What is Superior Labrum Lesions (SLAP tear)?
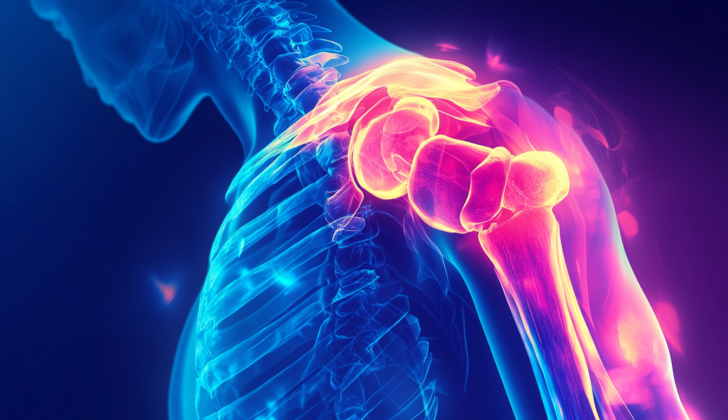
Superior labrum anterior to posterior (SLAP) tears are a specific type of injury to the labrum. The labrum is a cuff of cartilage which lines the shoulder socket, helping to keep the ball of the shoulder in place. These injuries can happen both suddenly or slowly over time. The first recognition and description of SLAP tears came in the 1980s, and since then, there has been a lot of research to better understand how to evaluate and treat it.
Treatment has to be specifically tailored to the patient. The best treatment approach could be non-surgical, such as physical therapy, or surgical, such as a labrum repair. It’s crucial to choose the right treatment for each individual so as to get the best possible outcome and minimize the risk of complications.
What Causes Superior Labrum Lesions (SLAP tear)?
SLAP tears are a type of shoulder injury where the top part of the labrum (a type of cartilage in your shoulder joint) gets frayed or torn from the socket (glenoid). If you think of the glenoid as a clock face, these tears usually occur in the area corresponding to 10 o’clock to 2 o’clock. There can be different types of SLAP tears, varying in how unstable the shoulder becomes and how much damage the labrum has.
This injury can happen in a few ways. First, it can happen suddenly due to a traumatic event causing twisting or compression forces on the shoulder. Activities that involve repeated overhead motions, like baseball pitching or manual labor, can also lead to SLAP tears due to the constant strain on the shoulder. Lastly, as people get older, their labrum naturally wears down, which can lead to SLAP tears as well.
Risk Factors and Frequency for Superior Labrum Lesions (SLAP tear)
The number of people suffering from SLAP tears is still a contentious issue. According to a 2012 study, SLAP tears were found to be more common in men than in women, with men experiencing this type of injury three times more frequently. The study highlighted that people in their 20s and 40s are at the highest risk, with incidences of SLAP repairs being 29.1 and 27.8 per 10,000 patients respectively.
Yet, other studies suggest that the rates can be anywhere between 6% and 26% when a person undergoes arthroscopy, a procedure used to diagnose and treat joint problems. Remarkably, some specific groups, such as overhead athletes, can have a SLAP tear prevalence of up to 83%.
It’s important to note though that not all SLAP tears are problematic or the main cause of symptoms. Sometimes, they are an incidental finding on advanced imaging tests or during an arthroscopy. Plus, they are often seen alongside other shoulder issues.
Signs and Symptoms of Superior Labrum Lesions (SLAP tear)
SLAP (Superior Labrum Anterior and Posterior) tears involve an injury to the labrum in the shoulder and can be difficult to diagnose because they often occur with other shoulder issues. Patients usually provide a detailed medical history, which includes information about when and how the symptoms began. This could range from a traumatic injury, doing activities where the arms are lifted above the head, or simply result from age-related conditions. Occasionally, there is no obvious cause of a SLAP tear, but a history of repetitive overhead activity can be a telltale sign.
Patient lifestyle is also critical for this diagnosis. Their involvement in sports, their job, daily activities, and personal goals can all factor into the condition. Typically, symptoms of SLAP tears include a deep, nonspecific shoulder pain, clicking sounds during movement, and discomfort during the night. Generally, these symptoms improve during periods of rest.
The initial examination usually includes looking for any noticeable differences in appearance between the shoulders and checking for muscle wasting. The skin is also examined for previous surgical scars or signs of injury. It’s important to conduct a thorough neurovascular assessment, including a muscle strength test. Movements are observed for both active (self-initiated) and passive (helped), and compared to the healthy shoulder. Attention is paid to the movement of the shoulder blade, as this can highlight an underlying SLAP tear. In addition, the stability of the shoulder is tested, considering that some types of SLAP tears can lead to instability. If instability is present, it’s necessary to evaluate the possibility of overall looseness of the body’s tissues. A Beighton score can be used as a measure of this.
No single physical examination can conclusively identify SLAP tears, but various tests can indicate an issue with the labrum or biceps. Here are some tests that can be used, but it is worth noting that these tests are not specific to SLAP tears as positive results can be found with other shoulder conditions.
- Biceps Tests:
- Speed’s test
- Uppercut test
- Yergason’s test
- Bicipital groove tenderness test
- Labral Tests:
- Anterior slide test
- Biceps load I and II tests
- Crank test
- Forced shoulder abduction and elbow flexion test
- Jobes relocation test
- Labral tension test
- Mimori pain provocation test
- Dynamic labral shear (O’Driscoll’s test)
- O’Brien (active compression) test
- Pronated load test
- Resisted supination external rotation test
Testing for Superior Labrum Lesions (SLAP tear)
The first step in examining a shoulder issue usually involves x-rays. X-rays are used to rule out bone-related issues. Chronic and long-lasting conditions may include degenerative changes in the shoulder. Sometimes, while tests of the superior labrum (a ring of cartilage that surrounds the shoulder socket) may be positive, it may not be the main cause of the pain.
A more detailed test, called a Magnetic Resonance Arthrogram (MRA), is often done to get a better look at the shoulder labrum. SLAP tear (a specific shoulder injury affecting this labrum) can vary in locations and severity, and it can be identified through this MRA test. Certain findings during this test, like a paralabral cyst (a fluid-filled sac near the labrum) could be a hint that there is a SLAP tear. Sometimes paralabral cysts can cause nerve compression, leading to weakness in the shoulder muscles.
Even though MRAs are pretty accurate with a sensitivity and specificity (ability to correctly identify those with and without the condition) between 82-100% and 71-98% respectively, there are normal variations in the shoulder anatomy which could be mistaken for a SLAP tear. Features such as a sublabral recess or foramen (small holes or spaces in the labrum area) could be misinterpreted as a labral tear. They are usually distinguished by their smooth edges, specific locations, and their inward orientation.
Other anatomical variations, like a thickened middle glenohumeral ligament (a ligament in the shoulder joint) and an absent anterosuperior labrum (a missing part of the labrum), can also be mistaken for a SLAP tear. Furthermore, a depression between the supraglenoid tubercle (a part of the shoulder blade) and the labrum might lead to false-positive results, making it seem like a SLAP tear is present when it isn’t. This is referred to as a pseudo SLAP tear.
There are several types of SLAP tears. The classification of these tears was first published in 1990 and since additional patterns of tears have been identified. Type I to Type X tears are differentiated based on their specific features, such as whether the biceps anchor (the point where the bicep tendon attaches to the labrum) is intact or damaged, whether the tear is like a bucket handle tear or a Bankart lesion (another type of shoulder injury that affects the labrum), and whether the tear extends to other areas of the shoulder.
Treatment Options for Superior Labrum Lesions (SLAP tear)
If shoulder pain is causing you trouble, the doctor may recommend starting with non-surgical treatments. These initially restrict movements that might worsen your shoulder’s condition. Usually, the first line of treatment includes anti-inflammatory drugs or corticosteroid injections which help to ease inflammation and pain. They will also recommend gentle range-of-motion exercises to gradually increase your shoulder’s movement capability.
In athletes who frequently perform overhead throwing actions, Glenohumeral internal rotation deficit (GIRD), which is a restricted inward rotation of the shoulder, is a common issue. Hence, part of the rehabilitation involves exercises to stretch the posterior (back) part of your shoulder, thereby aiming to improve the rotation. As the symptoms reduce, the physiotherapy sessions will shift the focus to exercises aiming to strengthen the rotator cuff (a group of muscles and tendons surrounding the shoulder joint) and other muscles around your shoulder joint.
For some patients, surgery may be necessary. The approach taken for surgery can depend on several factors, such as your activity level, goal for treatment, the type and severity of the tear in the shoulder tissue (also known as a SLAP tear), and other injuries that may exist alongside. In the early 2000s, there was an increase in repair surgeries for SLAP tears. However, more recently, trends are shifting towards a different surgery called tenodesis, which involves anchoring the tendon to the bone. This shift is due to a greater understanding of the injury, but the decision on the type of treatment remains centered on the patient’s specific situation.
For Type I and III SLAP tears, where the damage is less severe, a surgical cleaning procedure called debridement may be chosen. In more severe or unstable SLAP conditions, a repair with anchor fixation might be performed. The focus of all these techniques is to provide strong and stable repairs so that your shoulder joint regains stability and can undergo rehabilitation without any issues.
Sometimes, another approach is taken where the surgeon might sacrifice the biceps anchor, a part of your shoulder joint, and perform a tenotomy or tenodesis. A tenotomy involves cutting the tendon while tenodesis anchors the tendon to the bone. Although these methods are commonly used for young or highly active patients, they generally provide satisfactory results for a broad category of patients. Tenotomy may, however, lead to a slight change in the appearance of the bicep muscle. The treatment for the resultant tear of the shoulder tissue (labrum) could then vary based on its severity.
Finally, if you have a paralabral cyst, which is a fluid-filled sac near your shoulder joint, the treatment will depend on its location and whether it’s causing symptoms like nerve compression. If there are no symptoms, the doctor might recommend non-operative treatments like monitoring the cyst, prescribing anti-inflammatory drugs, or draining the cyst using a needle. If the cyst causes muscle weakness, pain, or muscle shrinkage (atrophy), surgical decompression, where the pressure caused by the cyst is relieved, could be suggested. It’s essential during such procedures to be careful to avoid further nerve damage.
What else can Superior Labrum Lesions (SLAP tear) be?
When discussing shoulder problems, we often consider several issues that may cause similar symptoms. Here are some examples:
- Biceps tendonitis: inflammation in the main tendon that attaches the top of the biceps muscle to the shoulder
- Internal impingement: a condition where the shoulder’s rotator cuff and labrum are pinched together within the joint
- Glenohumeral internal rotation deficit: a limitation in the shoulder’s ability to rotate internally
- Other labral pathology and/or instability: damage or abnormal positioning of the labrum, a type of cartilage found in the shoulder joint
- Rotator cuff tears: tears in the group of muscles and their tendons around the shoulder joint that stabilize it
- Scapular dyskinesis: abnormal movement or positioning of the shoulder blade
These conditions share common symptoms with one another, making an accurate diagnosis crucial for effective treatment.
What to expect with Superior Labrum Lesions (SLAP tear)
For many people with SLAP (superior labrum anterior to posterior) tears, which are injuries to the shoulder joint, non-surgical treatment can be quite effective and is often recommended as a first step. Research has shown this method to be successful for anywhere from 22% to 85% of patients.
On the other hand, surgical treatment in adults has also been shown to work well, with a success rate between 80% and 97%. However, these studies are pretty diverse, and what is considered successful treatment depends on how it’s defined. For some folks, it might mean the relief of pain and getting back their normal movement, but athletes who perform overhead activities may have a different view.
Indeed, many athletes may not be able to get back to their previous level of sports performance, with research showing rates of return to previous performance that range from just 7% to 84%. Athletes who don’t perform overhead activities tend to get back to sports at a higher rate consistently, but there are still some who can’t make a comeback. Along the same lines, teenagers have also shown good results with surgery in terms of pain relief and function, but returning to sports can be a concern here as well.
Worth noting is that for people over the age of 40, repairing the shoulder often produces inferior results compared to other procedures like tenodesis or tenotomy. Some experts even advise against repair in these age groups.
Ultimately, both non-surgical and surgical treatments can yield good results for many patients. However, the success of treatment largely depends on the functional level and treatment goals of the patient. It’s crucial to have an open and honest discussion with each patient about the potential outcomes before choosing the right path of treatment.
Possible Complications When Diagnosed with Superior Labrum Lesions (SLAP tear)
The success of treatment and the possibility of complications depend on several factors: The type of treatment, how strictly the patient follows the recovery plan, and specific characteristics of the patient like age, physical activity level, if the patient is overweight, if the patient is a woman, if the patient smokes, and other existing shoulder conditions.
Common Issues:
- Persistent pain and rigidity after surgical fixation
- Infection
- Inability of repair to hold
- Persistent pain
- Injury to nerves or blood vessels
- Repeated instability
In other words, the outcome can be influenced by many things and sometimes complications can happen, such as continued pain and stiffness, infection, unsuccessful repair, repeat instability, and nerve or blood vessels injuries.
Recovery from Superior Labrum Lesions (SLAP tear)
Recovering after surgery can depend on a few things. One important factor to consider is how the initial injury happened, so we can avoid doing the same things that could stress the surgical repair. For less complicated surgeries or SLAP patterns, patients usually start gentle movements and exercises in the first week after surgery. Care must be taken to not perform exercises involving the bicep muscle group. As patients feel less pain and their range of motion returns, they will be guided to do more strenuous exercises and activities specific to their sport.
On the other hand, more careful steps are needed for complicated SLAP repairs. These patients typically use a special sling and avoid movements that require external rotation and lifting away from the body. The first four weeks involve gentle exercises that slightly test the range of motion but very carefully. It’s only after about five to six weeks that patients will start doing strengthening exercises and slowly allowed to perform active rotation and lifting motions. However, exercises that involve the biceps continue to be avoided. A systematic program will be followed to increase strengthening and sports specific activities over the next several months. Depending on pain and progress, patients can slowly return to their sport between six to nine months after surgery.
For surgeries involving the bicep tendons, which include tenotomy and tenodesis, the above programs still apply. Though, patients who have isolated tenotomy can typically resume activity within a week. For tenodesis patients, it’s recommended to protect the area for four weeks, including avoiding twisting and flexing at the elbow. Strengthening exercises for these patients can be started six weeks after surgery.
Preventing Superior Labrum Lesions (SLAP tear)
Talking about the ways the body’s structure can contribute to worsening symptoms can help us understand why certain everyday actions should be avoided after treatment or surgery. It’s also important to talk about what you, the patient, hope to achieve through treatment, because the time it takes to recover from various procedures can be quite different. Knowing about the intense therapy needed after more advanced procedures can give you a clear idea of what will be required from you on your journey to recovery.
To help prevent injury, particularly in people who play sports that involve a lot of arm movement, we should focus on increasing flexibility and strengthening the muscles around the shoulder and scapula (which is the technical name for the shoulder blade). We also need to ensure that these activities are done correctly. This can help prevent overloading the shoulder’s support structures, and avoid placing too much pressure on the area where the shoulder socket meets the labrum (the soft tissue that adds depth to the shoulder socket). This is especially important in the prevention of further injury.