What is Myasthenia Gravis?
Myasthenia gravis (MG) is a common condition that affects the connection between the nerves and muscles, specifically targeting the muscles in your eyes, throat, and limbs. People with MG often experience fluctuating weakness that tends to be more pronounced later in the day. This weakness happens because the body starts producing harmful antibodies which impede the transmission of electrical signals from the nerves to the muscles, causing the muscles to weaken.
A range of situations can trigger MG – such as infections, vaccines, surgeries and certain medications. The condition can lead to a variety of complications. One such complication is a myasthenic crisis, a sudden severe weakness causing breathing to become too difficult, thereby requiring intensive care. Long-term side effects from the medication used to treat MG can also lead to complications such as opportunistic infections and the development of abnormal growths in the body’s lymph nodes (lymphoproliferative malignancies).
Understanding the cause, symptoms, treatment options, and complications of MG is necessary to ensure patients receive the best possible care and treatment outcomes.
What Causes Myasthenia Gravis?
Myasthenia gravis is an autoimmune disorder, which means the body’s immune system mistakenly attacks its own healthy cells. This usually happens in people with a certain genetic makeup. There can also be triggers that spark the condition, such as infections, vaccinations, surgeries, or certain medications.
This disease primarily targets proteins at the place where nerves and muscle meet, called the neuromuscular junction (NMJ). The body ends up producing harmful substances called autoantibodies against these proteins. The proteins affected include nicotinic acetylcholine receptors (n-AChR’s), muscle-specific kinase (MuSK), and lipoprotein-related protein 4 (LPR4). These proteins are important for maintaining the connection between nerves and muscles.
Interestingly, about 10% of people with myasthenia gravis also have a growth on their thymus gland, known as a thymoma. This gland plays a role in producing the harmful autoantibodies.
Myasthenia gravis is not a one-size-fits-all disease – it varies from person to person. This is why it’s grouped into different types based on the symptoms and the specific autoantibodies involved. Each group can respond differently to treatment, which is important to know for planning the best care strategy:
- Early-onset MG: The disease starts before the age of 50 and there’s enlargement of the thymus gland
- Late-onset MG: The disease starts after the age of 50 and there’s shrinkage of the thymus gland
- Thymoma-associated MG
- MG with anti-MuSK antibodies
- Ocular MG: Only the muscles around the eyes are affected
- MG with no detectable AChR and MuSK antibodies
Risk Factors and Frequency for Myasthenia Gravis
Myasthenia gravis is a condition that is not very common, affecting about 20 in every 100,000 people in the US. It’s more common in women under 40 years old, and more common in men over 50 years old. While it’s pretty rare in Western countries for kids to get this condition, it’s more common in Asian countries, with about half of the patients being under 15 years old. The main symptom is weakness in the muscles around the eyes.
- Myasthenia gravis affects about 20 in every 100,000 people in the US.
- It is more commonly seen in women under 40 and men over 50.
- Childhood myasthenia gravis is rare in Western countries but common in Asian countries.
- About half of the patients in Asia are under 15 years old.
- The predominant symptom is weakness in the muscles that control eye movements.
Signs and Symptoms of Myasthenia Gravis
Myasthenia Gravis (MG) is recognized by a muscle weakness that changes in intensity, gets worse with physical exertion, and gets better with rest. This weakness can be triggered by many things such as infections, surgery, emotional stress, and various medications. In patients with MG, you might notice signs like coughing after swallowing, slower eating, hoarseness, feeling tired going upstairs, or making more mistakes when writing or typing. These symptoms are especially noticeable at the end of the day.
The most common symptoms include the following:
- Eye muscle weakness: About 85% of patients experience this at first. They might complain of double vision, droopy eyelids, or both. These symptoms then progress and can cause MG that affects the throat, spine, and limb muscles in 50% of patients within two years.
- Throat muscle weakness: This could be the first symptom in 15% of patients. They may have difficulty chewing, choke more often, have trouble swallowing, a hoarse voice, and speech problems. Weak facial muscles can cause a lack of facial expression, and weakness in the neck muscles can lead to a drooping head.
- Arm and leg weakness: Usually the muscles in the shoulder and hip are more affected than muscles in the hand and foot, with the arms more affected than the legs.
- Myasthenic crisis: This is an emergency situation that happens when the breathing muscles are too weak. There are no symptoms related to the internal parts of the body like heart palpitations or issues with the bowel or bladder, as MG only involves the receptors that control muscle movement.
During a physical exam, the doctor might not see any muscle weakness because it can come and go. However, if the muscles are used continuously or many times, the weakness might be noticeable. The eyes, reflexes, and sense of touch are usually normal in patients with MG.
MuSK MG is a type of MG that affects mostly women. It’s different from the usual type of MG because it mostly affects the throat, face, and neck muscles. It does not often affect the eye muscles. Myasthenic crisis is also frequent in the MuSK MG.
The Myasthenia Gravis Foundation of America (MGFA) classifies MG into five categories based on the symptoms and how severe the disease is. Each category has a different outcome or response to treatment.
- Class I: Only the eye muscles are affected.
- Class II: Other muscles are mildly affected. Eye muscles of any degree may also be affected.
- Class III: Other muscles are moderately affected. Eye muscles of any degree may also be affected.
- Class IV: Other muscles are severely affected. Eye muscles of any degree may also be affected.
- Class V: This class includes cases where a breathing tube has been inserted, with or without mechanical assistance to help with breathing, except when used after surgery.
Testing for Myasthenia Gravis
Myasthenia Gravis (MG) is primarily diagnosed through a doctor’s examination, but lab tests and procedures can help confirm the diagnosis. In a majority of MG cases, a specific test for anti-AChR Ab can confirm the disease, as this antibody is found in approximately 80% of generalized MG patients and 50% of patients with a type of MG that primarily affects the eyes (ocular MG).
For a small percentage (5% to 10%) of patients who don’t carry anti-AChR are found to have anti-MuSK antibodies. There are also a small number of patients that have both antibodies. Some patients, who test negative for either of these antibodies, will exhibit anti-LRP4 antibodies. Around 30% of MG patients possess anti-striated muscle antibodies, which can be a useful marker for thymoma (a type of tumor), especially in younger patients.
Some tests, such as the repetitive nerve stimulation (RNS) test and single-fiber electromyography (SFEMG), are performed for patients who test negative for these antibodies. These tests assess the functioning of the communication points between nerves and muscles.
The RNS test is done by stimulating the nerve repeatedly, which depletes a chemical called acetylcholine, producing a reduced electrical signal. If the electrical signal reduces by 10% or more after repeated stimulation, it suggests MG.
As for the SFEMG, it measures how nerve signals behave in individual muscle fibers, affecting the difference in time it takes for two signals to fire. The presence of MG can cause this difference or “jitter” to increase. This test is considered to be the most sensitive diagnostic test for MG.
The Edrophonium test is another tool in diagnosing MG. Edrophonium is a medication that makes more acetylcholine available in the body. The test is specifically useful for diagnosing ocular MG. The medication is administered intravenously, and then the doctor will check for improvements in symptoms like eyelid drooping or double vision. This test has a 71% to 95% accuracy rate for diagnosing MG.
An alternative test called an ice-pack test is used when the Edrophonium test is not suitable. For this test, an ice-pack is placed over the eye for 2-5 minutes, and then the doctor checks if there is any improvement in drooping eyelids. However, this test is not for checking the condition of extraocular muscles.
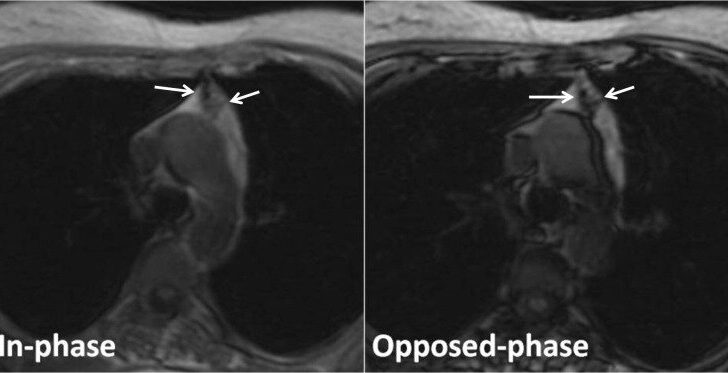
For patients diagnosed with MG, imaging techniques like CT scans or MRI scans of the chest are done to check for thymoma. For those with symptoms limited to the eyes, an MRI of the brain and orbits is conducted to check for any localized mass lesions.
Since MG often coexists with other autoimmune disorders, doctors often recommend testing for anti-nuclear antibodies (ANA), rheumatoid factor (RF), and thyroid functions.
Treatment Options for Myasthenia Gravis
The primary treatments for Myasthenia Gravis (MG), a neuromuscular disorder, include cholinesterase enzyme inhibitors and immunosuppressive agents. These drugs help to manage symptoms, but if they aren’t effective, or if the symptoms need to be quickly relieved (as in a myasthenic crisis), other treatments like plasmapheresis or intravenous immunoglobulins can be used.
There are four main strategies for managing MG:
Firstly, symptomatic treatment uses Acetylcholinesterase inhibitors. These increase the level of acetylcholine, a chemical that helps nerve cells communicate, in the neuromuscular junction (where nerves connect with muscles) by preventing the chemical’s breakdown. Pyridostigmine bromide is often used because it lasts longer in the body, although if it causes any problems, ambenonium chloride may be used as an alternative. If you have a particular type of MG, known as MuSK MG, these drugs may not work as well for you.
Secondly, if the symptoms continue even after taking pyridostigmine, immunosuppressive treatments might be necessary. These include steroids, such as prednisone, prednisolone, and methylprednisolone, and drugs like azathioprine. Second-line agents, used when the first line isn’t effective, include cyclosporine, methotrexate, mycophenolate, cyclophosphamide, and tacrolimus. More recently, monoclonal antibodies, such as rituximab and eculizumab, that help your immune system fight off diseases, have been used in cases of drug-resistant MG, but their effectiveness is still being studied.
Thirdly, intravenous immunoglobulins (IVIG) and plasmapheresis (a treatment that filters the blood) are recommended when a patient needs to be stabilized before a procedure. They are also used to treat a myasthenic crisis (a severe form of MG) and in cases that do not respond to immunosuppressive drugs because they usually have a rapid effect.
Lastly, a thymectomy, a surgery to remove the thymus (a small organ that is part of the immune system), may be recommended. This surgery is used for any type of MG where there’s evidence of a tumor in the thymus. It’s also used for non-cancerous forms of the disease, but is not recommended for a type of MG known as MuSK MG or for a form of the disease that only affects the eyes.
What else can Myasthenia Gravis be?
When a person shows signs of myasthenia gravis, a condition that weakens the muscles, doctors need to consider other health problems that could cause similar symptoms. These include:
- Lambert-Eaton syndrome, which causes changing muscle weakness that gets better with exercise, rather than worse. This health issue can be linked to cancer, especially a type called small-cell lung cancer. It affects areas in the nerve cells responsible for carrying signals to the muscles.
- Cavernous sinus thrombosis, which presents with consistent eye issues, sensitivity to light, eye swelling, and headaches. It can develop suddenly or quickly and can be caused by infection or blood clotting disorders.
- Brainstem gliomas are malignant, or cancerous, tumors that cause weak or numb muscles, balance issues, and even seizures, depending on where they’re located. Symptoms are usually constant and may also involve headaches and signs of high pressure within the skull.
- Multiple sclerosis may show any brain-related sign that can flare up, carry on over time ranging from hours to weeks, due to a condition where the protective covering of nerve fibers in the central nervous system gets damaged. These signs may include weakness, numbness, and cognitive and behavior changes. Muscle weakness could exist in one or both sides of the body and can be associated with signs of nerve damage, such as increased reflexes, muscular tension, and a positive Babinski sign, an abnormal foot reflex.
- Botulism is a bacterial infection that can cause drooping eyelids, double vision, overall weakness, and abnormal eye pupils, along with other body-wide symptoms. It can occur due to infection from eating food contaminated with the bacteria or honey, particularly in the case of infants.
- Tick-borne diseases can bring about increasing paralysis and breathing problems, lowered reflexes due to toxins from tick saliva, and usually come with a few overall body symptoms. They could sometimes cause eye movement disorders and symptoms related to the brainstem.
- Polymyositis and dermatomyositis cause weakness in muscles close to the trunk of the body and are often linked with pain. The actual muscles are what get inflamed in these conditions.
- Graves ophthalmopathy, which can cause the upper eyelid to retract and the gap between the eyelids to widen. It’s caused by the body’s immune system mistakenly attacking parts of the eye.
What to expect with Myasthenia Gravis
Today, most patients with Myasthenia Gravis (MG) – a condition that causes muscles to weaken – can expect to live nearly as long as they would without the disease, thanks to available treatments. It’s a far cry from 50 years ago when the condition was lethal in 50% to 80% of cases. Now, the mortality rate has dropped significantly to around 4.47%. However, MG can still lead to health problems including aspiration pneumonia, which is caused by inhaling food or drink into the lungs, and side effects from the drugs used to treat the disease.
Research has shown certain symptoms, and the results from blood tests and imaging scans can help predict how the disease may affect a patient. For instance, people who are older when they get MG, have high levels of certain antibodies in their blood, or have a certain type of tumor called a thymoma (mostly benign) are more likely to see their condition progress. Additionally, having two specific symptoms – drooping eyelids (ptosis), and double vision (diplopia) – when first diagnosed with MG makes it more likely that the disease will progress.
On the brighter side, early treatment with drugs that suppress the immune system, like corticosteroids and azathioprine, can lower this risk. Furthermore, being diagnosed at a young age (<40 years), undergoing early thymectomy (surgery to remove the thymus gland), and taking prednisolone can reduce the chances of the disease relapsing. However, people who have certain antibodies in their blood coupled with another autoimmune disease may experience the disease relapsing more frequently.
Possible Complications When Diagnosed with Myasthenia Gravis
Myasthenia gravis can lead to a serious condition called a myasthenic crisis. This usually happens due to infections, stress, or sudden illness.
Treatment for myasthenia gravis can also bring its own set of complications due to the long-term use of steroids. Some of these complications include weakened bones (osteoporosis), high blood sugar (hyperglycemia), cataracts, weight gain, high blood pressure (hypertension), and a condition where the bone tissue in the hip dies due to lack of blood supply (avascular necrosis of the hip). There’s also a chance of cancer related to blood cells formation (lymphoproliferative malignancies) and opportunistic infections like systemic fungal infections, tuberculosis, and Pneumocystis carinii pneumonia due to the long-term usage of drugs that suppress the immune system.
On the other hand, cholinergic crisis is another condition that may occur due to the excess presence of a chemical messenger (ACh) at nerve cell receptors due to a medication used for treatment, cholinesterase inhibitors. Symptoms of this may include cramps, excessive tear production, increased salivation, muscle weakness, uncontrolled muscle twitching (muscular fasciculation), paralysis, diarrhea, and blurred vision.
Common Complications:
- Myasthenic crisis
- Osteoporosis
- Hyperglycemia
- Cataracts
- Weight gain
- Hypertension
- Avascular necrosis of the hip
- Lymphoproliferative malignancies
- Opportunistic infections
- Cholinergic crisis
Preventing Myasthenia Gravis
It’s crucial for patients to avoid triggers that could aggravate their condition. These triggers can include infections, excessive physical effort, emotional stress, worsening of existing health problems, or certain medications such as aminoglycosides, fluoroquinolones, and beta-blockers.
Patients are encouraged to take their prescribed medications as instructed and to avoid starting new medicines without speaking to their healthcare provider first. It’s also important for patients to understand the potential complications of their condition. If they notice any changes or worsening symptoms, seek medical help immediately.
Using a medical identification bracelet that notes they have myasthenia gravis – a neuromuscular disease leading to fluctuating muscle weakness and fatigue – is a good idea. This can help medical professionals quickly identify their condition in case of an emergency.
Engaging in habits that promote good health can additionally help prevent infections. Simple measures like handwashing or getting the yearly flu shot can greatly reduce the risk of catching infections. Taking such precautions is very important for those managing this condition.