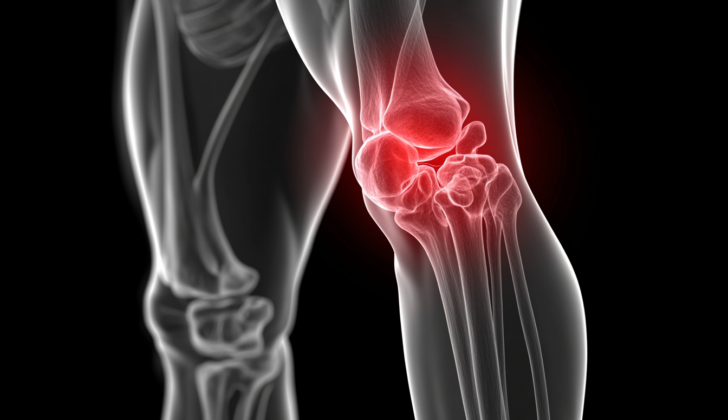
What is Quadriceps Tendon Rupture?
The quadriceps tendon is made from the meeting point of four muscles on the front upper knee – the rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius. This tendon, together with the patellar tendon and the kneecap (patella), form the system that helps us extend or straighten our lower leg.
This tendon is very resilient and can handle heavy loads without tearing. It gets its blood supply and nerve signals from the femoral nerve and artery. In particular, three of these four muscles get their blood from the lateral femoral circumflex artery while the vastus medialis muscle gets its supply from the femoral artery and other arteries around the knee.
The vastus lateralis, vastus medialis, and vastus intermedius help not only in straightening the knee but also keeping the kneecap in the correct position. The vastus lateralis, which is the largest among these four muscles, pulls the kneecap to the side. The smallest, the vastus medialis, balances this action by pulling the kneecap inwards, while the vastus intermedius helps keep the kneecap in the middle. The overall effect of these muscles working together allows us to extend our lower leg. The rectus femoris also helps in bending the hip.
Tearing of this crucial tendon severely affects the knee’s ability to straighten and can directly impact our day-to-day functionality. The extent to which a tear in the quadriceps tendon affects us depends on how severe the tear is. Small tears might not have a significant impact, but a complete tear could totally prevent the lower leg from extending or straightening.
What Causes Quadriceps Tendon Rupture?
Quadriceps tendon injuries seem to happen more often in men and become more common as people age, especially after 40. Males are eight times more likely to suffer from this type of injury than females. However, it’s worth noting that patellar tendon injuries, which are different, are more commonly found in younger people, usually because of sports-related activities.
Interesting to note is that men between the ages of 50 and 65 who have had a total knee replacement surgery, are particularly prone to suffer from a quadriceps tendon injury.
Having certain health conditions can also increase the chance of a quadriceps tendon injury. Conditions like diabetes, a disorder that results in too much sugar in the blood; hyperparathyroidism, overactivity of the parathyroid glands; gout, a form of arthritis caused by excess uric acid; chronic kidney disease, long-term damage to the kidneys; obesity, being excessively overweight; and hypercholesterolemia, excessively high levels of cholesterol in the blood. Also, people with certain conditions that affect the body’s connective tissues, like rheumatoid arthritis, systemic lupus erythematosus, and osteogenesis imperfecta, are at a higher risk as well.
Some medications might boost the risk of getting a quadriceps tendon injury as well. These medications include anabolic steroids, corticosteroids, and fluoroquinolones, a type of antibiotic. If you have a treatment involving injections directly into a joint, there’s a 20 to 33% chance it could lead to a quadriceps tendon injury.
Risk Factors and Frequency for Quadriceps Tendon Rupture
Ruptures in the extensor mechanism, a system involved in extending the lower leg, are highly uncommon. Despite their rarity, these injuries can be quite severe and often lead to long-term disability. Out of these rare injuries, tears in the quadriceps tendon occur more often than those in the patellar tendon. In comparison, the likelihood of a quadriceps tendon rupture is 1.37 per 100,000 people, while for a patellar tendon rupture, it’s 0.68 per 100,000 people. Mostly, these tears occur on one side, but there’ve been few instances where the injury occurred on both sides due to a single incident.
Signs and Symptoms of Quadriceps Tendon Rupture
If someone has a quadriceps tendon rupture, they typically experience three key symptoms – sudden pain, inability to lift the leg straightly, and a noticeable bump above the kneecap. Often people hear a ‘pop’ or feel a tearing, followed by difficulty bearing weight on the affected leg, and swelling. It can feel different from tendinopathy, which usually begins with pain. A gap can usually be felt at the top of the kneecap in complete tear cases, and this leads to difficulty in raising the leg straight. Depending on the severity, knee extension can be affected; it usually tends to disappear completely in serious cases. Hip or ankle mobility is typically not affected by this condition.
- Sudden and severe pain
- Inability to lift the leg straight
- A noticeable bump above the kneecap
- Popping sound or tearing sensation
- Difficulty bearing weight on the affected leg
- Swelling around the knee
- A gap felt at the top of the kneecap (in severe cases)
- Impaired knee extension (varies with severity of the tear)
- Usually no hip or ankle movement impairment
Testing for Quadriceps Tendon Rupture
A doctor can often diagnose a rupture in the quadriceps tendon, the tendon that connects the thigh muscles to the knee, through a simple health history assessment and physical examination. Additional imaging tests are usually not needed.
However, when imaging is necessary, ultrasound is often the first choice. Ultrasound can detect any breaks in the tendon, measure the gap caused by the rupture when the knee is bent, and check how well the tendon is healing over time. It can also spot any related issues, such as pooled blood (hematomas), fluid buildup (effusions), or hardened lumps (calcifications).
X-rays do not typically help in diagnosing quadriceps tendon ruptures. However, they can be used to rule out other injuries or conditions. For example, the position of the kneecap (patella) on an x-ray can suggest different types of tendon ruptures: a high-riding kneecap may hint towards a patellar tendon rupture, while a low-riding kneecap could indicate a quadriceps tendon rupture. X-rays can also spot any related kneecap injuries or fractures.
Magnetic resonance imaging (MRI), though less commonly used because ruptures in the quadriceps tendon aren’t very common, can accurately reveal tears in the quadriceps tendon. Ultrasound and MRI are both effective in detecting knee tendon injuries. However, ultrasound is slightly more accurate when it comes to spotting patellar tendon ruptures, while MRI may be slightly more accurate for quadriceps tendon ruptures. Nevertheless, this difference is unlikely to significantly impact treatment decisions.
Treatment Options for Quadriceps Tendon Rupture
If you suspect you’ve ruptured your quadriceps tendon, a type of injury common in muscles and bones, the initial treatment includes rest, ice, compression, and elevation. Minor tears in the quadriceps tendon that do not disrupt the mechanism of straightening the knee might be treated without surgery using a knee brace and physical therapy. However, for most complete ruptures, early detection and surgical treatment is vital to reduce long-term issues and disability. The timing of surgery is believed to impact the recovery and functionality more than the specific approach of the surgery used.
Acute, or sudden, ruptures can usually be repaired with surgery. Different repair techniques have been explored. Some involve suturing the two ends of the ruptured tendon together, particularly if the tear is in the middle of the tendon. Drilling holes in the patella, or kneecap, has been a common approach if the rupture is near or at the place where the tendon attaches to the bone. Suture anchors, which are devices affixed to the bone to secure the tendon, can be a good alternative to drilling holes because they make a smaller incision and reduce the surgery time. Both techniques have been reported to have similar outcomes in terms of clinical and mechanical results.
The optimal surgical technique is not well-established due to limited data. Typically, surgical repair is based on individual cases and the surgeon’s experience. However, there is a trend towards using patellar drill holes if the tear is located near the poles of the patella. Suture anchors are becoming more popular because they need smaller skin cuts and result in shorter surgical times. The effectiveness of this trend is yet to be determined. For intratendinous ruptures, where the rupture happens within the tendon, an end-to-end suture technique is typically used. The timing of the surgery is important because delay may result in the tendon retracting and the tissue quality reducing, making the surgery more challenging and impairing the recovery. Surgery is usually recommended within 48 to 72 hours after complete tendon ruptures.
The surgery usually involves a midline incision at the knee. The standard repair technique drills tunnels in the kneecap and uses sturdy, nonabsorbable sutures in the tendon. After the surgery, the knee should ideally be able to flex to 90 degrees. The knee is initially immobilized for a short period, after which the range of motion and strengthening exercises are gradually increased.
If the rupture is chronic, meaning it’s over two weeks old, the tendon may have retracted up to 5 cm. Surgical techniques similar to acute ruptures can be used, but the tendon might have to be lengthened, for example, using the Codivilla procedure (V-Y lengthening). Tissue grafts or synthetic tape may be needed to attach the tendon to the patella.
Additional reinforcement techniques might be suggested if the tissue quality is poor or surgery is delayed. These techniques can include wire reinforcement, Merisilen tape, and fascia lata reinforcement.
Postoperative management is not clear-cut due to the lack of studies evaluating the optimal approach. In the past, the knee was usually immobilized at full extension for six weeks postoperatively to allow the tendon to fully heal. Nowadays, there’s a trend towards early knee motion to reduce joint stiffness and muscle wasting. However, early movement has been found to possibly result in more adverse outcomes and the need for additional surgeries compared to keeping the knee straight for 6 weeks. Because this type of injury doesn’t happen often, there are no definitive, statistically supported best practices for surgical interventions or aftercare yet.
What else can Quadriceps Tendon Rupture be?
Doctors consider a range of other health conditions when diagnosing a patient’s knee pain. These can include:
- Torn patellar tendon (the tendon around the kneecap)
- Stress fracture in the kneecap
- Stress fracture in the thigh bone
- Bone or soft tissue tumors
- Compartment syndrome (a painful condition that occurs when pressure within the muscles builds to dangerous levels)
- Back pain that radiates to the knee
- Meralgia paresthetica (a condition characterized by tingling, numbness and burning pain in the outer part of your thigh)
- Injury or entrapment of the femoral nerve (the nerve in the thigh that supplies the skin and muscles of the thigh and leg)
What to expect with Quadriceps Tendon Rupture
Over half of people who suffer from a quadriceps tendon injury may experience weakness and soreness in their thigh at the site of injury. A patient’s chances of recovery increases if surgery is performed right after the injury. After full recovery, most patients are typically able to go back to their usual jobs or activities.
In the case of athletes, a thorough evaluation of the injured leg by the surgeon is crucial before returning to sports activities. The aim is for the injured leg to regain at least 85 to 90% of the strength compared to the uninjured leg. Also, the doctor will need to determine whether the patient’s balance is satisfactory and assess if there’s any remaining swelling.
Possible Complications When Diagnosed with Quadriceps Tendon Rupture
Regardless of the type of surgery or follow-up treatment, the most common issues patients might experience are pain and weakness in the quadriceps (thigh muscles). These difficulties usually appear when the patient is standing for a long time, squatting, or going up and down stairs. However, if the patients receive prompt medical help, they usually don’t report severe difficulties in carrying out daily tasks.
The possible difficulties include:
- Weakness: Around one-third to half of the patients might find their strength reduced.
- Stiffness
- Functional Impairment: Around half of the patients might not return to their normal level of activity or sports.
- Painful sensations in and around the kneecap, or particularly sensitive scars.
Recovery from Quadriceps Tendon Rupture
Being immobilized: Doctors usually recommend that patients should limit their movement for a certain time after surgery. The recommended length of time varies, but it is usually between 3 to 10 weeks. However, many medical studies recommend six weeks of limited movement to protect the repaired area, whether the repair was done immediately after the injury or later on.
Weight-bearing status: Even while being limited in movement, patients are often allowed to bear some weight on the repaired area. Alternatively, they can start gently moving the repaired area at angles from 0 to 55 or 0 to 60 degrees, while bearing partial or full weight.
Measuring the outcome: To measure how successful the operation was, doctors use several scoring systems. Some systems are specially designed by individual surgeons, such as those introduced by Siwek and Rao and Rougraff et al. Other commonly used methods of measurement include:
* The Lysholm score, which assesses knee injury recovery
* Isometric evaluation, which measures muscle tension without movement
* Manual evaluation of muscular strength, conducted by a healthcare professional
Isokinetic evaluation, which measures muscle strength with movement.
Preventing Quadriceps Tendon Rupture
The doctor and physiotherapist will create a tailored recovery plan for each patient. The length of therapy and the types of exercises recommended will depend on the nature of the injury, the surgical procedure performed, the patient’s overall health, and their specific needs after surgery. It’s important for patients to understand the active role they need to take in their own healing process.
Recovery typically takes at least four months, and most people find that their body has mostly healed within 6 months. However, many patients have noted that they didn’t fully meet their recovery objectives until a full year had passed.