What is Chronic Obstructive Pulmonary Disease (COPD)?
Chronic obstructive pulmonary disease (COPD) is a common disease that can be treated. It involves a gradual slowing down of the airflow in your lungs and damage to the lung tissue. This is mainly caused by continuous inflammation in the lungs due to prolonged exposure to harmful substances, cigarette smoke being the most common. This chronic inflammation can lead to the narrowing of the airways and a reduction in the elasticity of the lungs.
Usually, COPD causes symptoms like coughing, breathlessness, and the production of mucus. However, the intensity of symptoms can vary significantly: some people may not experience any symptoms while others might suffer from respiratory failure.
What Causes Chronic Obstructive Pulmonary Disease (COPD)?
COPD, or chronic obstructive pulmonary disease, happens when you’re exposed to damaging particles or gases for a long time. The most common cause of COPD around the world is cigarette smoking. Other factors that can cause COPD are being exposed to second-hand smoke, environmental and workplace hazards, and a condition called alpha-1 antitrypsin deficiency (AATD).
Risk Factors and Frequency for Chronic Obstructive Pulmonary Disease (COPD)
COPD, short for chronic obstructive pulmonary disease, is typically found in smokers and people over 40 years old. As people age, the chance of having COPD increases, making it the third most common cause of illness and death across the globe. In the year 2015, around 174 million people had COPD, and roughly 3.2 million died from it. However, these numbers might be lower than the actual figures, as COPD often goes undiagnosed.
- COPD usually affects smokers and people over 40.
- The likelihood of getting COPD increases with age.
- It’s the third leading cause of illness and death worldwide.
- In 2015, there were around 174 million people with COPD.
- Approximately 3.2 million people died from COPD that year.
- The actual prevalence may be higher, as COPD often goes undiagnosed.
Signs and Symptoms of Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) usually begins in adulthood and often shows up during the colder months. People with this condition often complain about ongoing and worsening shortness of breath, persistent cough, and producing mucus. Other symptoms include wheezing and a feeling of tightness in the chest. Although many people with COPD are smokers, not all of them have a history of smoking. Questions about exposure to secondhand smoke, work-related and environmental factors, and family medical history can help with diagnosis.
Once a diagnosis of COPD is confirmed, it’s important to look back at the person’s health history. This includes incidents of worsening symptoms, being woken up during the night by their condition, use of inhalers, and the impact of the disease on daily activities. Other past medical conditions like asthma, allergies, or childhood respiratory infections should be considered. If a patient has liver disease, basilar emphysema, or a family history of emphysema, it could mean they have a deficiency in alpha-1 antitrypsin, a protective enzyme in the lungs. Intense episodes of COPD symptoms, often called acute exacerbations, usually include increased shortness of breath, cough, and wheezing.
Those with COPD may show various physical symptoms, such as:
- General symptoms: severe breathing difficulties during acute exacerbations and muscle loss
- Lung-related symptoms: use of extra muscle strength for breathing, extended periods of exhaling breath, wheezing, and breathing through pursed lips
- Chest-related symptoms: an increase in the size of the chest from front to back (known as barrel chest)
- Skin-related symptoms: a bluish color in the face due to insufficient oxygen in the blood
- Extremity-related symptoms: finger clubbing (thickening of the fingertips) and swelling in the lower limbs due to right-sided heart failure
Testing for Chronic Obstructive Pulmonary Disease (COPD)
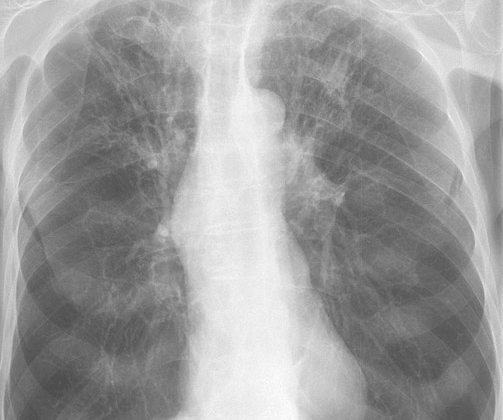
Chronic Obstructive Pulmonary Disease (COPD) is often checked for in patients having symptoms or risk factors associated with the disease. The diagnosis is typically confirmed with a breathing test called spirometry. The patient may also undergo a 6-minute walk test, laboratory tests and imaging procedures, like a chest X-ray or a computing tomography (CT) scan.
Pulmonary function testing (PFT), including spirometry, is crucial in diagnosing COPD. Spirometry is done before and after inhaling a bronchodilator – a medication that helps open the airways. If the result of the spirometry indicates that the amount of air expelled in one second relative to the total air capacity of the lungs (the FEV1/FVC ratio) is less than 0.7, it supports the diagnosis of COPD.
A well-known global initiative on COPD, called GOLD (Global Initiative for Chronic Obstructive Lung Disease), offers detailed reports and guidance on how to diagnose and manage the disease. The severity of a patient’s COPD can be determined using tools like the GOLD ABCD assessment.
The patient’s degree of breathlessness can be assessed using the mMRC (modified British Medical Research Council) questionnaire, while the COPD Assessment Test (CAT) evaluates how much the disease impacts a patient’s daily life.
A 6-minute walk test can measure a patient’s functional capacity as it records how much distance a patient can cover over a period of 6 minutes. Laboratory tests typically include a complete blood count to check for possible infection, anemia, and other potential complications. It might also be needed to test for alpha-1 antitrypsin levels – a protein that protects the lungs.
Chest X-rays or CT scans provide images of the lungs and may show signs such as lung over-inflation, flat diaphragm or increasing chest size. In some patients, CT scans can be helpful if additional issues like bronchiectasis or cancer are suspected, or if a surgical procedure is being considered.
A tissue biopsy is not routinely required for diagnosing COPD. In the case of sudden worsening of respiratory symptoms (known as an acute exacerbation of COPD), doctors may use a specific model to assess its severity, based on the presence of worsening breathlessness, increased sputum production, and purulence (pus). Other factors, such as an increased heart rate, fever, or upper respiratory infection, may also be indicative of a mild exacerbation. More intense symptoms could suggest moderate or severe exacerbations.
Treatment Options for Chronic Obstructive Pulmonary Disease (COPD)
The main goal of treating chronic obstructive pulmonary disease (COPD) is to lessen symptoms, enhance life quality, decrease instances of the disease getting worse, and lower the risk of death. Non-drug treatments include quitting smoking and undertaking a program to improve lung function.
Getting the flu vaccine every year is vital for all COPD patients. Those 65 and older should receive two different types of pneumonia vaccines at least one year apart. And people with comorbidities (like diabetes or heart disease) should also get pneumonia vaccination.
Several kinds of medications are used to manage COPD. These include bronchodilators which relax the airway muscles, inhaled steroids which reduce inflammation, systemic glucocorticoids, phosphodiesterase-4 (a type of inflammation reducer), and antibiotics.
Beta2-agonists are a type of bronchodilator. There are short-acting beta2-agonists, known as SABAs, used to provide immediate relief and long-acting ones, known as LABAs, used for ongoing care.
Antimuscarinics are used to prevent airway tightening. Like with beta2-agonists, there are short-acting antimuscarinics for immediate relief and long-acting ones for ongoing care.
Another bronchodilator, methylxanthines, is typically used as additional treatment after LABA or LAMA. The mechanism of action is not clear, but it may involve inhibition of certain enzymes. A common type of this medication is Theophylline, which can be used with Salmeterol to provide better improvement in lung function.
Inhaled steroids are often used in conjunction with LABAs and LAMAs to decrease inflammation. However, they come with a risk of developing pneumonia. Oral glucocorticoids, another type of steroid, should only be used for short-term relief during severe COPD flare-ups due to their potential side effects.
The Phosphodiesterase-4 inhibitors reduce inflammation and are used in patients with severe COPD to decrease the number of flare-ups. Roflumilast is an example of such a medication.
Studies have shown Azithromycin, an antibiotic, may decrease COPD flare-ups. However, doctors should be cautious, as overuse could lead to antibiotic resistance, and patients must be monitored for potential issues like prolonged heart rhythms and hearing loss.
The treatment of sudden COPD flare-ups can be managed at home or in the hospital, based on the severity of symptoms. Mild cases can be treated at home with bronchodilators, steroids, and antibiotics. However, more severe cases may require hospitalization and oxygen therapy. Hospitalized patients usually need bronchodilator therapy and may require oxygen ranging from a nasal cannula to full mechanical ventilation, depending on the severity of the disease.
Long-term treatment should be personalized to each patient and generally depends on the severity of the disease and symptoms. In serious cases, surgical options may be considered, like removing sections of the damaged lung or even lung transplantation.
Pulmonary rehabilitation, a tailored plan involving exercises and education, is recommended for all stages of COPD. The aim is to improve a patient’s physical and psychological wellbeing.
What else can Chronic Obstructive Pulmonary Disease (COPD) be?
Doctors must take into account a variety of different health conditions when diagnosing a patient with breathing problems. Here are some of the conditions they might consider:
- Asthma
- Asthma-COPD overlap syndrome (a condition where features of both asthma and COPD are present)
- Interstitial lung disease (diseases that cause scarring of the lung tissue)
- Bronchiolitis obliterans (a serious lung disease that affects the small airways)
- Diffuse panbronchiolitis (a progressive inflammatory lung disease)
- Heart failure
- Thromboembolic disease (a condition where a blood clot blocks a blood vessel)
- Lymphangioleiomyomatosis (a rare lung disease that usually affects women)
- Tuberculosis (an infectious disease that primarily affects the lungs)
- Cystic fibrosis (a genetic disorder that damages the lungs and digestive system)
- Bronchiectasis (a condition in which the bronchi in the lungs are permanently enlarged)
- Malignancy (cancer)
It’s essential for doctors to thoroughly consider all these possibilities and perform necessary tests to ensure an accurate diagnosis.
What to expect with Chronic Obstructive Pulmonary Disease (COPD)
The outlook for chronic obstructive pulmonary disease (COPD) can vary largely depending on how well the patients stick to their treatment plan. This includes quitting smoking and staying away from harmful gases. Those who also have other health conditions, like high blood pressure in the lungs, heart disease, or lung cancer, usually have a less favorable outlook. The limitations in airflow and shortness of breath that accompany COPD are often progressive, becoming worse over time.
Doctors may use what’s known as the BODE index to predict the risk of dying from COPD. BODE stands for Body-mass index (BMI), airflow Obstruction, Dyspnea (or breathlessness), and Exercise capacity. It factors in your lung function, how far you can walk in 6 minutes, your level of breathlessness, and your BMI. The score ranges from 1-10 and can give doctors a good idea about the 4-year survival rate for a COPD patient.
Possible Complications When Diagnosed with Chronic Obstructive Pulmonary Disease (COPD)
Here are some common complications that can occur with COPD (Chronic Obstructive Pulmonary Disease):
- Sudden worsening of COPD symptoms
- Respiratory failure, which can be either short-term or long-term
- Increased blood pressure in the arteries to the lungs, which is referred to as pulmonary hypertension
- Cor pulmonale, a condition where the right side of the heart enlarges and fails due to chronic lung disease
- Loss of weight
- Bacterial infections
- Negative side effects from the use of a type of medication called glucocorticoids
Preventing Chronic Obstructive Pulmonary Disease (COPD)
In order to slow down or prevent the intensification of COPD (Chronic Obstructive Pulmonary Disease), it’s important to educate patients about several crucial lifestyle changes. Here are some key points to bear in mind:
- Quit smoking: This is a significant step in preventing further damage to the lungs.
- Avoid exposure to second-hand smoke: It’s as harmful as firsthand smoking.
- Limit exposure to harmful substances: Especially at work or in the environment. This can include inorganic substances like asbestos, beryllium, carbon dust, silica, chromium, and organic substances such as certain types of fungi, bird droppings, and specific bacterial species.
- Avoid the use of unvented coal stoves: These can release harmful particles into the air.
- Learn how to use your inhaler properly: Good technique is key for medication to be effective.
- Understand the importance of using your inhaler: Reliability in medication use is crucial to managing COPD.
- Keep up with follow-up appointments: This helps your healthcare providers track your progress and adjust treatment as necessary.
- Stick to the treatment plan: This could involve medication, pulmonary rehabilitation, and lifestyle changes.
- Stay alert for worsening symptoms and seek medical attention as needed: Early detection allows for timely intervention.
- Participate in pulmonary rehabilitation: This is a program intended to improve lung function and overall quality of life for COPD patients.
By adopting these practices, risk and progression of COPD can be significantly reduced, and patients can lead a healthier life.