What is Osteochondritis Dissecans (osteochondral lesion)?
Osteochondritis dissecans (OCD), also known as an osteochondral lesion, is a condition first discovered in 1888 by a German surgeon named Franz König. This condition is not fully understood yet, but it’s believed to be caused by multiple factors. Oddly enough, the cause of OCD is unknown and it can occur at any age, but it’s most commonly found in teenagers.
The severity of osteochondral lesions varies greatly. Some people might not have any symptoms at all, while others may experience mild pain. In more severe cases, these lesions can cause joint instability and make the joint “lock” or get stuck. Over time, the cartilage, which is upper layer of bone in the joint, can break down and form a loose body inside the joint. The condition can also lead to early onset of osteoarthritis, which is a form of joint inflammation that causes pain and stiffness.
For this reason, it’s critical to diagnose and treat OCD as soon as possible. Early recognition and appropriate treatment are important to help prevent more serious issues and promote a better long-term outcome.
What Causes Osteochondritis Dissecans (osteochondral lesion)?
While the exact cause of osteochondritis dissecans, a condition where small pieces of bone and cartilage within a joint crack and lose blood supply, is not fully understood, it’s thought to be caused by several factors. These include, genetics, inflammation, sudden loss of blood supply to a bone (also known as avascular necrosis), and repeated minor injuries. Although originally it was thought that the condition was caused by bone inflammation (which is suggested by the name “osteochondritis”), many studies have not been able to confirm this.
Another explanation suggests that the condition occurs during adolescence when the cartilage, the soft tissue that covers the ends of the bones, is growing. At this stage, the blood supply to the bone just beneath the cartilage changes, leaving it more prone to losing its blood supply. Interestingly, osteochondritis dissecans is more common in young athletes, suggesting that the repeated stress and strain put on their joints might be a cause.
All these theories have been researched with varying degrees of success. However, the most widely accepted theory is that repetitive minor injuries, whether caused by major incidents or not, result in the first symptoms of the condition.
Risk Factors and Frequency for Osteochondritis Dissecans (osteochondral lesion)
Osteochondritis dissecans is a condition that tends to occur in about 15 to 29 out of every 100,000 patients. Although it can affect individuals from children to adults, it’s most commonly seen in people between the ages of 10 and 20. Males get this condition about twice as often as females, and it’s more common in young athletes. The parts of the body that are usually most affected by this are the knee (specifically a part of the knee called the medial femoral condyle), elbow (capitellum), and ankle (talus), with the knee being the most common.
- Osteochondritis dissecans affects approximately 15 to 29 per 100,000 patients.
- Most patients are between 10 to 20 years old, but it can occur in people of any age.
- Males get this twice as often as females.
- Young athletes are more likely to get this condition.
- The most affected areas are the knee (particularly the medial femoral condyle), followed by the elbow (capitellum), and the ankle (talus) to a lesser extent.
Signs and Symptoms of Osteochondritis Dissecans (osteochondral lesion)
Osteochondral lesions can be discovered in various ways. Some patients may not have any symptoms, and the issue is only found when they have an imaging test for another reason. Alternatively, they might recall a past experience of mild chronic pain that went away on its own without needing treatment. Other patients might come to the doctor when they experience mild chronic pain in the affected joint, which might occur with or without an injury. Usually, these sorts of patients only seek help several months to a year after the pain begins. The symptoms can be more severe for those who have a loose fragment, causing significant joint pain, a locking sensation, swelling, and the joint may feel unstable.
During a physical assessment, these patients may show signs of pain when the affected joint is pressed, they could have a reduced or painful range of movement in that joint, and there might be swelling or fluid build-up in the affected area. It’s also important to make sure that other injuries, such as fractures or ligament damage, are ruled out.
Testing for Osteochondritis Dissecans (osteochondral lesion)
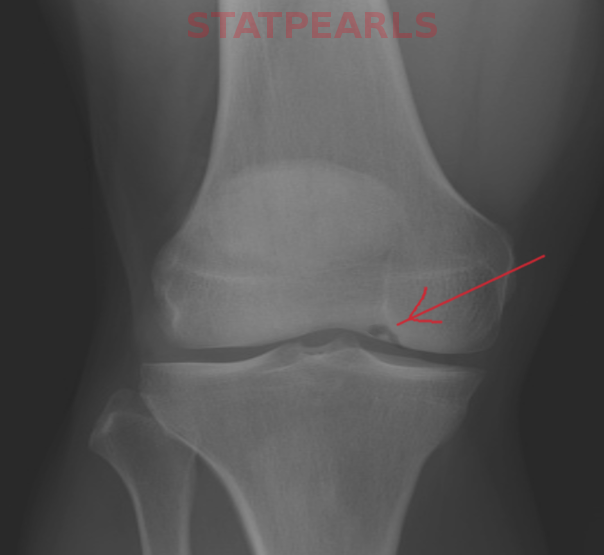
Imaging, or creating internal pictures of the body, is a critical part of diagnosing and treating patients with bone and joint problems. The first step is usually to take an x-ray of the affected joint. X-rays may reveal a hollow, or “lucent”, area in the bone near the joint, and can sometimes show a broken bit of bone within the joint. However, x-rays aren’t always detailed enough to tell us if this broken bone fragment is stable, meaning it’s properly embedded and not likely to move, or how large the fragment and the surrounding damaged area are.
This is where magnetic resonance imaging (MRI) comes in handy. Doctors use MRIs when the x-ray throws up an abnormality that needs further examination. MRI scans can tell if the bone fragment is likely to be stable, they can distinguish between normal bone development and bone-related diseases, and they are crucial for planning treatment. In fact, when doctors are unsure whether the bone fragment is stable, usually an MRI is recommended. This is because, compared to other imaging techniques, MRI is very sensitive (likely to correctly identify a problem when it’s present) and specific (likely to give a clear cut answer).
During the MRI, doctors look for certain features that can indicate whether the bone fragment is unstable. For example, a clear round focus of intense signal deep in the problematic area, or a clear line of intense signal beside the fragment. Doctors also look for a defect in the cartilage on top of the problem area, and an intense signal passing through the joint cartilage and the nearby bone. All these features can suggest that the bone fragment is unstable. Some tricky cases may require MRI with a dye (MRI arthrography), or a CT scan with a dye (CT arthrography), especially when the MRI scan is not an option.
Once treatment has started, whether that’s through surgery or more conservative measures, MRI scans can monitor the progress of healing. Doctors may check the MRI reports for decreased signals around the problematic area, capturing that the inflammation is going down, a shrinkage in the problematic area, or fresh bone growth in the bed of the problematic spot. Particularly after surgery, MRI allows doctors to see how well the surface of the joint and the bone-cartilage interface are recovering, without having to perform invasive procedures.
Treatment Options for Osteochondritis Dissecans (osteochondral lesion)
Your treatment will depend on your age, when you come in for treatment, how severe your symptoms are, and the stability of your lesion. Lesion refers to an area of tissue that has been damaged through disease or injury. There are systems in place to understand the exact state of the lesions, and the crucial factor is the degree of involvement and movement of the fragment of cartilage overlying the lesion.
If the lesions are stable, we usually try to manage it without intrusive procedures, using methods like immobilization (keeping the area from moving around much) and limiting how much weight you put on it. The duration of this will depend on which joint is affected. If you tried these less invasive treatments but they didn’t work, you might need drilling techniques – drilling into the bone to stimulate healing. These procedures generally have high success rates, healing and improving symptoms in 92% to 100% of patients, the ones that involve drilling through the joint having slightly better success rates.
But if the lesions are either unstable or have been moved from their original position, surgery becomes necessary. This is most common with knees, which are the site of 58% of all surgeries for these kinds of lesions. The strategies vary – depending on the individual case, doctors might decide to secure the affected area in place, remove the damaged tissues, create small fractures to stimulate healing, or graft in new cartilage.
The doctors might fix your lesions in place using different types of screws, absorbable implants, or bone plugs. Traditional metal screws have high success rates of 84% to 100% when the lesion size allows for their use. The downside of these screws is that you will often need a separate procedure a few weeks later to remove the screw. Absorbable implants don’t need to be removed but tend to lead to complications more often than with metal screws. Bone grafts can achieve “good to excellent” results in 72% of patients when receiving a graft from a donor. The primary goal of all these surgeries is to promote the reformation of cartilage and/or repair the surfaces of your joints to prevent an early onset of osteoarthritis, which is a type of degenerative disease causing pain and stiffness in the joints.
What else can Osteochondritis Dissecans (osteochondral lesion) be?
These medical conditions include:
- Osteoarthritis
- Meniscus injury
What to expect with Osteochondritis Dissecans (osteochondral lesion)
Osteochondral lesions, or damage to the cartilage and underlying bone in a joint, can be either stable or unstable. Stable lesions generally have a better recovery prognosis than unstable ones. In the case of stable lesions, if they are managed through non-surgical treatments, they usually heal on their own. Currently, there isn’t a universal grading scale for lesions that require surgery.
On the other hand, unstable lesions, those that need surgical treatment or ones that didn’t improve with non-surgical treatments and require surgery, have varying success rates. The success rate can range from 30% to 100%, depending on the surgical method used. It’s important to know that even with surgery, most patients still develop early-stage osteoarthritis, a condition that causes joint pain and stiffness.
It’s also worth noting that patients who receive treatment during their teen years typically have better outcomes than those who present as adults.
Possible Complications When Diagnosed with Osteochondritis Dissecans (osteochondral lesion)
Common Consequences:
- No healing of the bone
- Long-term pain
- Joint inflammation and stiffness