What is Renal Artery Stenosis?
Renal artery stenosis is a condition where one or both of the arteries that carry blood to your kidneys become narrower. This is a significant cause of high blood pressure and is estimated to cause between 1% to 10% of all high blood pressure cases among the 50 million people affected in the United States. Two conditions usually cause it; one is a disorder called atherosclerosis, a narrowing and hardening of the arteries due to fat buildup, and the other is fibromuscular dysplasia, a condition causing abnormal cell growth in the artery walls. Other complications linked to renal artery stenosis include chronic kidney disease, a long-term condition where the kidneys don’t work as well as they should, and end-stage renal disease, a severe kidney disease that requires dialysis or a kidney transplant.
What Causes Renal Artery Stenosis?
Unilateral renal artery stenosis (RAS) is a condition where the blood flow to one kidney becomes slow or blocked due to narrowing of the renal artery. It has two major causes:
1. Atherosclerosis (accounting for 60% to 90% of the cases): Atherosclerosis is a condition where the arteries become hardened due to plaque buildup and it most frequently occurs in men over the age of 45. The blockage typically occurs either at the beginning of the renal artery or within the first 2 centimeters. While this condition is common in people who have hardened arteries (atherosclerosis), it can also occur on its own in the kidney. Additionally, it can affect any of the multiple renal arteries, which happens in 14% to 28% of the cases. Risk factors for atherosclerosis include high cholesterol, smoking, viral infections, immune injury, and increased homocysteine or protein levels in the blood.
2. Fibromuscular dysplasia (makes up 10% to 30% of RAS cases): Unlike atherosclerosis, fibromuscular dysplasia impacts mainly women under the age of 50. It typically affects the middle to distant main renal artery or the branches within the kidney.
Other causes, which are less common and make up less than 10% of the cases, include thromboembolic disease (a clot blocking a blood vessel), arterial dissection (partial tearing of the artery wall), abdominal aortic aneurysm (an abnormal bulging in the main blood vessel), vasculitis (inflammation of the blood vessels) which includes conditions such as Takayasu arteritis, Buerger disease, polyarteritis nodosa, as well as radiation effects, neurofibromatosis type 1 (a genetic disorder leading to tumor growth on nerves), and retroperitoneal fibrosis (a rare disease that causes inflammation and excess fibrous tissue growth around the kidneys).
Risk Factors and Frequency for Renal Artery Stenosis
Renal artery stenosis, a narrowing of the arteries that carry blood to the kidneys, is less common in patients with mild high blood pressure – less than 1%. However, among those with acute, severe, or hard-to-treat high blood pressure, this condition can be present in up to 10% to 40%. Studies indicate that unilateral stenosis, or narrowing of one artery, is more prevalent than bilateral stenosis, or narrowing of both, with rates ranging from 53% to 80%.
Also, it is suggested that ischemic nephropathy, a kidney condition caused by an insufficient flow of blood to the kidneys, could be responsible for 5% to 22% of advanced kidney disease in people over 50. Patients with fibromuscular dysplasia, a condition that affects the muscular walls of arteries, often have their renal arteries affected – from 75% to 80% of cases. Around two-thirds of these patients have multiple renal arteries involved. Fibromuscular dysplasia is more common in females than in males.
- Less than 1% of patients with mild high blood pressure have renal artery stenosis.
- However, this can increase to 10% to 40% in cases of acute, severe or hard-to-treat high blood pressure.
- Unilateral stenosis is more common than bilateral stenosis, with rates between 53% and 80%.
- Ischemic nephropathy might cause 5% to 22% of advanced kidney disease in people over 50.
- 75% to 80% of fibromuscular dysplasia cases affect renal arteries.
- Two-thirds of these cases involve multiple renal arteries.
- Fibromuscular dysplasia is more common in females.
Signs and Symptoms of Renal Artery Stenosis
Renovascular disease could be the cause of high blood pressure if certain signs are present. You might have renovascular disease if you experience:
- Severe high blood pressure that doesn’t respond to treatment with three or more drugs
- High blood pressure at a young age without a family history
- Sudden high blood pressure before age 50, which might be caused by fibromuscular dysplasia, or after age 50, which could be due to atherosclerotic renal artery stenosis
- An acute and sustained rise in serum creatinine of more than 30% after taking angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs)
- A large variation of serum creatinine concentration due to changes in volume status
- Frequent episodes of flash pulmonary edema or heart failure that won’t go away
- One kidney significantly smaller than the other
- Low potassium levels without an obvious cause
- Worsening kidney function after placing an endovascular aortic stent graft
- An ongoing and worsening reduction in the rate of blood filteration through the kidneys
- An increase in blood urea nitrogen (BUN) for no obvious reason
- No evidence to suggest an alternative cause of kidney disease, such as an abnormal urinalysis, protein in the urine, a paraprotein, or use of a kidney-damaging drug
Additional symptoms may include an abnormal noise in the abdomen or flank, severe damage to the retina, or peripheral or coronary vascular disease. Renal artery stenosis (RAS) can make existing high blood pressure worse, which can complicate the management of the condition.
Testing for Renal Artery Stenosis
If your doctor suspects that you have a condition called renovascular disease, they will conduct several tests. These tests normally include checking your blood creatinine levels and collecting your urine over a 24-hour period. These tests are done to gauge how well your kidneys are working and how much protein is present in your urine. People with renovascular disease often have minor to moderate levels of protein in their urine but not in an extremely high nephrotic range. Your doctor may also look for red blood cells or red blood cell casts in your urine — these are typically absent in patients with renovascular disease. If they suspect you might have conditions like systemic lupus erythematosus or vasculitis, they may also order blood tests for these.
Imaging tests can also be used to diagnose renovascular disease, especially when the doctor needs to determine whether the patient’s high blood pressure is due to kidney function issues. Before investigating renal artery stenosis (narrowing of the blood vessels that supply your kidneys with blood), your doctor will first rule out other secondary causes of hypertension like primary kidney disease, primary aldosteronism, or pheochromocytoma.
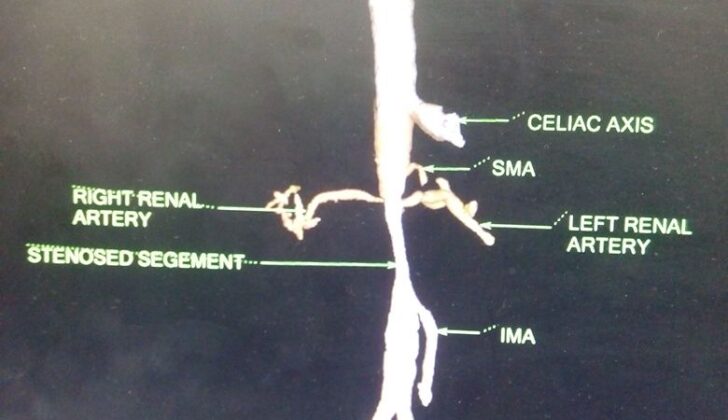
The most accurate way to diagnose renal artery stenosis is renal arteriography, which is basically taking x-ray images of the arteries in your kidneys. However, since this method is rather invasive, other easier tests like duplex Doppler ultrasonography, computed tomographic angiography (CTA), and magnetic resonance angiography (MRA) may be employed based on the situation and availability.
The duplex Doppler ultrasonography method uses high-frequency sound waves to check the blood flow in your renal arteries. Meanwhile, the CTA method uses a combination of X-ray and computer technology to produce detailed images of the blood vessels in your kidneys. MRA makes use of magnetic fields and radio waves to create comprehensive images of the structures in the body. However, the usage of MRA might be limited because of its high costs and the need for specialized knowledge for reading the imaging results.
Another method, Angiotensin-Converting Enzyme (ACE) Inhibitor Scintigraphy, uses a special camera and a tracer to examine how well blood is flowing in the kidneys. Any changes in the kidney function caused by an ACE inhibitor (a type of high blood pressure medication) can be revealed with this method.
Finally, the last method, conventional arteriography, uses a special dye and camera to take pictures of the blood flow in an artery or a vein. Even though this method produces excellent images, it requires a puncture in an artery, carries the risk of thromboembolism (a blood clot that has moved from its original location), and uses a moderate amount of contrast dye.
Treatment Options for Renal Artery Stenosis
If you have renal artery stenosis, which is a narrowing of the arteries that carry blood to your kidneys, initial treatment might involve just monitoring the condition, rather than immediate intervention. This is especially true if the narrowing is between 50-80% and tests show no further issues, or if the narrowing is less than 50%. Around every six months, your doctor may use ultrasound to examine your kidneys, and recommend medication to control your cholesterol and blood pressure, including drugs to prevent blood clots.
Medications commonly used in this situation are angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), which help to lower blood pressure and protect the kidneys. However, these medications can sometimes cause higher levels of a chemical called creatinine in your blood, a sign your kidneys may not be working well, and higher levels of potassium, which can be dangerous. If this is the case, your doctor might switch to another type of blood pressure medication, like a calcium channel blocker. They may also prescribe statins to lower your cholesterol levels.
Your doctor will consider intervention, such as surgery to widen the narrowed artery, if the narrowing goes above 80%. This holds true even if your kidneys are functioning well. If you only have one working kidney or both kidneys have this condition, intervention may be necessary.
If your kidney function is normal or near normal, doctors recommend fixing the blocked artery to prevent kidney issues in the future. This would be the case if the narrowing is above 80-85% or if it’s between 50-80% and a special type of scan, called captopril-enhanced scintigraphy, indicates issues within the kidney itself.
On the other hand, if there are already signs of kidney problems, your doctor might recommend intervention based on several factors. These include: your creatinine level is less than 4 mg/dL; your creatinine is above 4 mg/dL but there is a potential recent blood clot in a kidney artery; the narrowing of the artery is above 80%; your creatinine level increases after taking ACE inhibitors; and if your renal artery has 50-80% narrowing and the scan is positive for the condition.
What else can Renal Artery Stenosis be?
Here are some health conditions related to kidneys and blood pressure:
- Acute kidney injury
- Azotemia
- Chronic Glomerulonephritis
- Hypersensitivity Nephropathy
- Hypertension
- Malignant Hypertension
- Nephrosclerosis
- Renovascular hypertension
- Uremia