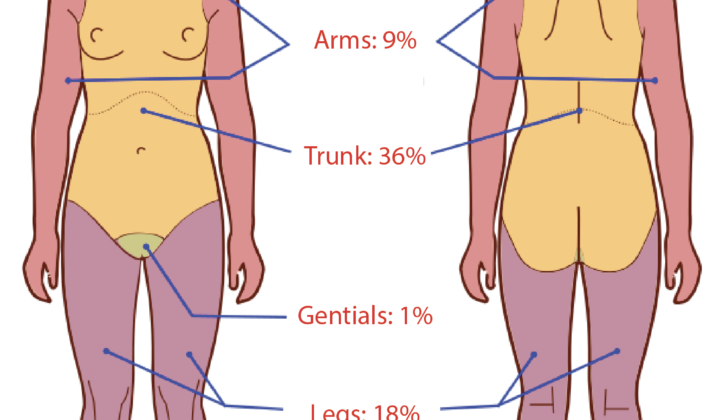
Total body surface area (TBSA) of second-degree or deeper burns should be estimated using measuring tools for adults or appropriate child-specific tools. Areas with full-thickness burns wrapping all the way around a limb or body part should be monitored for compartment syndrome – a dangerous condition where increased pressure affects blood flow and damages muscles and nerves. Symptoms include severe pain, abnormal sensations like tingling or numbness, changes in skin temperature, paralysis, and a lack of pulse.
Testing for Acute and Chronic Thermal Burn Evaluation and Management
If you’re suspected of having been injured, health professionals will conduct a variety of tests according to the ATLS (Advanced Trauma Life Support) guidelines. These tests will analyze your general health, the balance of minerals in your body, and your nutritional status. The tests usually include a complete blood count, a full metabolic profile, a test that measures how quickly your blood clots, and a test to determine your protein levels, known as pre-albumin.
They may also perform a urine drug screen. This is particularly important in this group of patients. Women who are able to have children will also need a pregnancy test. Another test doctors may carry out is to check the levels of carboxyhemoglobin in your blood. This can help indicate whether you’ve been exposed to carbon monoxide, which can cause poisoning. It also provides information about any potential damage to your lungs and whether you’re at risk of lung failure.
However, keep in mind that the amount of carboxyhemoglobin in your blood decreases pretty quickly if you’re receiving 100% oxygen. It roughly halves every four hours. Because of this, a test taken several hours after an injury showing low levels of carboxyhemoglobin doesn’t necessarily mean you haven’t inhaled any harmful substances.
Treatment Options for Acute and Chronic Thermal Burn Evaluation and Management
The first step in treating any burn patient is ensuring their airway, breathing, and circulation are stable – since they’re considered trauma patients first and foremost. This involves immediate medical support such as rehydration with special fluids, possible blood transfusions, and possibly inserting a tube into their windpipe to assist breathing. After this initial stabilization, it’s important to evaluate if the patient should be transferred to a specialist burn center.
Several factors may warrant a transfer, including if burns cover 10% or more of the total body surface area (TBSA), burns that affect sensitive areas such as the face, hands, feet, genitals or major joints, chemical or electrical burns, severe burns combined with other major injuries, and large burns in patients who need special care or have pre-existing medical problems that may affect survival rates. Moreover, burns in children should be treated by a team with the right expertise and equipment.
Determining the extent of the burn is crucial in deciding if the patient needs rehydration and how much fluid they should receive. While there’s some debate among experts on the best approach to burn rehydration, the American Burn Association agrees that patients with burns covering 20% or more of the TBSA usually require formal rehydration. Commonly used methods to calculate the rehydration fluids needed by burn victims include the Parkland and Modified Brooke formulas. But it’s important to note that giving too much fluid can be harmful too, which is why the rate should be adjusted based on physical responses, such as urine production.
The basic principles of burn wound care aim to prevent infection, remove dead tissue, lessen fluid loss, and minimize costs. There are different kinds of topical antibacterial treatments, such as silver nitrate, silver sulfadiazine, and mafenide acetate. Silver sulfadiazine is the most used as it penetrates well, has a broad antibiotic coverage, and is less painful than mafenide acetate. Silver nitrate is generally used for shallow burns in patients allergic to Sulfa, while mafenide acetate is used for very deep, heavily infected wounds, and burns on the ear, owing to its superior reach into cartilage.
For deep burns, damaged tissue needs to be surgically removed and replaced with a skin graft. Without surgery, these wounds can take three weeks or more to heal, which puts the patient at risk of wound infection, extensive scarring, and the formation of scar tissue that tightens and restricts movement. With early surgical treatment, the wound can heal within 7 to 10 days, significantly reducing these risks. For larger burns, early surgical removal and skin grafting also greatly reduce inflammation, help regulate body temperature, and manage fluid loss.
What else can Acute and Chronic Thermal Burn Evaluation and Management be?
Before a doctor can confirm that a patient has gotten a thermal burn, they need to ensure that two other conditions aren’t causing the symptoms. These conditions are:
- Cellulitis – an infection of the skin and the tissue underneath
- Toxic Epidermal Necrolysis (TEN) – a severe skin reaction typically caused by a drug allergy
These possibilities have to be ruled out to make a correct diagnosis.
What to expect with Acute and Chronic Thermal Burn Evaluation and Management
Thermal burn injuries are a serious issue that often result in severe health complications or even death. The rate of death may be even higher in cases where the individual has inhaled dangerous substances as a result of the burn – though, existing studies on this are limited and not fully conclusive. Current published research on burns survival suggests that the three strongest indicators of whether a person will die from their burns are the total proportion of the body surface area (%TBSA) affected by the burn, whether they’ve inhaled harmful substances due to the burn, and their age.
Possible Complications When Diagnosed with Acute and Chronic Thermal Burn Evaluation and Management
Burns, especially those related to heat or fire, are highly susceptible to becoming infected. Often, these infections aren’t just localized to the burned area. They can spread, causing other serious infections within the body, including in the bloodstream and lungs. If not managed properly, this can progress to a dangerous condition known as sepsis, whereby the entire body inflames in response to the infection. This can then cause all the body functions to go awry, potentially resulting in death. Alongside these daunting physical aspects, burn victims often grapple with mental health challenges such as anxiety and depression, stemming largely from the physical scars and disfigurement caused by the burns.
Preventing Acute and Chronic Thermal Burn Evaluation and Management
- First and foremost, stop the process of burning.
- Remove all clothes affected by the burn. Hot clothes could lead to a more severe injury. If the clothes are sticking to the skin, carefully cut or tear around them.
- Cool off the burned areas by pouring cool water over them. This should be done for about 3 to 5 minutes, or up to 30 to 40 minutes in the case of a chemical burn.
- Don’t place ice on the burns. This could cause further harm and even lead to low body temperature, also known as hypothermia.
- Get rid of all accessories like jewelry, belts, and any tight clothing. Burned areas tend to swell up quickly. If the person’s neck is burned, make sure nothing is obstructing it.
- Avoid applying ointments or other homemade remedies on severe burns. These might lead to serious infections.
- Cover the burns using a clean, dry bandage or sheet.
- Try to maintain the victim’s body temperature by keeping them warm.
Make sure to seek medical attention without any delay.