What is Tubulointerstitial Nephritis?
Tubulointerstitial nephritis, or interstitial nephritis, is a kidney condition that was first identified in 1898 by a scientist studying the body after a person’s death. They saw unusual signs of inflammation in the kidney tissue when looking at patients who had suffered from a streptococcal infection, which is a type of bacterial infection. This kidney condition involves inflammation within spaces in the kidney and inflammation of the surrounding kidney cells. This inflammation is usually due to white blood cells like macrophages, lymphocytes, plasma cells, with infrequently eosinophils, all types of immune cells. Typically, this disease spares the glomeruli, which are tiny units in the kidney responsible for filtering blood, unless it has been going on for a long time.
Doctors classify this disease into two types – acute or chronic. Classification depends on how quickly it develops, how the kidney looks under the microscope, and what has caused it. Most cases of this disease, about 70% to 75%, occur as a reaction to medication and are known as allergic acute interstitial nephritis. However, this explanation will focus only on cases unrelated to drug reactions, which are 20% to 25% of total cases.
Non-drug-related tubulointerstitial nephritis can arise due to various reasons. It may be because of unknown reasons, inherited from parents, due to the body’s immune response, or because of infections caused by viruses, bacteria, parasites, or fungi. Certain diseases can also cause this type of kidney inflammation. These diseases include inflammatory bowel disease, sarcoidosis, systemic lupus erythematosus (an autoimmune disease), Sjögren’s disease (an immune system disorder), an autoimmune disease related to the immunoglobulin G4 protein, an immune reaction against a component of the kidney cell, and a syndrome featuring both kidney inflammation and eye inflammation.
Detecting this disease can be quite challenging because its signs and symptoms are often not very specific, which can lead to delays in diagnosis. Late diagnosis may have severe impacts on health. While many attempts have been made to establish a faster, more reliable way to detect and diagnose tubulointerstitial nephritis, it continues to be difficult. This explanation provides an overview of the process of diagnosing and managing different forms of tubulointerstitial nephritis.
A genetic form of this disorder, called autosomal dominant tubulointerstitial kidney disease, has been covered separately.
What Causes Tubulointerstitial Nephritis?
Infections
Infections are another main cause of a condition called tubulointerstitial nephritis (TIN), especially in less developed countries. This is a type of kidney inflammation that can result from various sources. Some common types of bacteria that can lead to this are Escherichia coli, Campylobacter, and Salmonella. Viruses like HIV and COVID-19 can also cause it, as well as certain types of fungi and parasites. Usually, patients with TIN due to infections start to experience symptoms related to the specific infection they have, and kidney problems like acute kidney injury (AKI) may not be the first symptom. Doctors will first treat the underlying infection before treating TIN with steroids.
Autoimmune Disease
Some autoimmune diseases, which are when your own immune system mistakenly attacks your body, are known to cause TIN. These include lupus, Sjogren syndrome, sarcoidosis, inflammatory bowel disease, and a recently discovered condition called IgG4-related disease.
Lupus nephritis is a kidney problem caused by lupus. In the past, it was thought to mainly damage tiny structures in the kidney that filter the blood (glomeruli). However, newer research shows that scarring and atrophy (wasting away) in other parts of the kidney may actually be more important in determining how well treatment works and how the disease will progress. Lupus nephritis can affect anywhere between 40 to 80 percent of people who have lupus, depending on whether they are adults or children. Even with the most recent treatment methods, about 10 percent of these patients will develop End Stage Renal Disease (ESRD) and will need help from a machine (renal replacement therapy) to perform the roles of the kidney.
Similarly, Sjogren syndrome is another autoimmune disease that affects the kidneys, although less often. When it does, TIN is usually the most prominent pathology observed. Patients with this disease can experience several symptoms related to kidney problems such as inability to manage pH in the body (distal tubular acidosis), a form of diabetes caused by problems in the kidneys (nephrogenic diabetes insipidus), and more.
Inflammatory bowel disease (IBD), which includes conditions like Crohn’s disease and ulcerative colitis, also often leads to kidney dysfunction.
In addition, there is a condition known as IgG4-related disease which causes the kidneys to malfunction due to an overload of protein which results in cellular injury. This results in inflammation in the region and the disease can be treated effectively with steroids.
Transplant TIN
TIN is remarkably the third most common cause of problems with kidney transplants and usually results from an underlying infection. Some of the more frequent infections that lead to TIN in transplants are bacterial kidney infection (pyelonephritis) and the BK virus. Other viruses can also cause problems, including adenovirus, JC virus, and cytomegalovirus.
Then, there is a condition known as tubulointerstitial nephritis and uveitis syndrome (TINU), which is associated with the Epstein-Barr virus and bacteria like Leptospira, Mycoplasma, and Yersinia. It starts off with kidney failure from TIN and then eventually leads to a type of eye inflammation (uveitis). It is more common in females and mainly affects kids and teenagers under twenty. Uveitis symptoms can include light sensitivity, eye pain, and redness. However, up to half the patients may not experience these eye symptoms. The exact cause of TINU is not yet understood, but it seems to be related to various factors like an autoimmune response, genetic susceptibility, medical treatments, and infections.
Risk Factors and Frequency for Tubulointerstitial Nephritis
Acute AIN, a kidney condition, is found in 1% to 3% of all kidney biopsy cases globally. However, in cases where only AKI, another kidney condition, was diagnosed, the prevalence of acute AIN increased to between 15% and 27%. It’s worth noting that more cases of drug-induced acute AIN are reported in developed countries than in developing countries, where infectious causes are more common. Older people are often more susceptible to drug-induced acute AIN due to their higher medication usage and weaker immune systems.
It’s also interesting to note that different types of diseases have different demographic predominances. For instance, TINU, a specific illness, is primarily found in children and teenagers under the age of 20. In contrast, anti-TBM disease is found across all age groups. Furthermore, women are more likely to experience SLE and Sjogren syndrome, while the prevalence of sarcoidosis is fairly equal between both sexes.
Signs and Symptoms of Tubulointerstitial Nephritis
Tubulointerstitial nephritis (TIN) is a kidney disorder that can sometimes be hard to diagnose and treat due to its varying symptoms. Important factors to consider are the length of time when symptoms started appearing, the age of the patient, and whether they’ve been using any medication. Its classic signs, which are fever, skin rash, and an excessive amount of a type of white blood cells called eosinophils, don’t always occur all at once. Joint pain is also a common but vague symptom.
To better understand the condition, here are some additional variant presentations:
- Autoimmune and infectious diseases tend to show extra symptoms not related to the kidney, depending on the kind of disease itself.
- Initial signs of TIN might present normal or increased urination due to problems with the kidney’s reabsorption process. If TIN remains unnoticed and becomes worse, it could lead to low urine output (oliguria) as the condition progresses.
- Pain on the side of your body, a feeling of fullness in your belly, or fullness extending to your groin could reflect kidney swelling caused by TIN.
- Notices of a kidney disorder called nephrotic syndrome, like facial swelling and swollen feet or legs, may also be observed.
- Eye symptoms are usually associated with TIN in conjunction with uveitis (TINU) in children and teenagers below 20 years old, and with a disorder called Sjogren’s in patients over 20. However, it’s important to note that uveitis might not always present with eye symptoms and an eye exam is necessary to assess it.
Testing for Tubulointerstitial Nephritis
Tubulointerstitial nephritis is a condition related to the kidney that often has vague symptoms which can make its diagnosis delayed or difficult. It is important to correctly identify this condition because it’s different from other similar kidney diseases like glomerulonephritis and acute tubular necrosis. The treatment approach and potential outcomes for these diseases vary greatly. When a patient shows signs of issues with their kidney function, doctors should consider tubulointerstitial nephritis as a possible cause. The diagnosis typically involves a combination of clinical assessment, lab tests, and imaging studies.
A common early sign of tubulointerstitial nephritis is kidney failure, which can be detected through blood tests that measure levels of blood urea nitrogen and creatinine. These may be found as part of routine check-ups in patients who don’t have any symptoms. A crucial clue is when patients show an unexplained increase in the levels of creatinine in their blood. Detecting a BUN/creatinine ratio of 12 or less is highly suggestive of this condition. Doctors also check for levels of substances like complement factors, anti-neutrophilic cytoplasmic autoantibody, immunoglobulin subtypes, and anti-streptolysin O antibody.
Patient may also display issues with their electrolyte and acid-base balance, which can include higher than normal levels of potassium and chloride. A low level of phosphorous and uric acid might indicate a Fanconi-type syndrome, which is another type of tubular injury. Anemia can occur due to decreased erythropoietin production resulting from tubular cell injury. The test for C-reactive protein or erythrocyte sedimentation rate can also suggest the presence of an inflammatory process albeit being nonspecific.
Imaging techniques like ultrasound and CT scans are useful in diagnosing tubulointerstitial nephritis. These tests help eliminate other potential causes of kidney trouble, such as stones, cysts, tumours, blockages, and hydronephrosis. One possible indication of this condition is both kidneys appearing normal or slightly enlarged alongside uniformly increased echogenicity in the renal cortex. Other techniques like gallium scintigraphy and PET scans can also be used but they are generally less sensitive and specific.
Test of the urine under a microscope is a frequently-used tool to investigate kidney disorders. It can provide useful clues to diagnosing tubulointerstitial nephritis. Common findings include protein in the urine (usually less than 1g/day), white blood cells in the urine without evidence of bacterial infection, white blood cell casts, and red blood cells in the urine.
Urinary biomarkers like monocyte chemotactic peptide-1 (MCP-1), alpha1-microglobulin (A1M), matrix metalloproteinase-2 (MMP-2), beta 2-microglobulin (B2M), and CXCL9 could play a critical role in diagnosing and monitoring this condition. Presence of these small proteins in the urine may indicate tubular injury and inflammation in the interstitial tissue of the kidney.
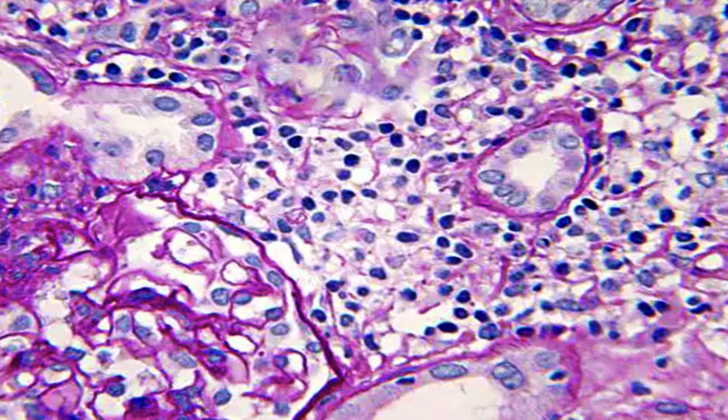
Inspecting kidney tissue under a microscope after a biopsy can provide a definitive diagnosis of tubulointerstitial nephritis. This procedure may be performed if there’s no improvement in the patient’s condition after stopping any potential offending drugs for 5 to 7 days, unless there are contraindications like uncorrected clotting disorders, inability to stop blood thinners due to other health issues, uncooperative patients, end-stage kidney disease with shrunken kidneys, uncontrolled high blood pressure, active infection, severe instability of vital signs, and patient’s refusal. Biopsy may be done on a solitary kidney only in absolutely necessary cases.
Treatment Options for Tubulointerstitial Nephritis
If you have tubulointerstitial nephritis, a kind of kidney disorder, doctors need to check thoroughly to find and deal with things which might be causing it, like certain medicines, and also treat any illnesses that might be related to it. A common treatment has been corticosteroids, a type of medication that reduces inflammation and calms down your immune system. However, research has not shown consistent benefits from this treatment. Still, because the risks associated with corticosteroids are relatively low, many doctors will prescribe a course of this medication if it’s safe for the patient. If the kidney disorder is due to an infection, the doctors will treat the infection before administering corticosteroids.
TINU syndrome, a kind of kidney disorder which also causes eye disease, is usually treated with systemic corticosteroids – the medication mentioned above which calms down your immune system. However, the eye inflammation may also be treated with special eye drops that contain steroids and drugs that relax the eye muscles. If patients can’t tolerate systemic corticosteroids, other drugs that modify the immune system such as methotrexate, azathioprine, and mycophenolate mofetil might be used. ‘Therapeutic plasma exchange’, which is a process to remove harmful substances from your blood, has been suggested as a possible treatment to get rid of harmful antibodies, but we don’t have data to say whether this really helps.
People who have had a kidney transplant and need strong medications to stop their bodies from rejecting the kidney are more likely to get tubulointerstitial nephritis due to viral and bacterial infections. If this happens, doctors manage it by lowering the dosage of immunosuppressants, which are the medications that prevent the body from rejecting the transplanted kidney. Sometimes, an antiviral drug called cidofovir is used to treat the disorder.
What else can Tubulointerstitial Nephritis be?
When doctors assess a patient for TIN, or Tubulointerstitial Nephritis, they look for signs that might be shared with a number of other kidney issues that can result in Acute Kidney Injury (AKI) or decreased kidney function. The following possible health problems could potentially overlap with TIN and need to be ruled out:
- Acute Tubular Necrosis (ATN): The main cause of sudden kidney failure, ATN is marked by damage to the kidney tube cells due to factors like insufficient blood flow, certain harmful substances or drugs, or other dangerous agents. It shares signs with TIN like decreased urine output, harmful acid buildup, increased BUN and creatinine levels, and mineral imbalances.
- Atheroembolism: This happens when cholesterol crystal clots should be considered in patients who are primarily showing white and red blood cell casts in their urine. Atheroemboli can also result in skin rashes, high eosinophil counts in urine and blood. Age, obesity, and history of vascular disease may also point to this condition.
- Glomerulonephritis: Various types of glomerular diseases can lead to kidney impairment and may have characteristics similar to TIN such as protein in the urine and lower urine output. However, the presence of white blood cell casts and misshapen red blood cells might suggest glomerulonephritis rather than TIN.
- Obstructive Uropathy: A blockage in the urinary tract can cause a certain type of kidney failure. This condition is often due to kidney stones, tumors or narrow passages, and may cause no urine output. Imaging can be helpful in distinguishing between uropathy and other possible causes of kidney injury.
- Vascular Injury: Various heart-related issues such as narrowed kidney arteries, heart failure, vasculitis, decreased blood flow due to blood vessel constriction in NSAID users, and decreased vascular tone due to ACE inhibitors can mimic TIN. However, the type of rash in vasculitis is usually different from the rash that might be seen in drug-induced TIN.
What to expect with Tubulointerstitial Nephritis
The outlook for TIN (Tubulointerstitial Nephritis, a type of kidney damage) depends on several factors. These include the cause of the TIN, when treatment begins, initial kidney function, any previous harmful substances, and how long the patient has been exposed to the cause. TIN that becomes chronic, marked by severe scarring (fibrosis) or the loss of tube-like structures in the kidneys (tubular atrophy), can have more serious outcomes. It’s crucial to identify and eliminate the cause early to improve kidney health.
Infections that cause TIN are often temporary and respond well to drugs that kill or delay the growth of microorganisms (antimicrobial treatment). TIN caused by an autoimmune disease (where the immune system attacks the body’s own cells) tends to recur depending on the activity of the original disease. Hence, it’s essential to continuously monitor kidney function.
A specific kind of TIN, known as TINU, especially requires careful and ongoing check-ups with an eye doctor (ophthalmology) due to its tendency to come back and the younger age of patients it affects. Patients who’ve undergone a kidney transplant and develop TIN because of a virus should have close supervision of their immunosuppressant therapy and viral levels. This is because each TIN occurrence could potentially harm the function of the transplanted kidney (allograft) and trigger a rejection episode.
Possible Complications When Diagnosed with Tubulointerstitial Nephritis
Elderly individuals may be more susceptible to health complications. Kidney insufficiency is a common problem that can worsen over time into End Stage Renal Disease. This is caused by the hardening of the spaces between cells in your kidneys and the breakdown of kidney cells responsible for filtering out waste from your blood. Another potential issue is inflammation or infection in cells of the kidney that can interfere with the production of a hormone called erythropoietin. This hormone is necessary for the production of red blood cells, and its lack can lead to complications such as anemia.
Another issue with TIN (Tubulointerstitial nephritis) is the overactivity of a hormone called angiotensin II. This hormone manages your blood pressure but, when overactive, can lead to high blood pressure. This is due to the increased retention of sodium and fluid in your body, constriction of your blood vessels, and enhanced oxidative stress. Too much angiotensin can, therefore, disrupt your blood pressure and oxidative stress, causing tightening of your blood vessels.
Potential Health Complications:
- Kidney insufficiency
- End Stage Renal Disease due to hardening of kidney cell spaces
- Inflammation or infection in kidney cells
- Reduced production of red blood cells
- Anemia
- Overactivity of angiotensin II
- High blood pressure
- Sodium and fluid retention
- Vasoconstriction
Preventing Tubulointerstitial Nephritis
It’s important to help patients understand what causes Tubulointerstitial Nephritis (TIN), a kidney condition, and how to prevent it from coming back in the future. All the tests conducted to diagnose the condition and the results of these tests should be fully discussed with the patient. Likewise, the different treatment options, including their potential risks and benefits, should be explained. This information about their condition and treatment plan is crucial for the patient’s understanding and should be presented in a way that is easy for them to comprehend.