What is Osgood-Schlatter Disease?
Osgood Schlatter disease, also known as osteochondrosis, is a frequent reason for knee pain in growing children and teenagers who play sports. It particularly affects those participating in sports like basketball, volleyball, sprinting, gymnastics, and football.
Usually, this condition starts with mild knee pain that gets worse with certain activities like jumping and sprinting. People with the disease will often feel discomfort at the point where the kneecap (patellar) tendon attaches to the shinbone (tibia). However, this is typically not due to any injury and will get better on its own over time.
The amount of pain generally determines the treatment needed, most commonly this is a combination of rest, applying ice to the area, using over-the-counter pain relievers, and making changes to physical activity. This can also include a routine of stretching exercises to correct any related posture or movement issues.
While Osgood Schlatter disease is usually not harmful in the long run, the recovery process can be long, which may prevent children and teenagers from taking part in their favourite sports activities for a while. The condition usually develops gradually and is commonly related to repetitive knee activities over time. And there’s often tenderness over the top of the shinbone.
What Causes Osgood-Schlatter Disease?
The patellar tendon, which is made of cartilage, attaches at a spot on the lower leg bone called the tibial tubercle. This tubercle becomes bone-like in girls between ages 10-12 and in boys between ages 12-14. It’s during this bone growth stage that a condition known as Osgood Schlatter disease often develops. The general belief is that this disease arises from ongoing stress on the tubercle resulting in small blood vessel tears, fractures, and inflammation – leading to swelling, pain, and tenderness.
Osgood Schlatter disease is a type of injury that can happen due to excessive use of the knee area and is common in active teenagers. The condition is linked to repeated stress and minor injury from the powerful tug of the patellar tendon where it connects to the relatively soft bone formation of the tibial tubercle. This pulling force can cause irritation and in severe instances, it can partially tear away the apophysis or the part of the tibial tubercle that’s still growing. The force is heightened with more vigorous activities and particularly after periods of fast growth. In rare cases, an injury can lead to a complete breakaway fracture. Known contributing factors include having tight quadriceps and hamstring muscles or other signs of misalignment in the knee extension mechanism.
Risk factors for this condition include:
* Being male
* Being in certain age groups: boys 12-15, girls 8-12
* Experiencing a growth spurt
* Partaking in repetitive activities like jumping and sprinting
Risk Factors and Frequency for Osgood-Schlatter Disease
Osgood Schlatter disease is frequently responsible for knee pain in young athletes, particularly during their growth spurts. It typically occurs in boys between the ages of 10 and 15 and in girls between the ages of 8 and 13. The disease is more common in boys, as well as in young athletes who take part in sports that require running and jumping. In adolescents aged 12 to 15, almost 10% have the disease, with boys being affected slightly more often. The disease can affect both knees in 20 to 30% of the patients.
- Osgood Schlatter disease is common among young athletes and can cause knee pain.
- It often starts when kids go through growth spurts, typically between ages 10-15 for boys and 8-13 for girls.
- The disease is more common in boys and in young athletes who run and jump in their sports.
- About 10% of adolescents aged 12-15 have this disease, with a bit higher percentage in boys (11.4%) than girls (8.3%).
- This disease can affect both knees in 20% to 30% of the patients.
Signs and Symptoms of Osgood-Schlatter Disease
Kids aged between 8 and 15 may experience pain in their knees associated with swelling, which can occur in one or both knees. Initially, the pain starts off as a dull ache over a specific part of the shin bone known as the tibial tubercle and tends to increase with physical activity. This kind of pain often comes on gradually without any prior injury.
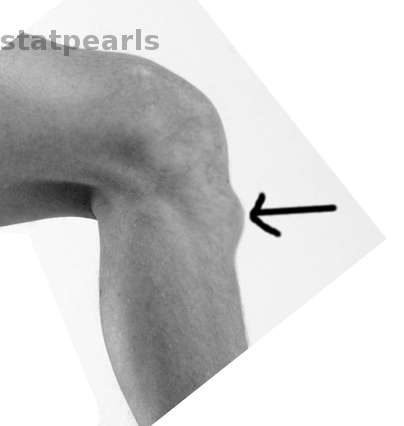
The pain usually eases with rest and ends within a few minutes to hours after stopping the activity or sport that caused it. Certain activities like running, jumping, experiencing direct trauma to the knee, kneeling, and squatting can make the pain worse. The shin bone may have a larger than normal bump at the tibial tubercle, which is usually sore to touch.
These kids might also have difficulty flexing their thigh and hamstring muscles. The knee pain can be recreated by pushing against resistance with a straightened knee, and bending the knee actively or passively.
- Pain in one or both knees
- Dull ache over the tibial tubercle
- Pain intensifies during physical activities
- Pain eases with rest
- Pain worsens during running, jumping, direct knee trauma, kneeling, and squatting
- Enlarged bump on the shin bone
- Difficulty in flexing thigh and hamstring muscles
- Recreation of pain by pushing against resistance with a straightened knee or bending the knee
Testing for Osgood-Schlatter Disease
Osgood Schlatter disease is typically diagnosed based on physical symptoms and medical history, so usually, tests like x-rays aren’t needed. But sometimes, your doctor might still recommend an x-ray to rule out other possible conditions that could be causing your symptoms. These could include things like a broken bone, an infection, or a bone tumor. In some cases, x-rays might also be taken to look for a type of injury known as an avulsion injury, which can occur after a traumatic event, in a certain section of the knee.
Osgood-Schlatter disease can show up on x-rays as a raised area on the shinbone under your knee (the tibial tubercle), along with swelling, separated pieces of bone, or hardened areas in the tendon located at the bottom of your kneecap. But, it’s important to note that these things can also appear on an x-ray even if you don’t have Osgood-Schlatter disease. That’s why it’s important for doctors to also take into account your symptoms and medical history when making a diagnosis.
If you do have an x-ray for Osgood-Schlatter disease, your doctor might recommend taking images of both knees. This allows them to see what’s normal for your body, and better spot any abnormalities that could suggest the disease.
Treatment Options for Osgood-Schlatter Disease
Osgood-Schlatter disease is a knee condition that can last for up to two years until the growth area (apophysis) in the knee fully develops and fuses. During this time, the condition will slowly get better on its own. Until then, doctors often recommend limiting or adjusting physical activities that cause pain. Even though taking a rest might not speed up recovery, it can significantly help reduce pain.
If you have this disease, you can still participate in sports and other physical activities. The main thing to consider is that any activity should not cause pain or discomfort. If you feel pain during the activity, it’s important to rest until the pain resolves.
To help manage the discomfort, you can apply ice and use non-steroidal anti-inflammatory drugs (NSAIDs) locally, which means directly to the knee area. These methods help in reducing pain. A protective knee pad can also be helpful, as it can shield the knee, specifically the bony bump below the kneecap (tibial tubercle), from getting hit or impacted directly.
Including hamstring and quadriceps stretching and strengthening exercises in your routine can also benefit you a lot. If the pain doesn’t decrease with these methods, you might need to attend physical therapy. In some severe cases, you may need to immobilize, or stop moving, your knee for a short while under professional guidance. However, methods such as injection therapy or surgery are generally not recommended to treat Osgood-Schlatter disease as they have not been proven to be effective.
Commonly, the symptoms of this condition eventually disappear as the knee fully grows. However, it might leave a thickened or prominent bump on the knee. This is normally not something to be concerned about, as it doesn’t cause problems in most cases.
In about 10% of cases, symptoms may continue for more than 1-2 years, even after the person has fully grown. For these rare cases, if the symptoms still persist, doctors may consider surgical intervention such as removing the bony bump on the knee. However, this is typically a last resort as it doesn’t offer additional benefits compared to medical treatment and could lead to complications.
What else can Osgood-Schlatter Disease be?
When experiencing a strange pain, there might be numerous medical conditions at play. Some possibilities can include:
- Patella tendonitis (inflammation of the tendon connecting the kneecap to the shinbone)
- Osteomyelitis of the tibia (an infection in the shinbone)
- Perthes disease (a childhood condition that affects the hip)
- Synovial plica injury (damage to the thin structures within the knee)
- Infectious apophysitis (an inflammation of a bony prominence due to a bacterial infection)
What to expect with Osgood-Schlatter Disease
The outlook for Osgood-Schlatter disease is generally very good. This condition naturally gets better over time, but it can take several months to fully resolve. However, for about 10% of patients, symptoms may persist into adulthood. This typically happens when the person either doesn’t seek treatment, or doesn’t follow the recommended treatment guidelines properly.
There are some reports of the pain associated with this disease lasting for several years. This is why it’s so important to get treatment when symptoms first appear and to stick with the treatment plan your doctor provides.
Possible Complications When Diagnosed with Osgood-Schlatter Disease
The medical term “prominence of the tibial tubercle” can be confusing. To put it in simple terms, this refers to a noticeable projection or bump on the shinbone.
Main Issue:
- Noticeable bump on the shinbone
Another concern is the ongoing pain, which means the pain is continuous and doesn’t go away.
Common Complaint:
- Continuous or lingering pain












