What is Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)?
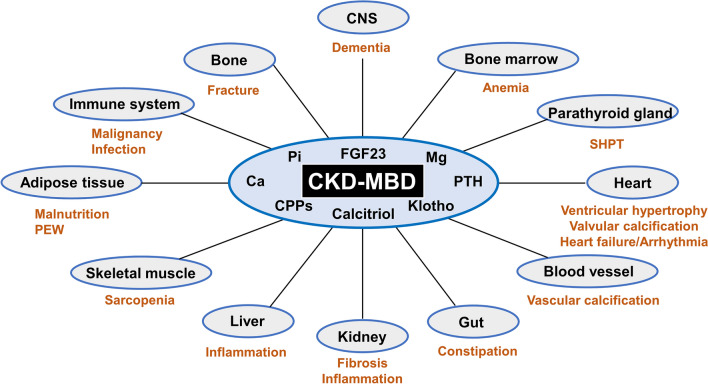
In 2005, a term was created by Moe and his team to describe a complicated health problem relating to the kidneys, called chronic kidney disease-mineral and bone disorder (CKD-MBD). This condition involves issues with calcium, phosphate, parathyroid hormone, vitamin D, and fibroblast growth factor-23 metabolism, leading to changes in bone shape, vascular calcification (hardening of the arteries and veins), and heart-related deaths in patients with chronic kidney disease. These abnormalities can potentially result in high mortality rates, primarily due to heart-related problems. Since CKD-MBD was identified, various clinical guidelines have been created to help manage the disease and improve patient outcomes. CKD-MBD can be assessed through a bone biopsy, and changes in serum levels of calcium, phosphorus, parathyroid hormone, and vitamin D are significant to this disease. Although most features appear when the kidney function decreases beyond a specific rate, some elements like loss of Klotho (a protein), increased FGF23 secretion, decreased bone synthesis rates, and vascular calcification often happen before abnormal lab results are detected. Studies evidence that these abnormalities lead to increased risks like fractures and heart-related deaths.
Important findings have shed light on the development of CKD-MBD, including the roles of FGF23, Klotho, Wnt inhibitors, and activin A. Management strategies mainly focus on preventing harmful effects associated with secondary hyperparathyroidism. Managing secondary hyperparathyroidism involves established indicators of disturbed mineral bone metabolism, such as serum calcium, phosphate, parathyroid hormone and vitamin D. Renal osteodystrophy, a facet of CKD-MBD, represents changes in bone shape. While a bone biopsy is the best way to diagnose and classify it, it is rarely done. ‘Kidney Disease Improving Global Outcomes’ recommends monitoring the trend of biochemical markers for managing renal osteodystrophy, and since a 2017 update, bone biopsy isn’t recommended before starting these medications.
What Causes Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)?
CKD-MBD is a complex condition that results in a variety of health issues, including issues related to the chemistry of the body, changes to body structure, bone problems, and issues that affect different parts of the body. There are many contributing factors, but a few key ones are outlined below.
Firstly, when the kidneys aren’t working right, it can lead to CKD-MBD. The kidneys are responsible for keeping a delicate balance of minerals and electrolytes, like calcium and phosphate, in the body. When kidney function decreases, this balance can get thrown off, leading to CKD-MBD.
Secondly, in someone with Chronic Kidney Disease (CKD), the reduced kidney function can cause a buildup of phosphate and a decrease in active vitamin D in the body. This results in too much phosphate and not enough calcium in the body – a state that can lead to issues like hardening of the blood vessels, related to CKD-MBD.
Finally, when kidney function is impaired in CKD, it can mess up the regulation of PTH, a hormone produced by the parathyroid glands. This can lead to hyperparathyroidism, a condition of excessively high levels of PTH in the blood. When there’s too much phosphate, not enough calcium, and not enough vitamin D, this can lead to the release of excessive PTH. This disrupts the balance of calcium in the skeletal system and is a major contributing factor to bone diseases associated with kidney diseases.
Secondary hyperparathyroidism is a significant part of CKD-MBD, often identified and monitored using PTH levels. It happens due to various factors that trigger and maintain the overproduction of PTH. This leads to phosphate retention, decreased calcium concentration, decreased levels of activated vitamin D, increased concentration of a hormone called FGF23, and reduced expression of various receptors in the parathyroid glands. As kidney function decreases, changes to these factors help to understand the development of secondary hyperparathyroidism.
To understand phosphate retention better, it’s worth considering the “tradeoff” hypothesis, which suggests that while initially, an increase in PTH helps balance phosphate levels and other imbalances in the body, in the long term, continuously high levels of PTH can be harmful. And in advanced stages of CKD, the compensatory increase in PTH becomes insufficient, leading to a continuous increase of phosphate levels.
Too much phosphate in the blood, known as hyperphosphatemia, has found to contribute to several health issues in patients with CKD-MBD. These include causing more FGF23 secretion, which suppresses PTH secretion, and contributing to hardening of the blood vessels.
When kidney function starts to go downhill, the concentration of calcitriol, the active form of vitamin D, can decrease. Initially, this is caused by increased FGF23. But, in more advanced CKD, the loss of functioning kidney tissue also contributes to the decrease. This lack of vitamin D created by the kidneys is pivotal to the dynamic between various factors involved in CKD-MBD, including phosphate, calcium, PTH, FGF23, and Klotho, a protein that binds to the FGF23 hormone.
No surprise that calcium plays a major role in managing PTH secretion. The parathyroid glands are very sensitive to changes in the levels of calcium in the blood. Lower than normal calcium levels and high calcium levels both contribute to increased death rates among kidney disease patients. Lower than normal calcium levels, also known as hypocalcemia, is common in CKD and leads to too much PTH secretion, resulting in abnormal bone changes. High calcium levels, also called hypercalcemia, is linked to calcium buildup outside of the bones.
The FGF23 plays a key role in managing PTH levels. Its levels rise even before PTH increases, in response to vitamin D, dietary phosphate, calcium, and PTH. Additionally, FGF23 helps maintain normal serum phosphate levels by decreasing phosphate reabsorption in the kidneys and inhibiting its absorption in the intestines by reducing the production of calcitriol. As a result, it increases the removal of phosphate in the urine and reduces its absorption in the gut, lowering serum phosphate levels. Suddenly a rise of FGF23 suppresses PTH secretion. Klotho, a protein mainly found in renal tubes, is crucial in activating FGF23 receptors and may also affect bone formation and bone mass. Not having enough Klotho leads to an increase in FGF23 levels, while an increase in FGF23 concentration exacerbates Klotho deficiency due to low vitamin D levels.
Risk Factors and Frequency for Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)
Chronic kidney disease-related mineral and bone disease (CKD-MBD) appears in a variety of forms, and how common it is will depend on the specific parts of the illness. One example is hardening of the arteries, which is more frequent in those having dialysis, with over 80% of these patients developing heart-related artery hardening. Different studies have varying results on how many people have CKD-MBD, but most recent data suggests a prevalence between 55% and 86%.
In recent years, there’s been a change from bone diseases caused by overactive parathyroid glands to bone diseases that show little to no activity (adynamic bone disease). This shift is thought to be due to several reasons:
- Excessive use of vitamin D variants that decrease parathyroid hormone (PTH) levels.
- Chemicals that bind to calcium in the body also lower PTH levels.
- People on long-term dialysis who also have diabetes usually have lower PTH levels, resulting in more instances of low bone activity.
- A decrease in a type of bone disease called osteomalacia due to the use of non-aluminum-based chemicals that bind to phosphates and more effective water treatment processes for dialysis.
Signs and Symptoms of Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)
CKD-MBD (Chronic Kidney Disease-Mineral and Bone Disorder) can lead to symptoms that develop gradually. In the early stages, patients may not show symptoms until treatment begins. The symptoms can include bone pain and muscle weakness near the body’s midsection. In severe cases, especially in children and adolescents, long bones might erode, leading to noticeable bone deformities. Also, the condition can lower the effectiveness of treatments like erythropoietin therapy.
There is another condition called aluminum-induced osteomalacia that can cause general bone pain, frequent fractures, and muscle weakness as well. It can also lead to anemia and dementia due to excess aluminum in the body. However, thanks to increased awareness about aluminum toxicity, these cases are becoming less common. It’s important to know that aluminum buildup occurs more rapidly in the bones of children and younger patients compared to older patients, and it’s more prevalent in patients with type 1 diabetes.
Low turnover states that result in poor mineralization can also be symptomatic. Bone pain is a primary symptom for patients suffering from a condition called adynamic bone disease. These patients tend to be at a higher risk for fractures, and in children, growth impairment might occur. If not managed properly, this could also progress into vascular calcification.
In patients with CKD’s bone disease, there are distinctive signs such as an overly suppressed PTH level, which may lead to high calcium level in the blood (hypercalcemia). This condition can cause calcifications in blood vessels, leading to hypertension, which could increase the likelihood of cardiovascular events or strokes. Other complications related to high levels of calcium, phosphorus, and parathyroid hormone (PTH) include calciphylaxis.
The bone disorder in children with CKD leads to fractures, bone pain, necrosis (death of bone tissue due to lack of blood), growth failure, and skeletal deformities. There are even rare cases where the disorder can lead to intracranial hypertension due to constriction (stenosis) of the hole in the skull where the jugular vein passes (jugular foramen).
Patients, especially ones with secondary hyperparathyroidism caused by chronic kidney disease, may show signs of renal osteodystrophy. This includes hardening of the bones and destruction of the outer layer of bones, and in severe cases, excessive thickening of the skull and facial bones.
Testing for Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)
When it comes to diagnosing CKD-MBD (Chronic Kidney Disease-Mineral and Bone Disorder), the process can be quite tricky as most patients do not show symptoms at the beginning of the disease. Doctors may get suspicious and start investigating when symptoms become apparent.
Even though a bone biopsy is the best way to confirm the disease, it’s not always possible because it’s an invasive procedure. Hence, doctors may rely on blood tests and radiological images to get a better idea of what’s going on. These different measures can help doctors narrow down their diagnosis.
The blood tests usually check for specific markers which indicate bone activity. One key marker is PTH (Parathyroid Hormone) – it plays a significant role in this disease and can indicate if the bone turnover is high or low. It’s important to note that the normal levels of PTH can vary depending on whether or not the patient is undergoing dialysis.
When the PTH levels are higher than usual, doctors usually check the vitamin D levels in the blood next. They also monitor the calcium and phosphate levels to help confirm the diagnosis. Other markers – like bone-specific alkaline phosphatase (bsALP), osteocalcin, and propeptide of type I collagen – are also present but not commonly used.
Radiological imaging, like x-rays and DEXA (Dual-energy x-ray absorptiometry) scans, help doctors understand the nature of the bone disease connected with CKD-MBD. For example, these scans can detect changes in bones that point towards renal osteodystrophy. DEXA scans measure bone density but their reliability in these cases is still debated.
In addition to these tests, doctors might also recommend a bone biopsy – the definitive test for diagnosing this disease. However, a new marker, FGF23, is also gaining attention. Despite its established effects, it is not frequently used due to issues like instability, cost, and lack of precision.
Once diagnosed, patients with CKD-MBD are regularly monitored by measuring their calcium, phosphate, and PTH levels in the blood. Some healthcare providers might also monitor bsALP to decide if a surgical intervention is necessary. While there’s no set standard for how often these tests should be done, it’s generally recommended to check calcium and phosphate every 1 to 3 months and PTH every 3 to 6 months. However, this might be subject to change based on the patients’ treatment plan. Vitamin D levels are usually checked on an annual basis.
Treatment Options for Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)
The management of patients with chronic kidney disease and mineral bone disorders (CKD-MBD) takes into account the features of kidney impairment, bone disease, and disruptions in normal levels of phosphate, calcium, vitamin D, and PTH.
Treatment procedures for adult patients who are not on dialysis differ from those for dialysis patients. If you have CKD and your estimated glomerular filtration rate (eGFR) is less than 60 mL/min/1.73 m2, you are at risk for secondary hyperparathyroidism. Therefore, it’s essential to monitor your PTH, calcium, phosphate, 25-hydroxy vitamin D, and bsALP levels.
Treatment emphasises reducing serum phosphate levels to below 5.5 mg/dL to reduce elevated PTH levels. Consider a low-phosphorus diet, especially vegetarian meals. If high serum phosphate levels persist, doctors may recommend medicine called phosphate binders taken with meals. Non-calcium-based binders like sevelamer and lanthanum are preferable as these don’t impact calcium levels. In cases of low levels of calcium requiring supplements, doctors may recommend calcium-based binders.
The treatment approach differs for calcium. Patients with mild low calcium levels that are symptom-free typically don’t require calcium or vitamin D treatments, as these could lead to high calcium levels or a surplus of calcium.
Vitamin D deficiency often appears in early lab reports of CKD patients and may trigger hyperparathyroidism and low calcium levels. Supplements of cholecalciferol or ergocalciferol are generally recommended.
In case you’re suffering from persistent or progressively worsening hyperparathyroidism, treatments target triggers such as vitamin D deficiency, high levels of phosphorus, and high phosphate intake. If these methods don’t reduce PTH levels, use of calcitriol can be considered.
For CKD patients on dialysis, the recommended phosphate levels range from 3.5 to 5.5 mg/dL, while calcium levels should stay below 9.5 mg/dL. PTH levels should not go beyond 2 to 9 times the assay’s upper limit.
Sensibly managing phosphate is key for patients with persistently high phosphate levels, as high levels can make high PTH treatments complicated due to potential increases in serum phosphate. Limiting phosphate in foods and using phosphate binders are often the first strategies.
Maintaining calcium levels under 9.5 mg/dL is also crucial. Mild and symptom-free low calcium conditions usually don’t require treatment.
In matters of vitamin D, rectifying vitamin D deficiency is essential, as low levels have been linked to higher death rates among hemodialysis patients.
Also, options for treating hyperparathyroidism include calcimimetics, calcitriol, synthetic vitamin D analogs, or a combination to decrease PTH levels.
What else can Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23) be?
When doctors see signs that a patient may have bone disease or structural irregularities in their bones, they perform tests like checking the levels of PTH, alkaline phosphatase, calcium, and phosphate. If the patient has a history of Chronic Kidney Disease (CKD), it could suggest they have a bone disorder related to CKD called CKD-MBD. But to arrive at the correct diagnosis, doctors must also consider and rule out other possible causes, such as:
- Thin bones (osteopenia)
- Weak, brittle bones (osteoporosis)
- Vitamin D-resistant rickets, a condition causing soft, weak bones in children
- Osteopetrosis, also known as marble bone disease, which is a rare disorder causing bones to harden
- Paget’s disease of the bone, leading to the formation of fragile and misshapen bones
Ensuring the accurate diagnosis is of utmost importance as it guides the doctors towards the right treatment plan.
What to expect with Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)
Several research studies have aimed to find a link between altered mineral metabolism in patients with Chronic Kidney Disease (CKD) and the rates of death. Findings from one such study, the Dialysis Outcomes and Practice Patterns Study (DOPPS), showed a clear connection between abnormal mineral metabolism, including elements like parathyroid hormone (PTH), phosphate, calcium, vitamin D, and the product of calcium and phosphorus, and the risk of dying from any cause or heart disease.
High phosphate levels in the blood have been investigated as a reason for increased death rates, especially in patients with CKD who are not undergoing dialysis. A significant study which included almost 5000 patients with CKD showed that for each milligram increase in blood phosphate levels beyond the normal range, there was a 35% increased risk of death.
Full recovery from a condition known as renal osteodystrophy typically requires a kidney transplant. However, in determining the overall outlook for this condition, it’s important to take into consideration other factors such as the bone-vascular axis. This includes vascular calcifications, hardening of blood vessels, and related heart events, all of which are common in patients with renal osteodystrophy. Understanding and dealing with these interrelated factors is vital in influencing the eventual outcome for patients with this condition.
Possible Complications When Diagnosed with Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)
Chronic kidney disease-mineral and bone disorder (CKD-MBD) is a complication that can occur as a result of chronic kidney disease (CKD). When patients develop this condition, they often feel pain in their bones, have changes in their bone shape, and can even show signs of slowed growth in children. CKD-MBD can also gradually worsen heart health, leading to changes in the heart’s shape and hardening of the arteries.
However, managing CKD-MBD with treatments like lower calcium dialysate and calcimimetics may cause dangerous irregular heart rhythms, due to an increased heart rate duration (QT prolongation). Abrupt fatal heart events such as sudden heart failure or sudden cardiac death from severe irregular heart rhythms are a distinctive problem that can be seen as part of the CKD-MBD-specific heart complex syndrome. Studies have shown that patients with bone disease caused by kidney disease and a history of initial fragility fracture are more likely to experience cardiovascular events like heart diseases and metastatic calcification (hardening of tissues due to calcium deposits).
Additionally, CKD-MBD can be associated with other complications like:
- Increased infections
- Muscle weakness
- Irregular heart rhythms (arrhythmias)
- Increased risk of hemorrhagic stroke (a stroke caused by bleeding in the brain)
Preventing Chronic Kidney Disease-Mineral Bone Disorder (CKD-MBD) (Kidney Disease Causing Disruptions in Calcium, Phosphate, Parathyroid hormone , Vitamin D, and Fibroblast growth factor-23)
Patients need to understand how phosphate, calcium, vitamin D, and PTH affect their health condition. Meeting with a dietitian for personal diet advice is also very important. The dietitian can help them know how to limit phosphate in their diet but still get enough protein. This is key as malnutrition is common in this disease, and reducing phosphate intake can help avoid further complications. The patients must also understand the different kinds of phosphate binders and why they should be taken during meals. In some cases, they may also need to take extra calcium and vitamin D.