What is Dysbaric Osteonecrosis?
Dysbaric osteonecrosis is a condition where bone tissue dies due to lack of blood supply, and it often affects divers or workers who breathe compressed air or gas. It can raise the risk of bone fractures, depending on the size and location of the affected bone area. People with this condition often end up needing total joint replacement surgery. The hip joint, especially the top part of the thigh bone, is frequently affected, and it’s not unusual for it to occur on both sides.
What Causes Dysbaric Osteonecrosis?
While we don’t fully understand it yet, dysbaric osteonecrosis is believed to result from decompression sickness, which doesn’t cause any noticeable symptoms at first. What happens is, when a person undergoes decompression, the gas dissolved in their blood comes out and can form gas bubbles. These bubbles can damage the inner lining of blood vessels, leading to blood clots within the tiny blood vessels inside bones. This can cause venous blood clots, which can actually make arterial blood flow backwards and increase the overall pressure inside the bones.
In particularly high-risk areas, like near the top part of the thigh bone, this process of blood not reaching the bone parts can make the head part of the thigh bone to eventually break down. This could lead to tiny fractures in the cartilaginous tissue and ultimate collapse.
Risk Factors and Frequency for Dysbaric Osteonecrosis
Dysbaric osteonecrosis is a condition that varies widely in how often it occurs, depending largely on its quiet, gradual onset and the challenge of regularly screening those most at risk. Some research in Japan has found it in as many as half of all professional divers there, while the US military sees it in only about 2.5% of their divers. It’s generally more common in those who spend longer periods in environments with pressurized air and gas. It’s also more frequent in males, likely because they make up a larger percentage of those working jobs that expose them to these types of environments. Furthermore, this aligns with the fact that avascular necrosis from all causes is more common in men. Those with the disease often have multiple affected areas, and it usually shows up in people between the ages of 30 and 50.
- Dysbaric osteonecrosis shows up differently in different populations; as much as 50% in Japanese commercial divers, but just 2.5% in US military divers.
- The disease is more common in those exposed to pressurized air and gas for longer periods of time.
- As men tend to work in environments that involve exposure to compressed gases more often, they are more likely to develop the illness.
- This aligns with the general trend of men being more prone to avascular necrosis, a similar condition.
- The disease often affects multiple areas of the body.
- It generally presents in individuals aged 30 to 50.
Signs and Symptoms of Dysbaric Osteonecrosis
Joint injuries, especially those related to the hips and shoulders, are more likely to lead to painful symptoms. These problems can increase in severity when the patient moves or bears weight on the affected joints, and can even cause the joint surface to collapse or fracture. Pain may be felt not just in the joint but also along the limb and the range of motion might also be restricted. However, non-joint injuries, which usually occur in the long, straight parts of the thigh and upper arm bones, are less likely to lead to symptoms because they rarely affect the bone’s outer layer or cause fractures.
It’s crucial to have a thorough checkup focused on the joints to identify the cause of these bone lesions, as it could be due to cancer or other causes of bone tissue death (osteonecrosis) aside from this relatively rare condition. Special consideration should be given to whether the patient experiences pain when performing day-to-day activities.
Testing for Dysbaric Osteonecrosis
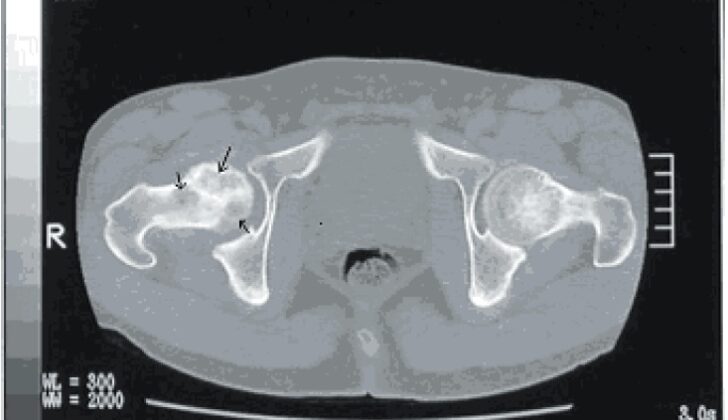
When a patient’s medical history and physical examination point towards a certain condition, x-rays are usually the first step in further investigation. X-rays can help doctors see what’s happening inside the body, particularly with the bones. MRI, or Magnetic Resonance Imaging, is another type of test that can provide more detailed information about any unusual spots or “lesions” that have been detected.
If the MRI results don’t give a clear answer, but doctors are still suspicious that something’s not right, they can use more advanced methods. These include bone scintigraphy and Single Positron Emission Computed Tomography. These tools are used more and more thanks to their high accuracy in confirming what the issue is.
CT scans or Computed Tomography scans, are also helpful as they provide a detailed view of the body’s anatomy. This can further clarify things and can be particularly helpful in planning for surgery, should it be needed, depending on the specific case.
Treatment Options for Dysbaric Osteonecrosis
Managing dysbaric osteonecrosis, a bone disease, can be quite tricky as the approach varies based on the specific location and characteristics of the bone lesion. When a bone lesion is first identified, it’s usually monitored with medical imaging to check for changes or possible self-healing.
Once a bone lesion is found, the patient should be referred to an orthopedic surgeon, a doctor who specializes in bone diseases. Large lesions particularly in the long bones of the body such as the thigh (femur) or shin (tibia), which cause a lot of walking pain, need immediate attention. The patient should be given crutches or a similar tool to avoid putting weight on the affected area until they see an orthopedic surgeon. This is done to prevent pathological fractures – these are fractures that occur in abnormal bone tissue. Preventive procedures like inserting a metal rod in the bone (intra-medullary nailing) might be considered to stop such fractures from happening.
For painful lesions located elsewhere, sometimes, treatment may involve removing the unhealthy bone tissue and replacing it with a bone graft – this is called curettage and bone grafting.
If the disease is in the upper part of the thigh bone (proximal femur), treating it can be more complex and depends on the stage of the disease. When the disease is in early stages (Ficat stage 0-II), oral medications called bisphosphonates can help prevent the collapse of the head of the thigh bone. Small, early-stage lesions have several surgical treatment options: core decompression with or without bone grafting (which relieves pressure within the bone and encourages new blood vessels growth), rotational osteotomy (a surgery that involves turning a portion of the bone to shift the weight-bearing surface), and vascularized, free-fibular, strut grafting (a procedure that uses a graft from the fibula bone) in young patients.
For patients aged over 40 with significant hip joint arthritis or younger patients with more progressive collapse of the head of the thigh bone or who already have a crescent sign (Ficat stage 3), a total hip replacement surgery could be the best option.
What else can Dysbaric Osteonecrosis be?
When doctors are trying to identify the root cause of a bone disease, they consider several possibilities:
- Cancer
- Fracture that’s not caused by disease
- Other reasons for bone tissue death, such as:
- Sickle cell disease
- Systemic lupus (an autoimmune disease)
- Viral infections
- HIV medication side effects
- Exposure to radiation
- Blood diseases
- Marrow-related diseases like Gaucher’s disease
- Alcoholism
- Use of steroids
- Conditions that cause blood to clot more than usual
What to expect with Dysbaric Osteonecrosis
The outcome or prognosis of a medical condition can change depending on several factors. These factors include the location and size of the lesion (injured tissue) and the patient’s age or overall health. Patients who have small lesions that don’t affect major joints may not experience any symptoms. However, patients with large lesions near their joints might have a poor overall health outlook and limited mobility without significant surgery.