What is Hemothorax?
Hemothorax is a common condition that happens when there is a significant injury to the chest, causing blood to collect in the space between the two layers of tissue that line the lungs. This can happen due to a blunt or sharp injury that causes bleeding from different parts of the chest, including the wall of the chest, blood vessels, heart muscle, lung tissue, or even the abdomen.
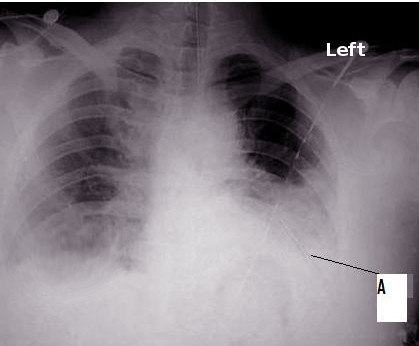
A CT scan, which is basically a detailed X-Ray, is usually the best way to identify injuries in the chest. However, it may not be possible to perform a CT scan in cases where the patient’s condition is critical. Also, not all hospitals may have the facility for a CT scan. In such situations, a chest X-Ray is traditionally used as an initial method to look for serious injuries.
However, recent studies show that a type of ultrasound, known as a point-of-care ultrasound (POCUS), may also be helpful. POCUS is quick, dependable, repeatable, and can be conducted right by the patient’s bedside. This makes it a great tool for quickly identifying life-threatening injuries. Since the mid-2000s, POCUS has been included in a protocol known as eFAST to check for fluid above the diaphragm.
Many studies have shown that using an ultrasound to examine the chest can be a valuable approach when dealing with patients who have experienced blunt chest trauma. Specifically, for hemothorax, studies have shown that lung ultrasound is not only accurate, but often more sensitive than a chest X-Ray.
What Causes Hemothorax?
Hemothorax is often a result of a traumatic injury (like blunt force or penetrating wounds) to the chest area. Most hemothorax cases are due to blunt injuries and carry an overall death rate of 9.4%. Causes that are not due to trauma are less common. These could include, for instance, medical procedures gone wrong, abnormal growths in the lungs, issues with the blood vessels, tumours, blood clotting disorders, and infections.
Risk Factors and Frequency for Hemothorax
Traumatic injuries, including chest injuries, are a significant health issue in the United States, causing around 140,000 deaths every year. Chest injuries are particularly common in severe trauma cases, making up about 60% of them and leading to about 20 to 25% of trauma-related deaths. Notably, these types of injuries are the main reason for deaths in people in their 40s.
The main cause of chest injuries in the US is car accidents, which account for 70 to 80% of these cases. An injury to the chest region can happen due to a direct hit or quick deceleration forces, such as sudden braking in a car accident.
Recent studies have found that chest bone fractures, lung bruising, and diaphragm injuries often occur in blunt chest traumas. Out of those with severe chest injuries, thirty to fifty percent also had a lung contusion, a punctured lung, or a buildup of blood in the chest cavity. In a study looking at traumatic rib fractures, these kinds of conditions were found in 72.3% of cases.
Signs and Symptoms of Hemothorax
Gathering a thorough and accurate history of a patient – either directly from them, from witnesses or from pre-hospital healthcare providers – is important for identifying signs of possible internal chest injuries. Key details to establish include whether the patient is experiencing chest pain or difficulty in breathing, the nature of the injury (such as a fall, the direction, and speed), any use of drugs or alcohol, existing health problems, surgical history, and any anticoagulant or antiplatelet treatments they are on. Factors that might suggest a serious chest injury include car accidents involving speeds greater than 35 mph, falls from over 15 feet, being thrown more than 10 feet as a pedestrian, and trauma resulting in loss of consciousness.
Hemothorax, a type of chest injury that may overlap with signs of pneumothorax, can have a range of different symptoms. These include shortness of breath, fast breathing, decreased or absent breathing sounds, dullness when the chest is tapped, unevenness in the chest wall, movement of the windpipe, low oxygen levels, narrow difference between systolic and diastolic blood pressure measurements, and low blood pressure. Look out for signs of bruising, scrapes, “seat belt sign”, penetrating injuries, abnormal movement (“flail chest”), bruising, deformities, crackling under the skin, and tenderness. Swollen neck veins may indicate pneumothorax or pericardial tamponade but could also be absent in cases of low blood volume. Low blood oxygen levels, increased breathing rate, excessive effort during breathing and use of additional muscles for breathing may all be signs of impending breathing problems.
The physical findings below should prompt the medical professional to consider the associated conditions:
- Swollen neck veins → pericardial tamponade, tension pneumothorax, heart failure, air embolism
- “Seat belt sign” → deceleration or vascular injury; chest wall bruising/scraping
- Abnormal chest wall movement → flail chest
- Facial/neck swelling or blue coloration → upper chest injury with blockage or squeezing of superior vena cava (SVC)
- Subcutaneous emphysema → torn windpipe or lung tissue laceration
- Flat stomach → diaphragmatic injury with herniation of stomach content into the chest
- Excessive stomach movement with breathing → chest wall injury
Testing for Hemothorax
If you’ve experienced a chest injury, it’s crucial to get evaluated and treated as soon as possible. Doctors use a standardized approach called the American Traumatic Life Support (ATLS) protocol, set up by the American College of Surgeons, for this very reason. During the evaluation, priority will be given to assessing your heart and lung function. Injuries to other chest structures like ribs, collarbone, windpipe, main airways, food pipe, and blood vessels will also be taken into consideration.
Imaging is an important part of managing traumatic injuries. A method called Focused Assessment with Sonography in Trauma (FAST) can be used for quick and accurate evaluation of your condition. This method uses ultrasound to look for signs of abnormal fluid or air in different parts of your body like around your heart, liver, spleen, and pelvis. Increasing evidence supports the use of FAST to diagnose instances of blood in the chest (hemothorax), air in the chest cavity (pneumothorax), and bruised lungs (lung contusion).
The use of point-of-care ultrasound in trauma situations has greatly improved the way trauma patients are evaluated and treated. This imaging technique is portable, non-invasive, can be easily reproduced, doesn’t involve radiation or contrast agents, and can therefore be done right at the patient’s side.
FAST can be further expanded to include viewing fluid around your lungs (hemothorax) and air in your chest cavity (pneumothorax). To do this, an ultrasound device is placed on your side around the area of your fifth or sixth rib, with a marker pointed towards your head. If there’s fluid or air in your chest cavity, it can be visualized on the ultrasound machine.
Traditionally, a chest X-ray has been the go-to for initial diagnosis of chest injuries. However, studies show that ultrasound is superior in detecting chest injuries like air or blood in the chest cavity. In fact, when compared to chest X-ray, ultrasound has a higher sensitivity (67% vs 54%); meaning it’s more likely to identify these issues. It’s noteworthy that ultrasound can detect as little as 20 ml of fluid in the chest cavity, compared to 175 ml detected with X-ray.
Moreover, ultrasound can also measure the volume of fluid buildup. Different formulas have been developed for volume prediction. Some involve patient lying flat while others require the patient to sit up.
Finally, other tests recommended for diagnosing blood in the chest include a complete blood count (to get a baseline hemoglobin level), a metabolic panel (to evaluate kidney function), a test for a protein called troponin involved in muscle contractions in the heart, a coagulation profile, and a blood type test. In cases of injury, high levels of lactate (a substance produced when your body breaks down carbohydrates for energy) in your blood can indicate a higher risk of death. If you’ve had a blunt chest injury, you might need multiple troponin tests along with an EKG to evaluate a bruised heart.
Treatment Options for Hemothorax
If a person is brought into a hospital with serious injuries, there are standard procedures to address any life-threatening situations. This involves setting up monitors for the patient’s heart and oxygen levels, and placing two large IV lines for fluid and medication administration. If the patient has a severe air and/or blood collection within the chest (pneumothorax or hemothorax), they may need an emergency intervention such as a needle or tube inserted into the chest to relieve pressure.
However, if the amount of blood collected in the chest cavity is less than 300 ml, it usually doesn’t need to be treated immediately and can naturally resolve over a few weeks. If the patient is stable and not experiencing significant breathing difficulties, they probably won’t require surgical intervention and can be managed with painkillers, while their condition is monitored via repeat imaging.
When it comes to draining blood from the chest (hemothorax), it’s a procedure that should be performed by a cardiothoracic or trauma surgeon, if possible. The tube for drainage is typically placed in the chest region, aiming towards a location that benefits from the help of gravity. The drainage tube is then attached to a system that facilitates rapid drainage and prevents air from entering back into the chest. This setup can also help to estimate the volume of blood, which can inform if surgical intervention is needed.
The signs that surgery might be needed include, draining over 1500 ml of blood in 24 hours through the chest tube, drainage of 300-500 ml per hour for 2 to 4 consecutive hours after the chest tube insertion, injury to a main blood vessel or the chest wall, or pressure buildup around the heart (pericardial tamponade). Surgery can allow doctors to quickly assess the injuries within the chest, and stop any bleeding.
It’s important to be cautious when dealing with a hemothorax condition in a patient who has a blood clotting disorder. Their clotting function should be corrected before any surgical intervention, if their condition allows for it. If blood in the chest is not properly drained, it can lead to complications such as infection within the chest (empyema) and scarring of the lung tissue (fibrothorax).
Multiple studies have highlighted the benefits of a minimally invasive surgical technique called Video-Assisted Thoracoscopy (VATS) for managing blood in the chest. VATS can reduce hospital stays and improve patient survival. It gives doctors a clear view of the chest cavity, assists with accurately controlling bleeding, and enables them to remove any remaining clots, and treat any infections. In addition, VATS can also be used to check for injuries to the diaphragm or the space around the lungs and heart (mediastinum).
What else can Hemothorax be?
When a patient experiences chest trauma, the doctor needs to consider various potential causes and damages to different parts of the body. These can be summed up in three major categories:
- Visceral injuries: These could include damage to the diaphragm, lungs, chest cavity, windpipe and bronchial tubes, esophagus, or the area around the lungs.
- Skeletal injuries: Damage may have occurred to the chest wall, ribs, collarbone, shoulder blade, spine or any joints present in this area.
- Cardiovascular injuries: Trauma might have caused harm to the heart or the blood vessels near the heart and chest area, such as the aorta, vena cava, arteries near the ribs, or the subclavian artery.
All these possibilities are explored by the doctor before reaching a precise diagnosis.
What to expect with Hemothorax
The risk of harm and the chance of dying from traumatic hemothorax (bleeding into the chest cavity) are linked with how severe the injury is. Those who are at risk of late complications, such as empyema (infection in the chest cavity) and fibrothorax or trapped lung (scar tissue in the chest), can face more serious results.
Patients with retained hemothorax (where the blood hasn’t been fully drained from the chest) are at risk of developing empyema, which can result in a prolonged stay in the intensive care unit or the hospital.
Possible Complications When Diagnosed with Hemothorax
Complications from using thoracic ultrasound are usually minor, though you might experience some soreness where the probe was placed on your body.
If your doctor uses a thoracic ultrasound to help treat a serious condition like massive hemothorax (a large amount of blood in the space between your lungs and chest wall), there can be more serious complications. These can include:
- Unstable heart rate and blood pressure
- Shock
- Low oxygen levels
- Risk of death
Additionally, if a chest tube isn’t placed correctly, it could injure an organ. Also, if a chest tube isn’t effective in draining a hemothorax, you could be at risk for developing an infection in your chest cavity, also known as empyema. Research shows that about 26.8% of patients with un-drained hemothorax after trauma develop an empyema.
Improper hemothorax drainage can also lead to another condition: fibrothorax. Fibrothorax occurs when too much scar tissue forms in the pleural space (the area between the membranes lining the lungs). This can cause an inflammatory layer within the chest cavity that stops the lungs from expanding properly (a condition called lung entrapment).
Preventing Hemothorax
Research indicates that not using seat belts and driving while under the influence significantly increases the risk of serious injuries in car accidents. It’s crucial for health professionals to recommend safety practices like always wearing seat belts, avoiding driving if impaired, and considering other forms of transportation when necessary.