What is Trigger Finger (Stenosing Flexor Tenosynovitis)?
Trigger finger, also medically known as stenosing tenosynovitis, is a common issue that happens due to overuse of the fourth finger and thumb. This can lead to significant problems in using the affected finger and a condition called tenosynovitis within the flexor sheaths, which are the coverings of the tendons in the fingers and thumb. The trigger finger condition is caused by a narrowing of these sheaths, with an enlargement and inflammation at the meeting point of the tendon and sheath. This inflammation can cause lump-like formations on the tendon.
Although the issue most commonly shows up in the ring finger and thumb, it can affect any finger. The main area involved in trigger finger is the A1 pulley sheath located at the main joint of the finger (metacarpophalangeal joint), which is the beginning section of the tendon sheath. Still, it can also occur at the A2 (the joint near to the middle of the finger, proximal interphalangeal joint) or A3 (the joint closest to the tip of the finger, distal interphalangeal joint).
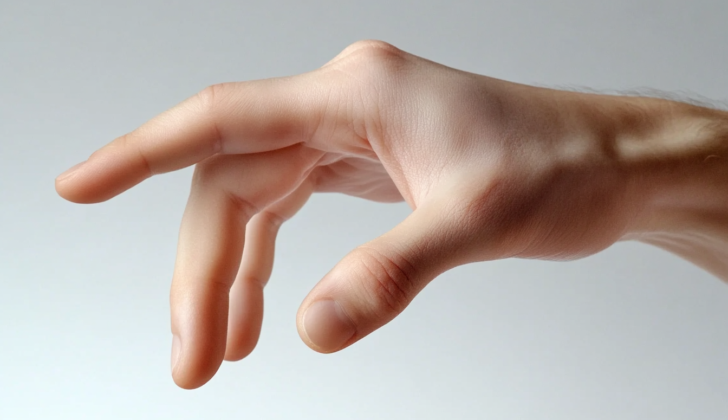
Patients usually report a locking feel with their finger both when bending it and straightening it out, with straightening it out typically presenting more difficulty.
People who have trigger finger experience pain and a strange discomfort in the palm while moving the affected finger. They may hear a clear snapping sound as they bend and stretch the finger. The condition often affects the hand we use the most, with the thumb and ring finger being the most commonly affected.
What Causes Trigger Finger (Stenosing Flexor Tenosynovitis)?
Trigger finger is a condition that can be caused by many factors and is often linked to certain other health conditions in adults. These can include diabetes, amyloidosis (a condition where abnormal proteins build up in your tissues and organs), carpal tunnel syndrome (a nerve condition affecting the hand and arm), gout, thyroid disease, and rheumatoid arthritis (a type of arthritis that causes inflammation in the joints).
This condition happens when the tendon in the finger becomes thick and inflamed due to injury or overuse, causing feelings of catching or locking because it can’t easily slide within its protective sheath. Trigger finger can also be caused by certain unusual features of the hand’s anatomy, like the attachment of a small muscle to a specific part of the tendon sheath.
In children, trigger finger is usually caused by the tendon of the thumb being too big for its sheath. This happens due to an increase in the number of fibroblasts (cells that produce collagen and other fibers) which causes a mismatch in size between the thumb tendon and its sheath. Most of the time, we don’t know the exact cause of trigger finger in children. However, it can also be associated with inherited metabolic conditions (like Hurler syndrome) and inflammatory conditions (like juvenile rheumatoid arthritis).
Risk Factors and Frequency for Trigger Finger (Stenosing Flexor Tenosynovitis)
Trigger finger mostly appears at two different stages of life. The first peak happens in children under 8 years old, and the second peak is seen in adults between the ages of 40 and 50. Although the condition is more common in adults, kids both boys and girls may also experience this problem, where it often impacts the thumb. In the case of adults, trigger finger is found more frequently in women, usually affecting the hand they use most.
- Trigger finger has two main periods where it is most common: in children under 8, and in adults between 40 and 50 years old.
- This condition is more often seen in adults than in children.
- In children, both boys and girls can get trigger finger, and it usually affects the thumb.
- Among adults, trigger finger is more likely to affect women, generally in the hand they use most frequently.
Signs and Symptoms of Trigger Finger (Stenosing Flexor Tenosynovitis)
Trigger finger is a condition that causes discomfort or limits finger movement. Patients may experience symptoms such as stiffness, discomfort, or increasing pain in the palm of the affected finger when it’s bent. The pain is often followed by what feels like a painful clicking sensation in the finger. Some patients’ fingers might get locked during stretching, or they might be unable to move a finger from a bent position. It’s also common for this condition to affect a person’s ability to work. The symptoms can come on gradually or suddenly.
During a physical examination, the doctor might notice a tender lump or swelling at the base of the palm of the affected hand. The finger might be bent and locked in place, and trying to move it could cause pain and/or a snapping sound.
Testing for Trigger Finger (Stenosing Flexor Tenosynovitis)
A diagnosis of trigger finger is mostly based on symptoms and physical examination. If you have a finger that locks when you try to bend it, makes a painful clicking sound, or gets stuck when stretching it back out, your doctor might suspect trigger finger. If you also have a bump or swelling at the bottom of the affected finger, this additional symptom may further support a diagnosis of trigger finger.
Ultrasound scans are typically the best way for doctors to evaluate this condition. Using sound waves to create images of the inside of your body, the ultrasound shows both stationary and moving pictures of the trigger finger and can be compared with your normal fingers. Through an ultrasound, your doctor might see a thickened pulley (a part in your finger that helps control finger movement), inflammation (internal swelling), and uneven areas of the connected tendon (flexor tendon), a thick cord in your hand that helps you flex your fingers. While ultrasound can show these problems, it may not always clearly pinpoint where the issue is. An ultrasound can also show the snapping and clicking issues that occur during the flexing of the tendon.
Doctors might also use a plain X-ray to make sure that symptoms aren’t caused by other conditions such as concealed fractures or breaks in the finger bones. That being said, more complex imaging machines like Computed Tomography (CT) scans or Magnetic Resonance Imaging (MRI) scans are generally not required to diagnose trigger finger.
Treatment Options for Trigger Finger (Stenosing Flexor Tenosynovitis)
There are two main methods for managing ‘trigger finger’ – a condition where your finger or thumb gets stuck in a bent position. These methods include non-surgical approaches, such as steroid injections and splints, or surgical procedures.
Non-Surgical Approaches
If you have trigger finger, your doctor might first recommend non-surgical treatments, especially if your symptoms have just started. This could include steroid injections or splinting.
With a steroid injection, your doctor injects medicine into the sheath around your tendon. This approach is often effective, easy to do and less invasive than surgery. It can also provide quick relief. However, keep in mind, even though an injection can help, there’s a chance your symptoms could return. Side effects can include tissue shrinkage, skin discoloration, or infection. Also, if your symptoms have been going on for a long time, this approach may not work as well.
The injections can be done either by ‘feel’, or using an ultrasound machine to guide the needle to the right spot. Studies have shown that using ultrasound can be more effective, with better results and faster return to work.
If you’ve been given a splint, it’s designed to limit the movement of your tendon and reduce swelling. Doctors often recommend wearing a hand splint for 6 to 10 weeks, but this may not work as well if your symptoms are severe or long-lasting.
One study tested three options – steroid injection, splinting, or a combination of both – and found no major difference in pain relief or function after a year. So, starting with a splint might be a good option for anyone with trigger finger.
Surgical Approaches
If non-surgical treatments don’t help, or you have a severe case of trigger finger, you might need surgery. The standard surgical treatment is to open and release the A1 pulley – a band of tissue that your tendons slide through.
There’s also a less invasive option, called percutaneous release. However, this technique requires a high degree of skill and knowledge to avoid damaging the tendon or nerves. Some doctors are hesitant to use this approach on the thumb because the nerve runs very close to the A1 pulley. One study found this technique works 87% of the time, but it’s more likely to fail on the index, middle or ring fingers.
Open release surgery and percutaneous release often have similar outcomes. For persistent or recurring trigger fingers, your surgeon might recommend another surgical procedure: removing one or more segments of the flexor digitorum superficialis, a tendon in your finger. This is particularly useful for people with diabetes, rheumatoid arthritis, or those whose finger is permanently bent.
One thing to note, having more than three steroid injections before surgery, or doing manual labor can increase your chances of trigger finger returning after treatment. So, a fourth round of steroid injections is typically avoided.
For advanced cases, where the fingers have limited movement, a surgery to reduce the tendon may be necessary to increase the range of motion. Post-surgery, you may need physical therapy or to wear a splint for a little while to get the best results.
What else can Trigger Finger (Stenosing Flexor Tenosynovitis) be?
If someone is showing symptoms of this condition, a doctor might consider several other possible causes. These could include:
- Abnormal sesamoids (small bones embedded in tendons)
- Acromegaly (a disorder that results from excess growth hormone)
- Wrist ganglion cyst (a lump filled with fluid that develops near a joint or a tendon)
- Ganglion involving the tendon sheath (fluid-filled sac on the tendon sheath)
- Infection within the tendon sheaths
- Presence of a loose body in the MCP joint (small fragments of cartilage or bone within the joint)
- Subluxation of extensor digitorum communis (partial dislocation of the tendon that extends the fingers)
- Osteophytes on the metacarpal head (bone spurs on the large bone in the hand)
- Palmar plate dislocation (dislocation of a ligament in the hand)
- Boxer’s knuckle (an injury to a knuckle caused by repetitive punching)
What to expect with Trigger Finger (Stenosing Flexor Tenosynovitis)
The future looks positive with the right treatment. Most patients react well to injections of a medicine called corticosteroids, but some may get better on their own if the root cause of their condition is treated. However, complete recovery might take a few months after a corticosteroid injection.
People with diabetes might not have such a good response to corticosteroids and may likely need surgery. The surgery to fix trigger finger, where the finger gets stuck in a bent position, has high success rates and is suggested if the condition doesn’t improve after corticosteroid injections.
Possible Complications When Diagnosed with Trigger Finger (Stenosing Flexor Tenosynovitis)
An open A1 pulley release, typically done to alleviate the symptoms of a condition called “trigger finger,” is generally safe with very few complications. Most of the issues that occur are minor and include things like discomfort at the scar site, pain, the recurrence of the triggering sensation, and a mild lag in extending the finger. Serious complications are rare, occurring in between 1% and 4% of cases. These can include injury to the nerves and blood vessels in the area, a condition called “bowstringing” where the flexor tendons stand out from the finger, and infection requiring further surgery. There’s also a small chance that bowstringing could lead to a finger deformity known as a swan neck deformity.
Common Side Effects:
- Scar tenderness
- Pain
- Recurrence of triggering
- Mild extension lag
- Neurovascular bundle injury
- Bowstringing
- Infection requiring further surgery
- Swan neck deformity
Preventing Trigger Finger (Stenosing Flexor Tenosynovitis)
Trigger finger is a common condition that can make it hard to use your hand. It can become more frequent and severe if you have diabetes. The initial treatment usually involves wearing a splint on the affected finger. If the splint isn’t helping, a doctor might give you a steroid injection in the area around your tendon, which can significantly reduce pain for most people. If these treatments don’t work, the doctor may suggest a surgical procedure to cut the “A1 pulley” – a part of your hand that’s causing the problem. This surgery is widely accepted as the best solution when other treatments are not effective.