What is Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)?
Chronic thromboembolic pulmonary hypertension (CTEPH) is a potentially severe health condition that can significantly reduce quality of life and potentially lead to death. But the good news is that improvements in medical treatment and surgeries have greatly improved patient outcomes. CTEPH is a specific type of pulmonary hypertension related to chronic blood clot disease and falls under a specific classification of lung hypertension by the World Health Organization.
Acute pulmonary embolism, which is a sudden blockage in the lung arteries usually caused by blood clots, can develop into chronic blood clot disease over time, leading to CTEPH. This can be especially true if additional risk factors are present, such as genetic tendencies towards blood clotting, recurring clotting events, genetic predisposition, and conditions like other illnesses. If it’s not treated in its advanced stages, CTEPH can lead to intense heart failure. Therefore, it’s important to monitor individuals who are at risk closely. If left untreated, CTEPH can lead to serious restriction in normal activity and ultimately premature death due to blood flow issues.
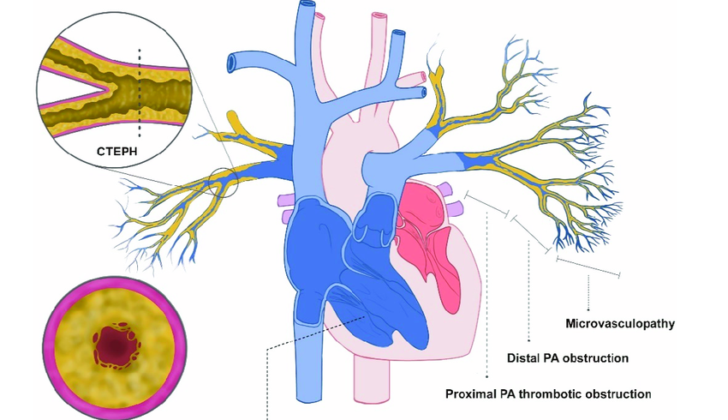
Understanding the physical structure of how CTEPH affects the body gives us insight into how blood clot blockages can influence blood flow in the lungs, gas exchange, and heart function. Blood circulation between the heart and lungs for oxygenation is known as pulmonary circulation. This process starts on the right side of the heart. The right ventricle sends oxygen-depleted blood into the lung arteries. These arteries then divide into smaller vessels, reaching the tiny lung capillaries.
In these tiny capillaries, gas exchange happens. Carbon dioxide leaves the blood to be breathed out, while inhaled oxygen enters the bloodstream to go back to the heart. Once filled with oxygen, the blood goes toward the left side of the heart via the lung veins.
Normally, the pulmonary circulation is a low-pressure system. The right ventricle only needs to pump blood a short distance into the flexible blood vessels of the lungs and back, which is efficient for gas exchange. This makes sure the blood is well-oxygenated before it circulates around the body. Besides, the lung blood vessels can quickly respond to changes in oxygen levels, allowing them to adjust blood flow to meet the body’s needs.
What Causes Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)?
Chronic Thromboembolic Pulmonary Hypertension (CTEPH) is a medical condition that is believed to form in a way similar to deep vein thrombosis and acute pulmonary embolism.
In these situations, clotlike substances travel into the lungs’ blood vessels, causing changes in the blood vessels and leading to high blood pressure in the lungs.
Some studies suggest that people with higher levels of certain substances in their blood, related to blood clotting, are more likely to develop CTEPH.
Several risk factors make a person more likely to develop CTEPH. These include:
- A history of lung blood clots, which increases the chances 19 times.
- Being younger increases the chances 1.79 times per decade.
- A large blood flow defect, which increases the chances 2.22 times per specific drop in lung scan results.
Almost 90% of people who have CTEPH have experienced acute pulmonary embolism, and close to half have reported recurrent pulmonary embolism.
Normally, the body can break down and get rid of these clots by itself, restoring normal blood flow. However, why this doesn’t always happen in some cases is unclear. Some theories suggest that it’s more difficult to break down large clots completely or that certain kinds of clots are more resistant to this process.
Other risk factors for CTEPH include:
- Repeat clotting events
- Certain genetic clotting disorders
- Immune diseases
- Specific heart surgeries or implants
- Cancer
- Inflammatory bowel diseases
- Spleen removal
- Chronic bone infections
- Heart dysfunction
- Diabetes
- Underactive thyroid
- Younger age
- Acute lung blood clots with a greater blood flow defect
- Unexplained lung blood clots
Determining whether a patient already had undiagnosed lung high blood pressure or if CTEPH was mistaken as acute pulmonary embolism can be challenging.
Risk Factors and Frequency for Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)
Studies exploring the reach and patterns of a condition called CTEPH are few. Yet, they estimate its occurrence at about 2% to 6% of the population, or roughly 26 to 38 cases per million people. After a person has a lung clot or pulmonary embolism, it’s estimated that about 1% will develop CTEPH within 6 months and around 3% within a year. It’s rare that CTEPH develops 2 years post-clot.
In America, those diagnosed with lung clots ranges in the development of CTEPH from 0.1% to 9.1%. Metastudy shows that less than 1% of this population will develop CTEPH. Often, CTEPH is under-diagnosed due to lack of awareness among healthcare providers and the so-called “honeymoon period” – the time between lung clot and the appearance of CTEPH symptoms.
- Recently, medical bodies in Europe introduced a new condition – “chronic thromboembolic pulmonary disease” (CTEPD) – that presents with or without lung hypertension.,
- CTEPD shows similar symptoms, blood circulation issues, and lung vessel blockages like CTEPH,
- It’s estimated that around 20% of those suspected with CTEPH indeed have CTEPD,
- Generally, these people are younger than CTEPH patients and have better functional status based on the 6-minute walk test.
Signs and Symptoms of Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)
CTEPH, or Chronic Thromboembolic Pulmonary Hypertension, can cause a variety of symptoms. Initially these may be mild and include shortness of breath, chest pain, dizziness, fainting spells, and fatigue. Without treatment, these symptoms can worsen. Some people might experience a decline in their ability to exercise, coughing, spitting up blood occasionally, atypical chest pain, or heart palpitations. However, these symptoms are less common.
In the early stages of CTEPH, a physical examination might not show clear signs of the disease. In many cases, CTEPH is only confirmed in its advanced stages. At that point, symptoms and indications of right ventricular dysfunction, which refers to problems with the right side of your heart, have started to appear. Examples of these symptoms include swelling in the arms and legs, chest pain during exercise, shortness of breath during exercise, dizziness, or fainting spells.
A doctor may use a stethoscope to listen to your heart and detect certain sounds that indicate CTEPH. These sounds include an intensified second heart sound, a specific kind of heart murmur known as an S4 gallop, and a clicking noise that suggests the blood isn’t flowing correctly through the pulmonary artery, which carries blood from your heart to your lungs. In CTEPH cases, a particular sound – subtle, high-pitched noises that sound like blowing, becoming louder when you breathe in and usually heard while holding breath – can be heard over the lungs. This sign indicates that the medium-to-large pulmonary arteries, which carry blood from the heart to the lungs, are blocked.
If the disease continues to progress, the resulting high blood pressure in the lungs (pulmonary hypertension) can lead to the appearance of additional symptoms. These include a specific heart murmur caused by blood flowing backwards in the heart (tricuspid regurgitation), swelling in the feet, distended neck veins, an enlarged liver, an abnormal buildup of fluid in the abdomen (ascites), and other signs of right heart failure. Many CTEPH patients have low oxygen levels (hypoxemia) due to mismatches in ventilation-perfusion, meaning there’s an imbalance between the amount of oxygen getting to the lungs and the blood flow in the lungs’ vessels. The severity of this oxygen deficiency is linked to the resistance in the lungs’ blood vessels, the pressure in the mean pulmonary artery (a vital blood vessel that carries blood from the heart to the lungs), and the extent of vascular obstruction.
Testing for Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)
For patients with new or persistent symptoms like difficulty breathing or inability to tolerate exercise, diagnostic tests are essential. These symptoms might signify Chronic Thromboembolic Pulmonary Hypertension, or CTEPH, which is tricky to diagnose early because the initial symptoms can be quite general.
Typically, a person experiencing these symptoms would first get a chest x-ray. In the early stages of CTEPH, this might look perfectly normal. Later on, however, the x-ray is likely to show signs of heart and lung problems, like enlarged heart chambers and scarring in the lung tissue.
If the doctor suspects CTEPH, based on factors like past blood clots, abnormal noises detected through a stethoscope, or findings from a chest CT scan, they can confirm this with a suite of additional tests. This can include lung function tests, an echocardiogram (a type of ultrasound), and a special kind of scan called a ventilation/perfusion scan, or V/Q scan.
An echocardiogram can detect high blood pressure in the lungs but can’t tell whether it’s due to a new or old blood clot. On the other hand, a V/Q scan is a powerful tool for diagnosing CTEPH, boasting high accuracy rates. A normal V/Q scan can reliably rule out chronic blood clots in the lungs, but it may underestimate how much lung function is affected if the blood clot is in a central location or if there are other mismatch causes.
To confirm a CTEPH diagnosis, several specific conditions must be met related to blood pressure and resistance in the lungs. Notably, despite its usefulness, a clean CT scan isn’t enough to rule out CTEPH. Therefore, a procedure called right heart catheterization with conventional pulmonary angiography is considered the gold standard for diagnosing CTEPH.
Emerging techniques such as dual-energy CT, dynamic contrast-enhanced MRI, and optical coherence tomography provide valuable insight for evaluating patients with suspected CTEPH. Also, digital subtraction methods for pulmonary angiography are considered the best for confirming CTEPH and figuring out if surgery is an option. Ultimately, combining different diagnostic tools can help accurately diagnose CTEPH, rule out other conditions, plan treatments, and monitor how well a patient is responding to those treatments.
Treatment Options for Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)
Patients who may have CTEPH (chronic thromboembolic pulmonary hypertension) need to be cared for in a specialized medical center by experts in the field. These patients should be given a blood thinner for around three months. During this time, symptoms might improve or disappear, helping medical professionals confirm a patient has CTEPH and start proper treatment.
A surgery called pulmonary endarterectomy (PEA) can sometimes be used to treat CTEPH by removing blood clots from the lungs and improving blood flow and oxygen levels. The University of California-San Diego has created a system that categorizes CTEPH. This helps surgeons understand the complexity of the case and decide the most appropriate treatment.
After PEA, patients will usually need to take blood thinners for the rest of their lives to prevent the formation of new blood clots. Besides, the surgery often improves heart function and quality of life for patients.
However, more than 30% of patients are unfit for surgery. As an alternative, they may undergo a less invasive procedure called balloon pulmonary angioplasty (BPA) which can help improve symptoms and the patients’ ability to exercise.
Every medical procedure comes with risks, and BPA is no exception. Potential complications include injury to the blood vessels, bleeding in the lungs, and fluid buildup in the lungs.
Patients could also be treated using medications such as blood thinners, diuretics (water pills), and oxygen therapy. A drug called riociguat can be beneficial for patients who can’t undergo PEA or who still have high blood pressure in the lungs even after surgery. A lung transplant is considered only as a final option when other treatments are not appropriate or have not worked.
For life-long prevention of blood clots, patients with CTEPH are prescribed anticoagulants like dabigatran, rivaroxaban, apixaban, or edoxaban, which prevent the blood from clotting. Furthermore, medications that target pulmonary arterial hypertension (PAH) may be used to manage CTEPH. These medications include endothelin-receptor antagonists, phosphodiesterase type-5 inhibitors, and prostanoids such as treprostinil and macitentan.
What else can Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots) be?
Chronic thromboembolic pulmonary hypertension (CTEPH) is a condition that can be cured with proper treatment. However, health practitioners need to differentiate it from other conditions that cause similar changes to the arteries in the lungs. These include, but are not limited to, idiopathic pulmonary artery hypertension (IPAH),
- Primary pulmonary arterial sarcoma
- Acute pulmonary thromboembolism that leads to right heart failure
- Thrombosis in situ
- Takayasu arteritis
- Congenital abnormalities in the proximal pulmonary artery
- Tumors in the pulmonary artery, which can be either cancerous or non-cancerous
- Von Recklinghausen and Osler-Weber-Randu diseases
- Arteritis
- Congenital pulmonary artery narrowing
- Fibrosing mediastinitis
A non-invasive test using Doppler ultrasound can help tell CTEPH apart from IPAH. Moreover, conditions like primary pulmonary arterial sarcoma can show up as a solid mass in the arteries on a CT or MRI scan, which does not respond to blood-thinning medication. Additionally, a PET scan using a special dye called F-fludeoxyglucose can help to distinguish between this sarcoma and CTEPH. Lastly, acute pulmonary thromboembolism, a condition that can look like CTEPH, is less likely to be marked by thickening of the right ventricle of the heart, which is often seen in CTEPH.
What to expect with Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)
PEA, or Pulmonary Endarterectomy, can significantly improve the survival rates of patients who are good candidates for the procedure. Research from 2017 showed that the five-year survival rate following PEA is between 70% to 80%. Not only does this operation improve a patient’s chances of survival, but it also significantly enhances the severity of their pulmonary arterial pressure.
One of the key factors influencing the risk of death during hospitalization is the length of time between the last pulmonary embolism episode and undergoing PEA. This highlights the importance of diagnosing Chronic Thromboembolic Pulmonary Hypertension (CTEPH) promptly for the best possible outcome. Currently, the long-term prognosis for CTEPH after having the blood clot surgically removed is extremely positive.
Possible Complications When Diagnosed with Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)
CTEPH, or Chronic Thromboembolic Pulmonary Hypertension, is a serious health issue. It occurs as a result of prolonged thromboembolism, which is a blood clot that blocks blood vessels. If CTEPH is not treated promptly, it can result in serious heart problems, specifically with the right side of the heart. Other symptoms can include severe shortness of breath and reduced physical fitness. Some patients might also faint (a condition known as “syncope”). The most severe consequence is death. In fact, studies have shown that if left untreated, CTEPH can have a 90% mortality rate within three years.
Preventing Chronic Thromboembolic Pulmonary Hypertension (High Blood Pressure in the Arteries of the Lungs due to Scarring from Blood Clots)
Taking steps to prevent an acute pulmonary embolism, which is a sudden blockage in your lung’s blood vessels, can also prevent CTEPH, a form of high blood pressure in your lungs. For people who are hospitalized for a long time, appropriate blood-thinning medications should be given to prevent clots. Other measures like inflatable devices or compression socks can prevent blood clots from forming. Frequent travelers or those having long flights should make sure to get up and walk around every hour or two or adjust their seating positions regularly.
For those diagnosed with CTEPH, it’s important to understand their medication regimen and to have consistent check-ups after leaving the hospital. Regular check-ups are especially crucial if the patient has other health conditions, because managing these together can significantly improve their function and quality of life. If air travel is necessary, these patients should be assessed for potential in-flight oxygen needs.