What is Multidirectional Shoulder Instability?
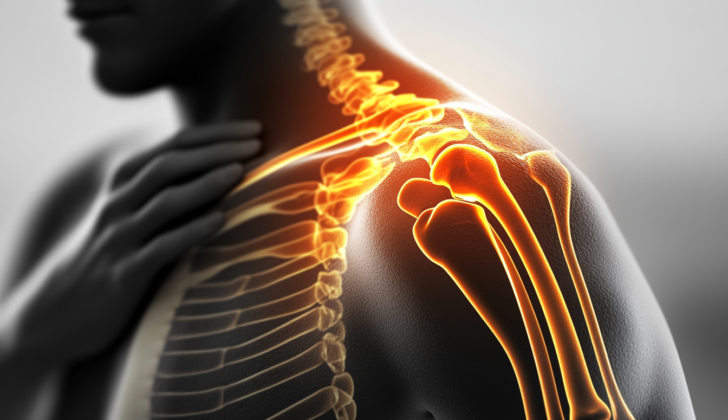
Multidirectional instability (MDI) of the shoulder is a complex condition that was first recognized in 1980. It refers to a state where the shoulder joint becomes unstable in two or more directions. The shoulder joint is unique because it allows for a lot of movement – it’s actually the joint with the most range of mobility in the human body. However, there’s a trade-off: the joint’s stability decreases as its mobility increases. This balance between movement and stability is crucial and needs careful management to prevent instability.
One of the main functions of the shoulder is to move the hand in space. Different activities demand different levels of mobility and stability from the shoulder joint. For example, swimming requires more mobility, while weight lifting requires more stability. The shoulder joint achieves its stability through two types of stabilizers: dynamic and static ones. The dynamic stabilizers include muscles and tendons around the shoulder, while the static stabilizers include structures in the joint itself, along with the negative pressure inside the joint. Shoulders become unstable and show symptoms when the top of the arm bone (the humeral head) moves beyond the limits set by a part of the shoulder joint known as the glenoid labrum complex. This can happen due to issues with either the static or dynamic stabilizers.
Initially, it was thought that shoulder instability could be divided into just two types. The first, known as TUBS (Traumatic Unilateral with Bankart lesion treated Surgically), involves a specific type of shoulder injury treated using surgery. The second type, AMBRI (Atraumatic, Multidirectional, Bilateral), is usually resolved with rehabilitation or a certain kind of surgery (Inferior capsular shift). However, these categories were too simplistic and didn’t cover all types of shoulder instability. As we learned more about MDI, these classifications were changed to better reflect the condition’s complexity.
What Causes Multidirectional Shoulder Instability?
Multidirectional instability refers to a condition where the shoulder can move too freely and possibly dislocate in multiple directions. It can develop through two different ways. The first way is through repeated minor injuries that often occur in athletes involved in overhead sports like baseball, volleyball, gymnastics, and swimming.
The second way happens because of conditions that make ligaments more flexible than normal, causing them to have too much movement. Some of these conditions include Ehlers-Danlos syndrome (a condition that affects the skin, joints and blood vessels), Marfan syndrome (which impacts the body’s connective tissue), osteogenesis imperfecta (also known as brittle bone disease), and benign joint hypermobility syndrome (where joints move beyond the normal range).
Risk Factors and Frequency for Multidirectional Shoulder Instability
Multidirectional instability (MDI) of the shoulder is a condition whose exact occurrence is hard to determine, due to the varying ways it can be classified and diagnosed. Usually, MDI is most common in people in their 20s and 30s, then less typical in those over 40. This decrease in older age is related to the natural hardening of the shoulder joint and loss of flexibility in the tissues. It’s important to note that while MDI is more commonly seen in physically inactive women with weak muscles, it can affect anyone, including both male and female athletes.
Signs and Symptoms of Multidirectional Shoulder Instability
Multidirectional instability of the shoulder is a difficult condition to diagnose because it doesn’t have clear, distinctive symptoms. It typically starts with unspecific, activity-related shoulder pain that gradually gets worse, especially when carrying heavy objects or doing overhead activities. Some people may also notice a decrease in strength or athletic performance, but they don’t often complain about instability. However, healthcare providers should be mindful of people who can dislocate or sublux their shoulder at will, as there might be a mental health aspect involved that should be addressed during treatment.
To diagnose multidirectional instability, a physical exam is usually performed. This involves testing for instability in at least two different directions (anterior, posterior, or inferior). One common finding is the ‘sulcus sign,’ which indicates a loose shoulder joint. This is tested by pulling the arm downwards and creating a shallow dip under the shoulder bone. If this dip is more than 2 cm deep, it might indicate an abnormal looseness, especially if it triggers the patient’s symptoms. The patient might also experience increased rotation with the arm down.
Patients might feel uneasy when their shoulder is lifted and rotated externally — a sensation that is tested for with the ‘apprehension’ test. If applying a gentle pressure on the upper arm bone during this test relieves the uneasy feeling, it’s a sign of true anterior instability. A load-and-shift test, where the healthcare provider applies pressure to the shoulder joint while the patient is relaxed, might also be positive.
In patients with multidirectional instability, it’s also important to check for looseness in other joints. The Beighton criterion is used for this, which assigns points based on how much beyond a normal range of motion certain joints can move. Points are given for:
- Elbows or knees that extend beyond 10 degrees
- Small finger joints that extend beyond 90 degrees
- Thumbs that can touch the forearm of the same side
- Both palms being able to touch the floor while bending at the waist with straight knees
If a person scores 4 or more points out of 9, it could suggest a hyperlaxity disorder. While this alone doesn’t confirm the diagnosis, it signals to the clinician that this could be contributing to the instability. Some people with these conditions may never experience shoulder instability, but it’s still important to consider it as it can affect the outcome of treatment interventions.
Testing for Multidirectional Shoulder Instability
If you’re suspected of having multi-directional instability (MDI), which is a condition where your shoulder can easily dislocate, the first thing your doctor will do is examine your shoulder. However, additional tests are necessary to fully understand what is going on, starting with several types of X-ray images. These can include images of your shoulder taken from the front, side, and angles that show the shoulder blade. X-rays can often appear normal in people with MDI, but they are used to check for other issues that could be contributing to the problem, such as an irregular shape of one of the shoulder bones or specific types of bone damage.
Your doctor may also order an MRI (Magnetic Resonance Imaging) scan with a dye injection to get a more detailed view of the shoulder. This scan can highlight issues in the lower part of the shoulder joint capsule, where laxity or looseness might occur. Also, MRI can be used to investigate further any possible Bankart lesions, Kim lesions, or deterioration of the shoulder socket. Bankart and Kim lesions are specific types of damage that can occur to the part of the shoulder joint called the labrum, and they often show up in people with shoulder instability.
Treatment Options for Multidirectional Shoulder Instability
If you are diagnosed with Multidirectional Instability (MDI), a condition where the shoulder is too loose and may easily slip out of place, the first step in treatment is to understand your daily activities and demands. This is due to the fact that some sports can benefit from a certain degree of shoulder flexibility. As such, there’s no “one-size-fits-all” treatment for MDI. Instead, the treatment is tailored to meet your needs and expectations.
MDI often occurs when the balance between two types of shoulder stabilizers (parts that hold your shoulder in place) is disrupted: dynamic and static stabilizers. Therefore, the first line of treatment typically involves physical therapy to strengthen your dynamic stabilizers. In simple terms, these are the muscles that support your shoulder, including your rotator cuff and muscles around your shoulder blade. A specific type of exercise known as ‘closed kinetic chain’ exercises are used in therapy. These exercises aim to teach your muscles to work together in harmony, enhancing the stability of your shoulder.
Before considering more aggressive treatments, you should continue this physical therapy for at least 3 to 6 months. This works because as we age, our shoulder joint naturally gets stiffer, reducing symptoms of MDI. As the body reaches full growth, symptoms of MDI often decrease, and that’s why sticking to therapy long-term is strongly encouraged.
If physical therapy doesn’t work, surgical procedures like open or arthroscopic (minimally invasive) stabilization might be considered. These procedures could involve mechanisms to tighten the shoulder, such as capsular shift, closing a part of the shoulder called the rotator interval, or reducing excess tissue in the shoulder capsule. In some cases, for patients with certain types of disorders affecting the connective tissue, a capsular allograft reconstruction – a procedure where tissue from a donor is used to repair your shoulder – might be used. If any other issues are found in the “glenoid” or “labrum,” areas in your shoulder joint that could add to instability, these should also be addressed during the same procedure.
What else can Multidirectional Shoulder Instability be?
If you are experiencing unclear shoulder pain that seems to be connected to physical activity, the root cause could be a condition known as Multidirectional Instability (MDI). That said, diagnosing MDI could be challenging because other conditions can cause similar symptoms. These conditions include:
- Unidirectional instability – instability in one direction
- Cervical spine disease – a condition that affects the neck
- Os acromiale – a condition where a part of the shoulder blade is not completely fused
- Thoracic outlet syndrome – pressure on the nerves or blood vessels under the collarbone
It’s important to pinpoint the exact cause of the shoulder pain as each of these conditions requires a different treatment approach.
What to expect with Multidirectional Shoulder Instability
Multidirectional instability, or MDI, usually has a good outcome. MDI symptoms are related to how strong your shoulder is – so, the stronger your shoulder, the fewer symptoms you’ll experience. This is why physical therapy that focuses on strengthening the muscles around the shoulder blade and shoulder is encouraged. Doctors typically recommend trying this therapy for at least 3 to 6 months before considering surgery.
Possible Complications When Diagnosed with Multidirectional Shoulder Instability
Most issues related to multi-directional instability (MDI) arise from its treatment. This includes problems such as decrease in range of motion, arthritis caused by capsulorrhaphy (a surgery to tighten soft tissues), weakness of subscapularis muscle (a muscle in the shoulder blade), injury to the axillary nerve (a nerve in the shoulder), and a return of instability. It often happened that the instability returned after a specific procedure of capsulorrhaphy that used heat which caused permanent damage to the shoulder capsule, thus this procedure is no longer recommended and is only referred to for historical study.
Past procedures like Magnuson-Stack or Putti-Platte led to arthritis, as these treatments tightened the capsule excessively and placed pressure on the humeral head (a part of the arm bone) into the glenoid (part of the shoulder joint), which resulted in an accelerated rate of cartilage wear.
Lastly, a common problem after open procedures is the deficiency of the subscapularis muscle. In these procedures, the subscapularis tendon is removed for exposure and then repaired. However, if the subscapularis doesn’t heal properly, it leads to its deficiency.
Common Problems:
- Decrease in motion range
- Arthritis caused by capsulorrhaphy
- Weakness of the subscapularis muscle
- Axillary nerve injury
- Return of instability
- Cartilage degradation
- Subscapularis deficiency
Recovery from Multidirectional Shoulder Instability
After a shoulder operation, the typical healing process lasts about 4 to 6 weeks, during which the shoulder should be kept as still as possible. After 6 weeks, patients can gradually begin simple shoulder movements, including daily tasks, but should avoid moving their shoulder more than 45 degrees sideways or in a rotation. Around the 10th week, they can start gentle stretching exercises to improve the range of motion in their shoulder.
Beginning the 16th week, strength training can be started to regain shoulder strength. However, returning to sports, particularly those that involve physical contact, shouldn’t happen until the shoulder has completely healed, or at least regained 90% of its original strength. This usually takes between 9 to 12 months after the operation.
Preventing Multidirectional Shoulder Instability
People with multidirectional instability (MDI), a condition where the shoulder can dislocate in multiple directions, should understand that their symptoms can become more noticeable if their shoulder muscles weaken. Therefore, it’s crucial to keep up with regular shoulder-strengthening exercises even when they don’t feel any discomfort, as the symptoms are likely to return if the shoulder loses strength.
Patients should be prepared for the fact that recovery generally requires a long period of physical therapy, rather than a quick surgical solution. This therapy helps improve the stability and function of the shoulder and can effectively treat the condition in most cases.
Finally, learning about which activities worsen their symptoms can be beneficial for these patients. They can then make lifestyle changes that might help reduce their discomfort and improve their shoulder stability, limiting the disruption this condition causes in their daily lives.