What is Shoulder Impingement Syndrome?
Shoulder pain is a common reason why people visit their regular doctor or a bone and muscle specialist. This happens all around the world. It’s estimated that between 7% to 34% of patients report shoulder complaints, often due to a condition called shoulder impingement syndrome. This condition is believed to be the main cause of shoulder pain. It’s first description dates back to 1852, and it accounts for 44% to 65% of all shoulder pain complaints.
In the United Kingdom, 20% to 50% people seek treatment for shoulder pain from a general practitioner. Of these, 25% are diagnosed with shoulder impingement syndrome. Shoulder pain is not only common but also tends to persist or come back repeatedly. In fact, 54% of patients affected by shoulder pain report that their symptoms don’t go away even after 3 years.
What Causes Shoulder Impingement Syndrome?
It’s important to understand that shoulder external impingement is a different problem from internal impingement. In basic terms, external and internal impingement are determined by whether the issue is occurring outside or inside the rotator cuff, which is a group of muscles and tendons in the shoulder. Instances of internal impingement are commonly seen in people who often make overhead movements, like throwers or manual laborers. This can lead to issues, like damage to the rotator cuff, restriction in shoulder rotation (GIRD), or tears in the labrum, a piece of fibrocartilage in the shoulder.
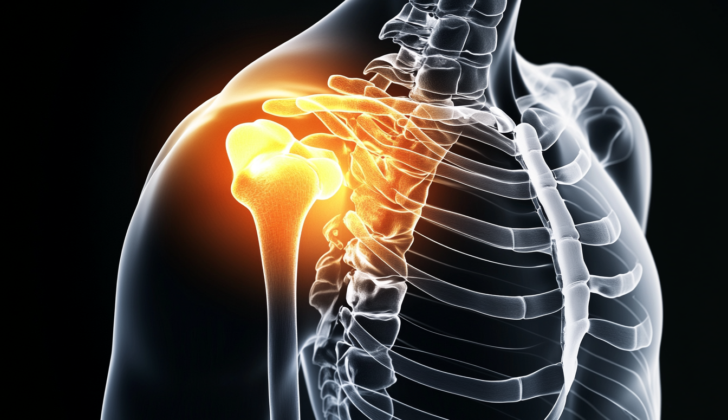
External impingement, also commonly known as shoulder impingement, is a painful shoulder condition due to inflammation and irritation within a particular space in the shoulder known as the subacromial space. We used to think of this as a single problem, but now we know it consists of many symptoms and anatomical issues.
The boundaries of the subacromial space are the acromion and coracoacromial ligament at the front, the acromioclavicular (AC) joint at the top, and the top of the upper arm bone (humerus) at the bottom. The acromion shape is believed to have role in the development of external impingement syndrome. This can be categorized into three types: flat, curved, and hooked acromion.
When you raise, move forward, or rotate your shoulder, the subacromial space usually narrows. This space is generally 1.0 to 1.5 cm wide, but it narrows when the top of the upper arm bone moves up and gets closer to the bottom edge of the acromion. The impingement pain occurs when this narrowing causes the upper arm bone to apply pressure to the rotator cuff or the subacromial bursa, the cushioning sac in the shoulder joint, or both.
Repeated injury, wear and tear, and fraying of the rotator cuff tendons are known to contribute to the narrowing of the subacromial space, but it’s unclear whether inflammation and tendon damage cause impingement or whether the narrowing causes the tendon inflammation.
Shoulder impingement syndrome can be categorized according to its location (external or internal) and/or its cause (primary or secondary). External impingement results from the physical encroachment of the soft tissue located within the subacromial space, while internal impingement occurs when the rotator cuff tendons become trapped between the upper arm bone and the rim of the shoulder socket. This is most common with the supraspinatus and infraspinatus tendons.
In primary impingement, the subacromial space becomes narrower due to structural changes, for instance, abnormal acromion shape or swelling of the soft tissues. Secondary impingement is characterized by normal anatomy at rest with the onset of impingement during shoulder movement, likely due to weakness of the rotator cuff. This weakens control of the upper arm bone’s movement. Secondary impingement syndrome can also be due to weak trapezius and serratus anterior muscles, which further limit shoulder movement and narrow the subacromial space.
The severity of shoulder impingement is classified into three stages by Neer. In stage I, impingement primarily results from swelling, bleeding, or both and typically happens due to overuse. Stage II is characterized by greater scarring and irreversible tendon changes. Chronic scarring can lead to a tear in the tendon, which characterizes stage III shoulder impingement.
Risk Factors and Frequency for Shoulder Impingement Syndrome
Shoulder impingement syndrome is often linked to activities that require a lot of repetition in overhead movements. This condition is common in people who do sports or jobs that demand such movements, like playing handball, volleyball, and swimming, or jobs like carpentry, painting, and hairdressing. There are also certain risk factors that can increase the chances of developing this condition, such as carrying heavy loads, experiencing an infection, smoking, and taking a specific type of antibiotic called fluoroquinolone. The likelihood of experiencing shoulder impingement syndrome goes up as you get older, with the majority of cases happening to people in their sixties.
- Shoulder impingement syndrome is often seen in people who do repeated overhead movements, like certain sports players and professionals like carpenters, painters, and hairdressers.
- Carrying heavy loads, having an infection, smoking, and taking fluoroquinolone antibiotics might increase your risk.
- The majority of shoulder impingement syndrome cases happen to people in their sixties.
Signs and Symptoms of Shoulder Impingement Syndrome
Shoulder impingement syndrome is a condition that can be diagnosed through a detailed medical history and physical examination. The common symptoms include pain while lifting the arm, discomfort when sleeping on the affected side, and loss of motion. Other related complaints could be weakness, stiffness, and disrupted sleep due to nighttime pain. These symptoms usually develop gradually, over weeks or months, and many patients aren’t able to pinpoint a specific injury that led to the pain. Pain is commonly felt over the upper side of the shoulder, often extending towards the middle of the upper arm.
Potential causes to investigate could include overhead activities and repetitive tasks. Relief might be experienced when resting, taking anti-inflammatory drugs, and using ice, but symptoms usually return upon restarting activities.
The physical examination is likely to include looking at and touching the shoulders and neck, comparing motion between the left and right side, and testing the strength of the areas. Weakness could be seen when lifting the arm away from the body and/or twisting the affected side outwards. There might be tenderness to the touch over the front part of the shoulder blade area of the affected arm.
Several special examinations can be performed to assist the doctors in diagnosing shoulder impingement syndrome. Even though these tests individually are not fully accurate, combined, they present a comprehensive picture of the condition. The four major tests include the Hawkins test, Neer sign, Jobe test, and a painful arc of motion.
- Hawkins Test: This is when pain is felt over the shoulder while turning the arm inwards at a right angle.
- Neer Sign: There is localized pain on the front of the shoulder when the arm is lifted.
- Jobe Test: This test is done by keeping the arms up and inward, with the patient trying to resist further upward movement (This may cause pain).
- Painful Arc of Motion: Any pain felt while lifting the arm sideways between 70 to 120 degrees.
There are also special tests to investigate shoulder instability, which is a different condition from shoulder impingement syndrome, these are commonly negative for shoulder impingement patients. These tests include the sulcus sign, anterior apprehension, and relocation test.
- Sulcus Sign: Here, the clinician applies a downward force at the elbow while the patient’s arm is at rest. If the upper arm bone descends, it’s deemed a positive test.
- Anterior Apprehension: The patient lies flat, and the arm is moved to ‘crank’ position (right angle to the body and bent at elbow). If the patient feels like the shoulder is about to slip out of the socket, the test is considered positive.
- Relocation Test: While the patient’s arm is in the ‘crank’ position and the patient feels an impending shoulder dislocation, the clinician applies a force pushing the shoulder head backward, relieving the patient’s discomfort.
Testing for Shoulder Impingement Syndrome
Physical examinations can often determine the cause of your symptoms with about 90% accuracy. However, to confirm the diagnosis and rule out other possible causes, your doctor may conduct imaging studies.
If radiographs (a type of X-ray image) are required, they will be taken from both sides, not just the affected one. This dual-sided approach allows your doctor to look for any natural variations in your anatomy and exclude other potential issues such as calcium build-up in the tendons (calcific tendinitis) or degenerative changes in the joints (arthritic changes).
Standard plain radiograph shoulder films usually contain two views: front on (AP) and from the side (lateral/scapular Y). The AP view helps your doctor measure the ‘critical shoulder angle’ (CSA). This measurement involves the extent of coverage provided by the acromion (a bone at the top of your shoulder) and the angle of the glenoid (the shoulder joint socket). If the CSA is greater than 35 degrees, there is an increased likelihood of a rotator cuff, a group of muscles and tendons around the shoulder joint, causing your symptoms.
Similarly, the measurement known as the ‘acromiohumeral distance’ (AHD) can help pinpoint issues related to the rotator cuffs. The AHD is the distance measured from the lower edge of the acromion to the top of your upper arm bone (the humeral head). The normal range is approximately 7 to 14 mm for men and 7 to 12 mm for women. A smaller AHD could suggest potential issues with the rotator cuff.
The lateral/scapular Y view allows your doctor to see how the humeral head positions on the glenoid. Other plain radiographs showing the outlet view help visualize and evaluate the shape of the acromion.
Shoulder ultrasound and magnetic resonance imaging (MRI) may also be used for further detailed assessments. Ultrasound, which can be done at your bedside, primarily helps examine soft tissues for conditions such as inflammation of a bursa (bursitis), damaged tendons (tendinopathy), and/or ruptured tendons. An MRI, which provides a detailed picture of both the bone and soft tissues in your shoulder, is usually recommended if there’s no improvement after six weeks of treatment.
Treatment Options for Shoulder Impingement Syndrome
Traditionally, shoulder impingement syndrome, a common cause of shoulder pain, is typically managed with exercise and physical therapy. If these treatments fail, or there are underlying structural issues, then surgery may be necessary. When there is no known severe structural damage, the usual course of treatment in the initial stage of 3 to 6 months includes exercises, NSAIDs (pain relievers like ibuprofen), and injections beneath the acromion – the bony tip of the shoulder.
A study found exercise therapy to give better results in the early stage of injury compared to a placebo. Physical therapy for this condition should focus on exercises designed to strengthen certain shoulder muscles, such as the rotator cuff muscles, the trapezius, and the serratus anterior. These exercises can help correct abnormalities in shoulder blade movement and balance upper body strength. Research suggests combining exercise with other treatments, like injections, can lead to greater improvements in pain relief than either treatment individually. Additionally, adding heat therapy to physical therapy can provide short-term symptom relief.
Where injections are needed, a commonly used method involves inserting a needle into the back part of the shoulder joint. The provider will typically use a local anesthetic and a corticosteroid (an anti-inflammatory medication). The aim is to inject the medication under the bone at the top of your shoulder, where it can help decrease inflammation. In some cases, using ultrasound for guidance during the procedure may provide better symptom relief.
Data from multiple studies suggest that surgery may not be more effective than physical therapy specifically targetting shoulder impingement for reducing pain. One type of surgery, Arthroscopic Subacromial Decompression (ASD), involves removing bone and soft tissue in the shoulder to relieve pressure and alleviate pain. This surgery is usually considered when a patient’s severe shoulder pain and functional limitations persist despite conservative treatments. Combining ASD with other treatments can have better effects than open surgery combined with injection of a substance from your blood that can promote healing. However, a review in 2018 found no additional benefit in pain reduction when comparing the results of ASD surgery to a placebo surgery after 12 months.
Other surgical options, including shaving down the bone (acromioplasty) or removing the bursa (a sac filled with lubricating fluid, located between tissues such as bone, muscle, tendons, and skin), may not provide much benefit. In fact, examining treatment where surgical intervention was paired with physiotherapy versus surgery alone, there was no substantial difference in pain or function up to 10 years later.
What else can Shoulder Impingement Syndrome be?
When diagnosing shoulder pain, various conditions can be responsible. These conditions may include:
- Adhesive capsulitis (Frozen shoulder)
- Rotator cuff tear
- Acromioclavicular joint arthritis (Shoulder arthritis)
- Acromioclavicular joint sprain (Shoulder sprain)
- Trapezius muscle spasm (Muscle spasm in the neck)
- Biceps tendonitis (Inflammation of the upper arm tendon)
- Biceps tendon rupture (Tear of the upper arm tendon)
- Calcific tendonitis (Calcium deposits in the tendons)
- Glenohumeral arthritis (Type of shoulder arthritis)
- Distal clavicle osteolysis (Bone loss in the collar-bone)
- Cervical radiculopathy (Nerve issue in the neck)
- Thoracic outlet syndrome (Condition affecting nerves in the lower neck and upper chest)
Please seek a healthcare professional’s advice if you are experiencing shoulder pain. They can help to identify the root cause and provide suitable treatment.
What to expect with Shoulder Impingement Syndrome
In around 60% of patients, methods such as physical therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroid injections, along with other non-surgical treatments, lead to satisfactory improvements within two years.
Possible Complications When Diagnosed with Shoulder Impingement Syndrome
Shoulder impingement syndrome can cause complications, mainly due to damage in the subacromial space (a space in the shoulder), altered mechanics, or muscle wasting from not using the shoulder. These complications can lead to various conditions:
- Rotator cuff tendonitis (inflammation of the rotator cuff tendon)
- Rotator cuff tear (tearing of the rotator cuff tendon)
- Bicipital tendonitis (inflammation of the biceps tendon)
- Bicipital tear (tearing of the biceps tendon)
- Adhesive capsulitis (stiffness or freezing of the shoulder joint)
Preventing Shoulder Impingement Syndrome
It’s crucial for patients to understand the importance of sticking to their physical therapy and home exercise programs. Additionally, making changes to their everyday activities can also help in their recovery. For example, they may need to stop doing activities that involve reaching overhead until their pain gets better.
One beneficial change they could make is to live “within the window”. This means they should try to limit their movements to an imaginary rectangle about 2 to 3 feet wide at the front of their body. By doing so, they can avoid reaching overhead or behind their back, which could cause further pain or injury.