Overview of Inferior Vena Cava Filter
Pulmonary embolism, which is a sudden blockage in a lung artery, usually happens due to a blood clot that started in a leg (known as venous thromboembolism or VTE). This can be one of the main reasons for death in hospital patients. However, this can be prevented. The main way to do this is to give patients who are at high risk, certain medicines and techniques that help to thin their blood and prevent clots (this is called prophylactic anticoagulation).
If a patient is diagnosed with a blood clot condition such as VTE and pulmonary embolism, the first treatment usually given is a type of medicine that thins the blood known as pharmacological anticoagulation. However, in some cases, this treatment might not be suitable or may not work well. For these patients, a special type of device called an inferior vena cava (IVC) filter might be used. This helps to prevent pulmonary embolism by catching blood clots before they get to the lungs.
The first IVC filter available was the Greenfield inferior vena cava filter which came out in 1973. Nowadays, there are two types of IVC filters – permanent ones and those that can be removed. Since 2003 and 2004, when the Food and Drug Administration (FDA) approved removable IVC filters, their use has increased.
Research has shown that, in terms of death rates, there’s no big difference between patients with deep vein thrombosis (DVT), a type of blood clot condition, treated with IVC filters and those treated only with blood-thinning medication. Sometimes, IVC filters are used to prevent blood clots in high-risk patients, particularly if they can’t take blood-thinning medication. However, research hasn’t shown that these filters reduce the risk of death. In fact, they might increase the risk of blood clotting again and other complications.
Anatomy and Physiology of Inferior Vena Cava Filter
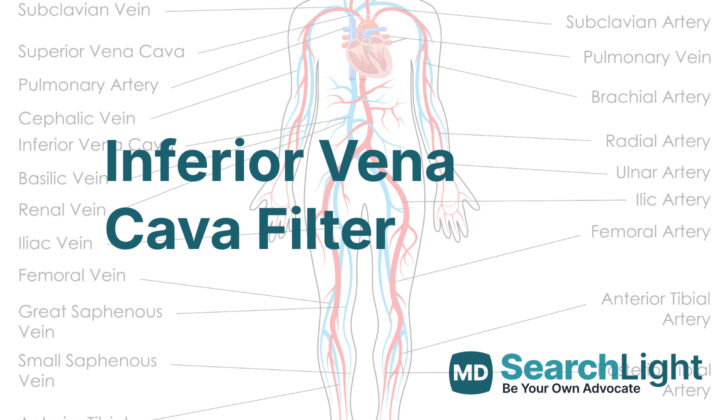
The inferior vena cava is a large vein that carries deoxygenated blood from lower parts of the body back to the heart. It’s important for doctors to understand the standard arrangement and variations of this vein to accurately place a filter and avoid complications. This vein begins to form when the common femoral vein, located under the groin ligament, becomes the external iliac vein. As it combines with the internal iliac vein, it forms the common iliac vein. These veins merge at the fifth segment of our lumbar spine (lower back), creating the inferior vena cava.
The inferior vena cava is divided into two parts by the joining point of the right and left kidney veins, which occurs at the first and second segments of the lumbar spine. Above this point, it’s called the suprarenal portion and below it is known as the infrarenal portion.
A dual inferior vena cava, which is present at birth in about 2% of people, might occur if the left main vein to the kidney doesn’t correctly reduce during development. With this abnormality, if a person gets blood clots in the lungs even after an inferior vena cava filter is put in place, further investigation is needed. Another common variation is a kidney vein that loops around the inferior vena cava, which makes placing the filter more difficult due to the close proximity of the kidney and hip veins. In these situations, it might be necessary to either place the filter above the kidney vein or use two filters in both hip veins. Doctors might mistakenly identify these congenital abnormalities as swollen lymph nodes in the abdomen area during imaging.
When an inferior vena cava is more than 28 millimeters wide, it is called a mega vena cava. While standard filters fit veins up to 28 millimeters wide, a larger filter – known as a bird’s nest filter – can accommodate veins up to 40 millimeters wide.
Why do People Need Inferior Vena Cava Filter
The American Heart Association and other expert medical groups recommend using a device called an inferior vena cava (IVC) filter for patients who have a condition called venous thromboembolism (VTE). VTE is a disease where blood clots form in the veins and can travel to other parts of the body. This can be very dangerous if a clot reaches the lungs, for example. This device is recommended if certain patients can’t be treated with drugs that prevent blood clotting, have complications that require stopping these drugs, or have new blood clots form even when taking these drugs correctly.
With the introduction of IVC filters that can be removed, there has been an increase in their use in patients who have additional health problems. These include patients with a high risk of getting new blood clots, those who are not taking their blood thinners correctly, patients with other severe heart and lung conditions, large movable blood clots in a deep vein of their legs, people at risk of complications from using blood thinners, and those with blood clots associated with cancer. Although the use of IVC filters has expanded, many studies have shown that a large number of these filters are never removed. Guidelines about using IVC filters in these ways are not as clear. Because there are not many trials comparing patient outcomes, doctors must use their best judgment when deciding to use IVC filters.
Doctors sometimes place IVC filters in patients to prevent blood clots from forming in the veins when they are at high risk. Such patients may be immobile for a long time (for instance, due to significant injuries or surgeries), or have certain medical conditions that increase the chances of blood clot formation, like cancer. In a study comparing patients at high risk for blood clots in the veins, those who received a permanent IVC filter initially had fewer instances of clots reaching the lungs. However, there were no immediate or long-term differences in the number of patients dying in the two groups. Two years after the procedure, more patients in the group with the IVC filter had recurring blood clots in the veins.
When a Person Should Avoid Inferior Vena Cava Filter
Generally, putting a filter in the inferior vena cava (a large vein that carries blood from your lower body to your heart) is thought to be safe. However, there are no definite reasons why someone should not have an IVC filter. But, there are certain situations where having an IVC filter might not be a good idea:
If a person has a severe problem with their blood that makes it hard for their blood to clot and stop bleeding, which is known as uncorrectable coagulopathy. In this case, having an IVC filter could be too risky. Also, if a person has bacteremia, an infection in the blood, they might not be suitable for having an IVC filter.
Equipment used for Inferior Vena Cava Filter
An Inferior vena cava (IVC) filter is a small device that’s used to prevent blood clots from reaching your lungs. It’s usually placed in a large vein, known as the inferior vena cava. A Catheter, which is basically a thin tube, is used during the process of placing the filter.
An X-ray machine and an Ultrasound machine are types of equipment that doctors use to clearly see the veins and the placement of the filter. These machines basically produce images of the inside of your body and help the doctor maneuver the catheter properly.
Local anesthetic is a type of medicine used to numb a specific area of your body during the procedure, so you don’t feel pain. An IV line is used to give you fluids or medicines directly into a vein. Sedatives are medicines that help you relax or sleep during the procedure.
Contrast dye is a special kind of dye that’s used to make the veins and the IVC filter show up more clearly on the x-ray images. This helps the doctor to see exactly where the filter needs to be placed and also confirm its right placement.
Who is needed to perform Inferior Vena Cava Filter?
An interventional radiologist is a special type of doctor who performs procedures using imaging to guide them. This can help in diagnosing or treating certain conditions without needing major surgery. A nurse will be there to assist during the procedure and help take care of you. A technologist is a healthcare professional who operates the medical imaging equipment, like the machines for x-rays or MRI scans. Together, these medical professionals will work hard to ensure your health and safety during the procedure.
Preparing for Inferior Vena Cava Filter
Before planning a medical procedure, it’s common to do a series of tests. Some tests might check your blood’s ability to clot, an important factor in preventing excessive bleeding during the procedure. Another key test might evaluate your kidney function, as it’s vital to know if your kidneys can efficiently process any contrast dye that might be used for imaging during the procedure.
It’s important that you prepare your body for the procedure. Doctors usually advise you to stop eating solid food eight hours before the procedure and to avoid drinking anything two hours before. This helps ensure a safer process. Also, you should discuss your current medications with the doctor. They may need to be adjusted to coordinate with the procedure.
Imaging tests, like a CT or MRI, can be very helpful in analyzing the main vein in your abdomen, known as the inferior vena cava (IVC), and the place where the medical tool will be inserted for the procedure. If you haven’t done such imaging tests before, doctors may carry out a special x-ray, known as cavography, which can analyze the IVC for abnormalities, its size, or if any blood clots are present. This helps ensure a safer operation and more successful outcome.
How is Inferior Vena Cava Filter performed
Inferior Vena Cava (IVC) filters are mainly inserted while the patient is in the hospital due to the active management needed for venous thromboembolism (VTE), which is a blood clot that starts in a vein. However, this can also be done as an outpatient procedure, meaning you can go home the same day. There are two main ways to place the IVC filter: through the internal jugular vein (in your neck) or the femoral vein (in your groin). Regardless of the access point, the right side is usually preferred as it has a direct and less tilted path to the IVC.
The right internal jugular vein is often the first choice due to its convenience, straightforward path, and reduced risk of interacting with a blood clot, if one is present in the femoral or iliac vein (vein in your pelvis). However, if you have a central venous catheter, require intubation (a tube inserted into your windpipe to aid breathing), or when using a type of imaging called intravascular ultrasound, the femoral vein approach is more appropriate.
There are different imaging techniques available to guide the doctor during the placement of the IVC filter. These include fluoroscopy (a type of x-ray that shows a continuous image on a monitor), duplex ultrasound (combines regular ultrasound and Doppler ultrasound, which shows blood flow), and intravascular ultrasound (an ultrasound inside the blood vessels). Fluoroscopy is the most commonly used imaging method. However, if you cannot be moved to the imaging suite, the doctor may use duplex ultrasound or intravascular ultrasound for bedside insertion of the filter.
After cleaning the access site and making it sterile, a small cut is made and a tube (catheter) is inserted, ideally while watching under fluoroscopy. The filter is then pushed along the catheter and put in place. The most common location for the IVC filter is just below the inflow of the renal veins (veins that carry blood away from the kidneys). This place is chosen due to the reduced risk of a blood clot blocking the renal veins. In some cases, such as pregnancy, presence of clot below the renal veins, and other conditions where putting the IVC filter below the renal veins is not possible, the filter can be placed in the IVC above the renal veins.
Possible Complications of Inferior Vena Cava Filter
Using an inferior vena cava (IVC) filter can cause some complications which can occur during the insertion procedure, afterwards, and during its removal.
During the placement procedure, the most common problems are bleeding and blood clotting. There can be other issues as well, such as: the filter tilting more than 15 degrees along its longitudinal axis inside the IVC; the filter moving more than 2cm from its original place; or the filter getting placed in a wrong place or incorrect orientation by the person doing the procedure. These errors can make the filter ineffective and difficult to retrieve later on.
After the procedure, problems can include: IVC blood clots resulting in pain and swelling in both legs or increased risk of a lung embolism, a condition when a blood clot reaches the lungs; kidney failure in case the blood clot extends up to the suprarenal IVC (an area above the kidneys); the filter penetrating the IVC or fragments of the filter breaking off and moving to the heart or lungs. To prevent the filters from moving, hooks were added to them, but this has led to an increased rate of IVC perforation.
As for filter removal, the longer it stays inside you before being removed, the higher the chance for complications. Common issues during retrieval include filter breakage and IVC injury, such as a tear to the inner lining. So, whenever possible, the filter should be removed as soon as it’s no longer needed.
Compared to permanent IVC filters, temporary, retrievable ones have been found to be more likely to cause complications. The most common issue with temporary filters is that they break. As for permanent filters, they tend to be incorrectly placed more often.
What Else Should I Know About Inferior Vena Cava Filter?
The use of a medical device called an inferior vena cava filter (IVC), a small metal device placed in a large vein to prevent blood clots from moving to the lungs, has been a topic of debate. This is due to a lack of extensive studies on its effectiveness. Doctors often decide to use IVC filters based on their own professional judgment and experience.
A notable research trial known as the PREPIC trial looked into the effectiveness of IVC filters. The trial failed to show that using IVC filters leads to better survival rates as compared to using blood thinners alone. While this trail found that IVC filters could help to stop additional lung clots (recurrent pulmonary embolisms) in the short term and long term, the trial also found that there was a significant increase in the recurrence of deep vein thrombosis (DVT), a type of blood clot, in individuals who received these filters. It’s clear from this finding that we need more comprehensive trials to determine if IVC filters are truly beneficial, when they should be used, and how different types of filters compare in terms of complications.
Blood clot-related conditions, known as Venous Thromboembolism (VTE), are a leading cause of death during pregnancy. Pregnant women have a higher risk of dying from these conditions in comparison to the general public. Warfarin, an anticoagulant or blood-thinning medication, is not recommended for these women because it can cause birth defects. Low Molecular Weight Heparin (LMWH), another blood-thinning medication, is a more appropriate choice. However, in patients at a high risk of bleeding, like those with a low-lying placenta (placenta previa) or recurrent VTE, a temporary or retrievable IVC filter could be considered. It’s crucial to remember that pregnancy can increase the size of the IVC vein and therefore the risk of the filter moving is increased.
The use of retrievable IVC filters has been on the rise. However, their retrieval has been a significant concern due to physicians not following the appropriate guidelines. The removal rates vary for numerous reasons, including geographical location and whether the filter was used for prevention or treatment. The retrievable filters are most commonly used in patients who cannot safely use blood thinner medications, but the reasons not to use blood thinners are often temporary. So, once it becomes safe to use blood thinners, the filters should be removed to decrease the risk of recurrent DVT and the formation of a blood clot in the IVC vein. Ideally, removal should happen within 30 days of insertion.