What is Pelvic Ring Injuries?
The pelvic ring is made up of the sacrum (a triangular bone at the bottom of your spine) and two innominate bones (made up of three parts: the ilium, ischium, and pubis). This ring-like structure is not very stable on its own, which is why it relies on strong ligaments – tough connective tissues, to maintain its shape and stability. If the pelvic ring is moved out of place, at least two areas must be disrupted.
Injuries to the pelvic ring can vary greatly. They may include simple fractures of the sacrum or pubis that can often be treated with rest and limited medical intervention, to more serious injuries that are caused by large forces, damaging the bones or the ligaments of the pelvic ring. The latter types of injuries require immediate medical assistance as they can be life-threatening.
Let’s understand the role of the various ligaments that make up the pelvic ring:
– The anterior symphyseal ligaments at the front of the body help resist rotation.
– The pelvic floor has sacrospinous ligaments (prevents rotation) and sacrotuberous ligaments (resists shear, a force that causes layers or parts to slide upon each other, and bending).
– The back of the pelvic ring has the most potent ligaments in our body that create greater stability compared to those at the front. This complex includes
– Anterior sacroiliac ligaments that resist rotation once the pelvic floor and front structures have failed.
– Interosseous sacroiliac ligament that helps to prevent the pelvis from sliding front to back.
– Posterior sacroiliac ligament that restricts movement of the pelvis upwards and downwards.
– The iliolumbar ligament supports the back of the pelvic ring by resisting rotation.
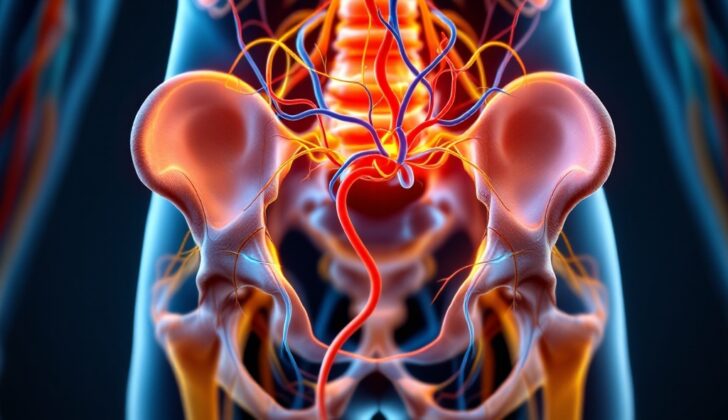
This bony and ligamentous structure of the pelvic ring helps in protecting our organs as well as various nerve and blood vessels:
Nerve routes:
– The lumbosacral trunk (a bunch of nerves) runs in front of the sacral ala (a portion of the sacrum) and sacroiliac joint (where the spine and pelvic bone meet).
– The L5 nerve root runs in front of the top part of the sacral ala.
– The S1 nerve root leaves from the anterior sacral foramina, a hole between the first and second sacral bone.
Blood circulation:
– The external iliac artery, a large blood vessel, passes in front of the pelvis and branches out into the common femoral artery, after passing the inguinal ligament (a band running from the pubic bone to the hip bone).
– The internal iliac artery, another large blood vessel, curves at the back, near to the sacroiliac joint, and branches out into anterior and posterior divisions, becoming obturator and superior gluteal arteries.
– A network of connections called the corona mortis connects the obturator artery and the external iliac artery or the deep inferior epigastric artery, lies at an average of 6.2 cm from the pubic symphysis (where the left and right hip bones meet in front).
– The venous plexus, a large network of veins in the back of the pelvic area, tends to be a significant source of bleeding with pelvic ring injuries.
What Causes Pelvic Ring Injuries?
Pelvic ring injuries often happen in young people due to incidents involving a lot of force, such as falls from high places or car crashes. These high-impact accidents can also cause injuries to other parts of the body. In contrast, in older people, pelvic ring injuries are typically caused by falls that don’t involve a lot of force.
Anterior-posterior compression injuries, which happen when the front and back of the pelvis are squeezed together, are common injuries seen in horse riding and motorcycle accidents. On the other hand, lateral compression injuries, which happen when the side of the pelvis is impacted, often happen when a vehicle hits the pelvis. Vertical pelvis injuries, or injuries resulting from an impact coming from the top or bottom, typically happen from falls or injuries involving a force coming from above or below.
It’s important to note that these injuries can be serious. While the death rate for closed fractures, or fractures that don’t break the skin, varies between 1% and 15%, it can rise to 50% for open fractures, or fractures that break the skin. The main cause of death in these cases is typically heavy bleeding. In the case of lateral compression injuries, or injuries where the side of the pelvis is impacted, the most common cause of death is a closed head injury, or head injuries where the skull is not fractured.
Risk Factors and Frequency for Pelvic Ring Injuries
Pelvic ring injuries occur in people of all ages and make up about 3% of all bone fractures. They most commonly affect those aged 18 to 44, and men tend to experience these injuries more often than women. The rate of these injuries is approximately 0.82 per 100,000 individuals, and they are typically associated with a high injury severity score.
- Pelvic ring injuries happen to people of all ages and make up about 3% of all bone breaks.
- People aged between 18 and 44 are the most commonly affected by these injuries.
- Men are more likely to experience these kinds of injuries than women.
- These injuries occur at a rate of around 0.82 per 100,000 people.
- They are usually associated with a high injury severity score, ranking between 25 and 48.
Signs and Symptoms of Pelvic Ring Injuries
Pelvic ring injuries are high-energy impacts that can cause various other health issues. These issues may require immediate attention and include:
- Chest trauma: up to 63% of cases
- Long bone fractures: detected in about 50% of cases
- Head injuries and damage to organs within the body cavity: around 40% cases
- Spinal fractures: seen in around 25% of patients
- Intestinal injuries: occur in 14% of cases
- Injuries to the genital and urinary system: between 6% to 15% of cases
- Open fractures: approximately 5% of cases. Open pelvis fractures have about a 50% mortality rate; immediate antibiotics are essential. Doctors should also check the rectal and vaginal areas for any breaks in the skin.
Having a pelvic ring injury could pose a serious risk to life or be connected to other life-threatening injuries. As such, a detailed check-up is typically recommended that may include:
- Advanced trauma life support
- Checking nerve-based activity and sensitivity to sensation
- A physical examination of the pelvic region, including certain pressure tests
- A check for uneven leg length not caused by limb fractures
- Looking at the prostate for signs of injury or at the urethral opening for traces of blood, which may hint at injury in the urinary system
- A thorough check of the rectum and/or vagina
- Checking the genital region which can reveal any swelling or movement abnormalities
Further, some specific signs can indicate significant issues:
- The Destot sign: Refers to the detection of a blood-filled swelling in the area between the legs and the lower trunk. This may hint at a pelvic fracture with active bleeding.
- The Grey Turner sign: Characterized by bruising in the side area of the body, indicating internal bleeding.
- Morel-Lavallée lesion: This condition results from a shearing force acting on the skin during the trauma. Clinically, it may appear as significant abrasions, deep-seated bruising, or under the skin bleeding. It might influence the surgery plan and may require further action. It may also be spotted on a computerised imaging of the body.
Testing for Pelvic Ring Injuries
Evaluating injuries to the pelvic ring involves several different imaging methods that help doctors understand the extent of the injury and decide on the most appropriate treatment. These methods include x-rays, CT scans, and sometimes an MRI scan, each playing a specific role in highlighting injuries and associated complications.
Imaging:
* X-rays: Basic x-rays of the chest and the front of the pelvis are the first step in evaluation, followed by more specific views such as inlet and outlet, which are important in evaluating movement and change in shape in the front-to-back (coronal) plane. There is also a special type of x-ray known as the flamingo view which helps in determining if the pelvic ring is unstable over a long period.
* CT scan: A CT scan is a basic requirement for all injuries to the pelvic ring. CT scans provide clear pictures of bone structures and give a good idea of the extent of any sacral (lower spine) injury.
* MRI: MRI scans are not often used in acute (immediate) trauma to the pelvic ring. However, in certain situations, they can give more detailed information about injuries to soft tissues.
The classification of injuries to the pelvic ring is as follows:
Type A: Stable
* A1: Fractures that do not involve the pelvic ring
* A2: Stable fractures of the pelvic ring that have moved little or not at all
Type B: Not stable when rotated, but stable vertically
* B1: Open book
* B2: Lateral compression on the same side
* B3: Lateral compression on the opposite side
Type C: Not stable when rotated and not stable vertically
* C1: On one side only
* C2: On both sides
* C3: Accompanied by a fracture of the acetabulum (hip socket)
The Young and Burgess classification system has four main categories of pelvic ring injuries :
* Lateral compression (LC)
* Anterior-posterior compression (APC)
* Vertical shear (VS): The half-pelvis is moved in a vertical direction indicating total instability.
* Combined Mechanism (CM): Any combination of the above
Sacral fractures (fractures of the lower spine) are classified into three zones according to the classification system developed by Denis:
* Zone 1: To the side of the sacral foramen (holes through which nerves and blood vessels pass)
* Zone 2: Involving the sacral foramen
* Zone 3: To the inner side of the sacral foramen – these fractures have the highest chance of causing nerve injury, including injury to the nerve roots or the lower end of the spinal cord (cauda equina).
The term “lumbopelvic dissociation” describes a type of fracture that disrupts the connection between the lower spine and the pelvis, often requiring surgical repair. It is important to note that this is often found in people having fractures on both sides of the sacrum (lower spine), emphasizing why it’s critical to carefully review CT scans for fractures in the coronal (front-to-back) plane of the sacrum.
Treatment Options for Pelvic Ring Injuries
Recognizing an injury to the pelvic ring, the structure formed by the hip bones, is critical as it may be a life-threatening emergency. It requires teamwork between healthcare professionals to effectively manage the patient, particularly those who are severely injured.
In a rush to stabilize the patient, medical providers must remember that a person with a pelvic ring injury could have additional sources of bleeding, hence a thorough assessment of the entire body is required.
Pelvic ring injuries can cause serious blood loss from various parts of the body. Commonly, it is from the pelvic veins which, if ruptured, can cause a hematoma (a collection of blood outside of blood vessels) that can hold up to 4 liters of blood. Apart from this, blood can also leak from the bone or from blood vessels like arteries. Although arterial injury is less common, this sort of bleeding can involve major blood vessels supplying the pelvic region.
When dealing with severe cases that require extensive blood transfusions, healthcare providers follow a protocol to ensure the best survival rates. In the meantime, a temporary measure could be the placement of a special device called a pelvic binder or a sheet around the patient’s pelvis. This technique can help reduce the displacement of the pelvic ring injury and limit blood loss. However, this measure has its pros and cons, and its use depends on the stability of the patient and the type of pelvic injury.
In case the patient remains unstable even after blood transfusion, and after placement of the stabilizing device, additional steps might be necessary. The next steps could include the use of angiography and embolization, procedures geared towards identifying and stopping the source of bleeding. These methods are, however, subject to debate.
Pinpointing the run-off areas for bleeding can be done with CT angiography which can reliably provide up to 98% to 100% accuracy. If the bleeding continues even after targeted attempts to stop it, temporary blocking off of the two internal iliac arteries might be necessary. This procedure, while effective, can also lead to complications such as tissue death and impotence.
In severe cases, an external fixation may be used either as a temporary or permanent measure. This involves the placement of fixation devices (usually pins) on the external surface of the bone to hold the fracture together. The decision to place external fixators depends on several factors, such as the stability of injuries and external injury components. Pin positions for these fixators vary, and each placement has its advantages and drawbacks.
Anterior subcutaneous pelvic fixator, a new method, is designed to avoid complications related to external fixation. It promises advantages such as lesser operative time and blood loss. In certain instances of open pelvic ring injury with perineal trauma, a surgical procedure called diverting colostomy might be necessary.
Definitive measures are applied depending on the stability of fractures. Unstable fractures usually require surgical intervention whereas stable fractures can undergo non-operative management. Different techniques of open and closed fixation can be used depending on the pattern of the fracture. One of these methods known as triangular osteosynthesis might be used for addressing posterior instability.
The best timing for definitive fixation remains a topic of debate. There are both pros and cons to having early surgery. The benefits include pain relief, supportive care, improved reduction quality, bleeding control, and early mobility. Conversely, it might increase the risk of bleeding and possibly worsen the patient’s condition if the patient isn’t fully stabilized.
What to expect with Pelvic Ring Injuries
Injuries to the pelvic ring, especially in cases where there’s unsteady blood flow, are still associated with high death rates. This is due to factors like rapid blood loss, difficulty in stopping the bleeding, and the severity of related injuries. In spite of these challenges, recent advancements have led to a decrease in death rates associated with pelvic ring injuries, from 9.1% down to 4.9%. This improvement becomes even more impressive when taking into account the patient’s age and the severity of brain, chest, and abdomen injuries.
A classification system by Young and Burgess helps predict the death rate in pelvic ring injuries. In this system, injuries are categorized as either stable or unstable. Stable injuries have a death rate of 7.9%, while unstable injuries have a higher death rate of 11.5%. Long-term outcomes also tend to be better if the back part of the pelvic ring can be realigned within 1 cm.
When it comes to returning to work after a pelvic ring injury, outcomes vary. Many patients experience some form of lasting impairment. According to research, 24% of patients lose their jobs, 34% return to work but with changes to their duties, and 46% are unable to perform their tasks as they did before the injury.
In terms of the likelihood of death in pelvic ring injuries, males and older individuals tend to have higher rates. However, it should be noted that women who have had a procedure to stabilise the front of their pelvic ring are still able to safely give birth vaginally, as long as both the front and back of the pelvis are not immobilised.
Possible Complications When Diagnosed with Pelvic Ring Injuries
Pelvic ring injuries can cause several complications including malunion, hardware failure, neurological dysfunction, sexual dysfunction, chronic pain and disability, infections, and deep vein thrombosis or pulmonary embolisms. In some cases, these injuries can also lead to additional problems if they involve other areas, like the hip joint or the acetabulum.
Malunion is a common issue after pelvic ring injuries:
- There’s ongoing debate over how to define or measure this displacement.
- Patients who recover correctly tend to have better outcomes. Displacements little less than 1cm are often considered bearable.
- It might be hard to tell apart stable and unstable patterns.
- For specific cases, or to guide surgery, doctors may consider testing stability under anesthesia.
- Non-operative treatment of complete sacral fractures with fractures on the same side may lead to displacement over time in about 39% of cases; this increases to 68% for those with fractures on both sides.
Hardware failure is also common, but doesn’t necessarily mean the hardware needs to be removed:
- Micro movement always occurs in a well-aligned and healed pelvic ring, leading to high rates of hardware failure over time. But, if the pelvic ring has fully healed, any breakage of the hardware won’t cause any displacement.
- Hardware positioned across the symphysis might fail in around 43% of cases after one year, but 97% of these cases don’t have symptoms.
Other complications include:
- Neurological Dysfunction: Around half the people with a ‘Denis 3’ fracture to the sacrum end up with nervous system dysfunction.
- Sexual Dysfunction: Erectile dysfunction may occur in around 46% of men, and painful intercourse in about 56% of women after a pelvic ring injury. The latter increases to 91% with ‘APC’ injuries and to 79% of patients treated with symphysial plating.
- Pain and disability is discussed more in the prognosis section.
- Infections: Infections may occur in up to 16% of cases when using a posterior approach to the sacrum, especially in obese patients who are also at greater risk for complications and needing reoperation.
- Deep Vein Thrombosis/Pulmonary Embolism: In some pelvic-ring injury cases, there may be a need for an inferior vena cava (IVC) filter to prevent blood clots from reaching the lungs or forming in deep veins.
- Combined Injuries: In some cases, people have injuries to both the pelvic ring and the acetabulum, which are often linked with higher rates of complications. Hip dislocation, specifically, has been linked to an increased rate of complications.
Recovery from Pelvic Ring Injuries
Depending on the type of injury and the treatment used, a patient may need to limit the amount of weight they put on one or both limbs for a time. This is where the help of nursing staff and therapists comes in – they are vital in aiding the patient’s return to their normal function. It’s also essential to take preventive measures against deep vein thrombosis (DVT, a blood clot in the leg) after the surgery.
Preventing Pelvic Ring Injuries
Doctors are often encouraged to talk with their patients about what they can expect in the early stages of their interactions. This can include explaining what kind of results are likely and that there may be some ongoing discomfort. It’s also important to discuss sensitive topics such as problems with sexual function or pain during sex, as these factors can greatly affect a person’s overall health and happiness. If needed, the doctor may recommend seeing a specialist in women’s health (OB-GYN) or urinary and sexual health (urologist).