What is Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)?
Injury to the subclavian artery, a major blood vessel, necessitates swift detection and immediate medical intervention. A detailed understanding of body structure can aid in the diagnosis and guide the choice of surgical procedure. Recent research indicates that a technique called endovascular management could be useful in treating these kinds of injuries. This discussion will cover different aspects of subclavian artery damage.
What Causes Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)?
Injuries to the subclavian artery, a major blood vessel found behind the collarbone, are quite rare, happening in less than 5% of people who have been in a trauma. Because these vessels are tucked behind the collarbone, a serious incident is typically needed to cause any damage. One noteworthy fact from autopsy reports is that most people with such injuries don’t survive long enough to reach the hospital.
For those who do make it to the hospital, there’s still a significant chance of death, with a 10% mortality rate reported in recent studies. Interestingly, the chances of surviving in the hospital are greatly influenced by the patient’s blood pressure upon arrival. For instance, patients with lower blood pressure have a higher mortality rate when compared to those showing normal blood pressure levels. In fact, nearly half of those with blunt force injuries to the subclavian artery who arrived in shock did not survive.
To add, if we compare artery and vein injuries of the subclavian area, the vein injuries appear to have a higher mortality rate than artery ones.
Risk Factors and Frequency for Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)
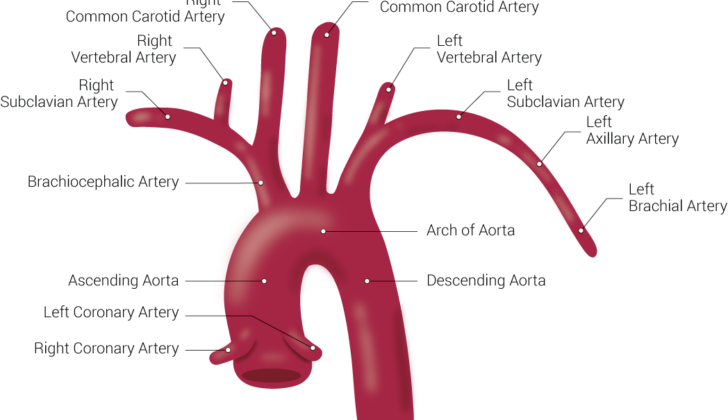
The subclavian vessels, which are located in a protected spot in the body, are usually damaged by puncture injuries such as gunshots or stabbings. Although less common, blunt force trauma can also result in injuries to these vessels. These types of injuries are becoming more frequently reported due to improved diagnosis from medical imaging. The type of injury often varies based on how it was caused.
- Wounds caused by puncture injuries often form something called a pseudoaneurysm.
- Injuries from blunt force trauma, such as a fall on an outstretched hand, commonly result in entire damage to the brachial plexus, a network of nerves that send signals from your spinal cord to your shoulder, arm, and hand.
- Injuries from puncture trauma are linked to a higher death rate, while blunt trauma often leads to more health complications due to damage to nearby structures.
- Another type of injury to the subclavian artery can happen accidentally during the placement of a central venous catheter, a tube placed in a large vein to give medication or fluids. However, this type of injury will not be covered in this overview.
Signs and Symptoms of Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)
When a patient arrives with a potential subclavian artery injury – an injury to the major artery in the upper chest, it’s crucial to start proper trauma support protocols immediately. Even so, the symptoms may not be apparent right away, especially if the injury is from blunt force trauma. In fact, less than a quarter of people with subclavian artery injuries display clear signs of vascular trauma from a physical exam.
Suspicions of a subclavian artery injury could be raised by signs such as:
- Missing upper arm pulses
- Brachial plexus palsy
- An audible rush of blood (bruit)
- A hematoma above the collarbone (supraclavicular)
- A fracture of the first rib
- Active bleeding
If a patient’s arm seems to be suffering from reduced blood flow (ischemia), this could indicate an associated injury to the brachial plexus – the nerve network that sends signals from your spinal cord to your shoulder, arm, and hand. This may need further exploration or repair. However, collateral circulation from another artery, the thyrocervicular trunk, could hide visible signs of ischemia in patients with a subclavian injury. Just because a patient has a pulse in their upper extremity (arm, wrist, or hand) does not mean they don’t have a subclavian artery injury.
Independent risk factors for subclavian artery trauma in patients with thoracic (chest area) trauma can include:
- A Glasgow Coma Scale score (a measure of consciousness) of less than 12
- An Abbreviated Injury Score (which assesses head injury) of greater than 3
- Presence of fractures in the collarbone or shoulder blade
A patient who has sustained abdominal trauma has a lower chance of also having a subclavian artery injury. However, it’s important to consider a subclavian artery injury in any patient with chest, neck, or shoulder trauma. Failure to diagnose or late diagnosis can lead to delayed bleeding, formation of a blood-filled bulge in an artery (pseudoaneurysm), or the development of a connection between an artery and a vein (arteriovenous fistula).
Testing for Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)
When a patient is in a critical condition, they should be quickly taken to the operating room. It’s extremely important to set up a robust intravenous (IV) line to start a large-scale blood transfusion. Besides giving them blood swiftly, it’s necessary to control the bleeding as soon as possible. If a patient has obvious neck or chest wounds and clear signs of blood vessel damage, applying direct pressure with a finger can block the bleeding until surgery can start. In some cases, a Foley catheter, which is a tube, can be filled with air and put into the wound to stop the bleeding. In extreme situations, a procedure called a resuscitative thoracotomy may be performed in the emergency department to control the bleeding through direct pressure on the chest cavity.
Identifying injuries to the subclavian artery, which is a major blood vessel in the upper chest, is often done during surgery as the patient’s unstable condition may prevent them from having scans. However, if the patient is stable and exhibits early signs of blood vessel injury, they can be scanned to confirm the diagnosis. A chest X-ray might show a fracture of the first rib, an abnormally wide gap in the middle of the chest (mediastinum), a blood clot at the top of the lungs (apical pleural hematoma), or unusual shadows along the path of the subclavian artery if it’s injured.
Angiography, which is a type of imaging test, is crucial for pre-surgery planning. It was once considered the best way to diagnose injuries to blood vessels like the subclavian artery. However, it is now less used because of possible complications and the length of the procedure. Now, practitioners prefer to use a computed tomography angiography (CTA). It provides the best details about injuries to the subclavian artery. If a penetrating injury causes the vessel to become blocked, the CTA will show no enhancement (or brightening) at the injury site. If the vessel is cut (transected), the CTA will show contrast material leaking out. And if a blunt trauma causes a dissection or tear in the artery that doesn’t block blood flow, the CTA will show unusual, linear defects with contrast filling the section of the artery beyond the injury.
Treatment Options for Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)
Minor injuries or blockages in the arteries might be handled without surgery in some patients who show no signs of limb ischemia or poor blood supply. Repeated imaging scans like CT scans or ultrasounds and blood-thinning medications can be used for management in such cases. However, for high-grade subclavian trauma, or more severe injuries to the arteries beneath the collarbone, surgery is usually required as not doing so can lead to poor outcomes.
These surgical procedures are complex due to the tricky location and anatomy of the affected arteries. Surgical complications tend to arise due to the often rapid blood loss during surgery, the location of the subclavian vessels and the surgeon’s unfamiliarity with these types of injuries.
During surgery, understanding the differences in anatomy between the right and left subclavian vessels is key to ensure a proper surgical approach. Quick control over the proximal and distal ends of the artery is crucial to prevent excessive blood loss. In the case of an unstable patient, a temporary shunt can be placed or the subclavian artery can be ligated, meaning tied off, until the patient is stable enough for definitive repair. One must be aware, this approach should be avoided in patients with a history of radiation therapy to the shoulder or significant tissue injury as it increases risk factors like potential limb loss. Also, the carotid-to-subclavian bypass, another surgical procedure, should be avoided because it significantly increases the risk of perioperative cerebral infarction, or stroke.
There are multiple surgical operation incisions that can be used to access the subclavian vessels, including median sternotomy, limited sternotomy, thoracotomy, supraclavicular, infraclavicular, or trap door incisions. The best incision depends on the injury’s location and brings with it its own potential advantages and disadvantages.
The repair of the injured subclavian vessels may involve the removal of clots and debris (debridement), end-to-end anastomosis or direct connection of the two ends, vein patch or grafting if a large segment of the artery is damaged. This repair and endovascular methods, where the procedure is carried out through the blood vessels themselves, are more frequently reported in recent literature.
The subclavian arteries are more commonly treated using endovascular methods for aneurysms, particularly for injuries in the left subclavian artery. Depending on the location of the injury, diverse sites such as the femoral, brachial or axillary arteries are used for access. Some conditions contraindicate this approach including a completely severed blood vessel, compression of the nerves of the upper limbs by a blood clot and injuries to the trachea or esophagus. However unstable patient conditions are not seen as a complete contraindication and sometimes a combination of surgical and endovascular approaches are used successfully.
What else can Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder) be?
Injuries to the chest, neck, or shoulder area can create confusing symptoms that might result in harm to major blood vessels. These could include important arteries located in the shoulder region, neck, under the collarbone, and the key vessels associated with the heart.
What to expect with Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)
For patients who reach the hospital after suffering subclavian injuries, chances of recovery are generally good if they undergo successful vascular repair. The most common complication after an injury to the subclavian artery is related to the brachial plexus, a network of nerves running from the neck to the arm. Even after successful repair of the artery and removal of any blood clots, many patients still suffer long-term nerve damage resulting in disability. In a study involving the repair of both nerve and artery injuries in the brachial region, only half of the patients had a good functional recovery.
In patients with injuries to the subclavian and axillary arteries, limb loss occurs in about 2.4% to 2.9% of cases. A review of data from the National Trauma Data Bank showed that the risk of limb loss in patients with these injuries was higher in patients with arterial and venous injuries, blunt trauma, and those treated with open surgery. Interestingly, brachial plexus injury was not an independent risk factor for limb loss.
Those who suffer trauma to the subclavian artery often have other associated injuries. These may include fractures to the spine, collarbone, or ribs, injuries to the trachea or bronchial tubes, or formation of blood clots that exert pressure on surrounding tissues. A fracture to the humerus (the bone in the upper arm) was found to have a higher risk of limb loss. During surgical intervention, the patient is preferably laid flat on their back to allow easy access to the abdomen, neck, and extremities to check for and manage these additional injuries.
Overall, compared to traditional surgery, the endovascular approach – a less invasive procedure that involves inserting a tube into the blood vessel – has been reported to reduce recovery time, cause less pain, and lower the incidence of bleeding and infection. However, most of this evidence is currently based on individual case reports and small studies. In addition, things like long-term results or the success rate of keeping the tube open are not well-defined. This could be a concern for younger patients. More comprehensive studies directly comparing traditional surgery and the endovascular approach are needed.
Possible Complications When Diagnosed with Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)
Damage to the nerves is a common side effect following injury to the subclavian artery, which is located below the collarbone. With such nerve damage, even with early treatment, there may be long-term issues. For this reason, doctors should thoroughly discuss possible long-term complications and expectations with their patients. Specific nerves, such as the recurrent laryngeal nerve and the phrenic nerve, can be accidentally hurt during surgery. Damaging these can lead to permanent hoarseness or other complications.
Care needs to be taken during surgery to ensure no extra damage is done. For instance, when the subclavian artery is being repaired, the vertebral arteries and the thoracic duct can also be at risk of injury. If the thoracic duct is injured during surgery, it should be tied off, and a drain should be put in place.
Those who undergo surgery to fix their subclavian artery via a minimally invasive procedure known as an endovascular approach, also face a list of potential complications such as:
- Bruising at the access site
- Formation of false aneurysms
- Narrowing of stent-graft
- Leakage around the graft
- Clot formation
- Reduced blood flow to the brain due to a stent covering the vertebral artery
People who’ve had this procedure often need long-term treatments to prevent blood clots, which can increase their risk of bleeding. If the vertebral artery becomes blocked, this can cause clots to form and travel along to the base of the brain. The endovascular approach can sometimes necessitate a secondary procedure, though very few patients require a switch to open surgery.
Preventing Subclavian Artery Trauma (Injury to Blood Vessels in the Shoulder)
By increasing awareness among emergency and hospital care providers about the need for quick diagnosis of subclavian artery injuries, patients can be transported to the right trauma centers for immediate treatment. This knowledge can help ensure that patients with such injuries have the best chance at a swift and successful recovery.