What is Neonatal Respiratory Distress Syndrome?
Neonatal respiratory distress syndrome, or RDS, is a common reason for breathing troubles in a newborn baby, appearing usually within hours after birth, most commonly right after delivery. RDS mainly affects preterm (born too early) babies, and rarely, full-term babies. This syndrome’s occurrence is closely related to the baby’s gestational age, which is how long the baby spent in the womb, with the smallest and earliest-born babies getting the severest forms of the disease. While treatments such as antenatal corticosteroids (drugs given before birth), surfactants (a kind of lung medication), and cutting-edge respiratory care for the newborn have made things better for patients with RDS, it still remains a leading cause of sickness and death in preterm babies.
What Causes Neonatal Respiratory Distress Syndrome?
Neonatal respiratory distress syndrome (RDS) happens when a baby doesn’t have enough surfactant in the lungs. This condition can be due to either not enough surfactant production, or because the surfactant is not working the way it should in lungs that haven’t fully developed yet. Babies that are born prematurely can have this issue because their lungs aren’t fully developed, and they can’t produce enough surfactant.
Surfactant and Fetal Lung Development
To understand why RDS happens, it’s important to understand how a baby’s lungs develop and how surfactant is produced. A baby’s lungs develop in several stages, from the embryonic stage, to pseudo glandular, canalicular, saccular, and alveolar stages.
The process starts around 26 days into pregnancy when the lung bud appears. This lung bud divides and infiltrates the surrounding mesenchyme, forming the main breathing tubes by 37 days. These tubes branch out more, forming smaller breathing passages by 48 days. At the same time, lung blood vessels also start to form.
The pseudo glandular stage starts around the fifth week and ends at the sixteenth week of pregnancy. During this stage, there is the development of the important tissue types that make up the structure and function of the lungs. The airways branch out 15 to 20 times by the 18th week of pregnancy.
The canalicular stage starts around the 16th week and ends around the 25th week. This is when the acini (small sacs where gas exchange happens) begin to form, a blood-air barrier is established, and surfactant production begins via specialized cells called type 2 cells. This stage ends with a lung that is potentially able to do gas exchange.
From the 24th week to the 32nd week, the saccular stage occurs, during which the tiniest parts of the lung that allow for gas exchange are formed. It is from this stage that a baby born prematurely has potential to survive outside the womb.
At 32 weeks, the alveolar stage begins, and tiny air sacs in the lungs called alveoli start to form. These increase the surface area for gas exchange. By term age, the lung contains 50 to 150 million alveoli.
Surfactant covers the inner lining of the alveoli. During fetal life, surfactant production begins around 20 weeks gestation. It is made mostly of lipids and proteins, with some of the proteins also playing a role in controlling inflammation. Some proteins, such as SP-B, are critical for normal formation of lamellar bodies in the type 2 cells and are also involved in processing another protein, SP-C, which works together with SP-B to enhance surfactant function by lowering surface tension.
The lung experiences force due to its elastic tissue and the surface tension of air-fluid interfaces in the small airways and alveoli. The surfactant is significant as it decreases the surface tension, which prevents the alveoli from collapsing. The type 2 cells reabsorb the surfactant complex from the airspace; this process of recycling maintains the surfactant pool. Babies born prematurely often have less surfactant, and the surfactant can be less effective due to its composition.
Genetics
There have been observations that identical twins have a higher incidence of RDS compared to non-identical twins, and an increased incidence of RDS has also been reported in families, suggesting that genetics may play a role. In some cases, infants with genetic causes of surfactant protein deficiency can also present with varying degrees of RDS. Some of these genetic mutations can result in severe RDS and progression to severe respiratory failure. However, the exact incidence of fatal RDS in this population is currently unknown.
Risk Factors and Frequency for Neonatal Respiratory Distress Syndrome
Respiratory distress syndrome (RDS) is the leading cause of breathing problems in newborns who are born prematurely. Approximately 24,000 infants are affected by this condition every year in the United States. Being premature and having a low birth weight are the two main factors that increase an infant’s risk of developing RDS. However, other factors can also contribute to the risk, such as being of white ethnicity, male, a late preterm delivery, or having a mother with diabetes. It’s also riskier if the baby experienced a lack of oxygen (hypoxia) and insufficient blood supply (ischemia) around the time of birth, or if there was no labor during the delivery.
The chance of a baby developing RDS decreases as the pregnancy progresses. This means that the younger a baby is at birth, the more likely they are to develop the condition. For instance, nearly all babies born at 24 weeks (98%) developed RDS in a particular study from 2003 to 2007. The rate drops to 5% if the baby is born at 34 weeks, and it’s less than 1% for babies born at 37 weeks.
Signs and Symptoms of Neonatal Respiratory Distress Syndrome
Neonatal respiratory distress syndrome usually affects babies who are born prematurely. They start to show signs of breathing difficulties quickly, sometimes immediately after birth, or within a few minutes. Typically, these babies have decreased breath sounds and their pulses may be weaker. Upon checking the baby, doctors will often notice the baby is having difficulty breathing. This can be seen through fast breathing, grunting when breathing out, flaring of the nostrils, and signs of additional muscle strain when breathing.
These muscles include those below the ribs (subcostal), below the sternum (subxiphoid), between the ribs (intercostal), and above the sternum (suprasternal). The baby may also appear blue due to lack of oxygen (cyanosis) and display signs of poor blood flow to the hands and feet. In severe cases, if the condition is not treated, the symptoms can get worse over 2 to 3 days and can lead to breathing failure. The baby may become less alert and have pauses in breathing (apnea). Other signs may include swelling of the arms and legs and producing less urine.
- Fast breathing
- Grunting when breathing out
- Nostril flaring
- Extra muscle use during breathing, seen in the subcostal, subxiphoid, intercostal, and suprasternal muscles
- Cyanosis (blueness due to lack of oxygen)
- Poor blood flow to hands and feet
- Decreased alertness, if condition worsens
- Pauses in breathing, if condition worsens
- Swelling in the arms and legs
- Less urine being produced
Testing for Neonatal Respiratory Distress Syndrome
If a newborn is suspected of having neonatal respiratory distress syndrome, which is a condition that makes it difficult for them to breathe, it’s necessary for the doctor to look at several things. This includes the baby’s prenatal history and delivery, the symptoms the baby is showing, x-ray results, and blood tests that show how much oxygen is in the baby’s blood.
The symptoms may include rapid breathing, flared nostrils, grunting noises with each breath, the baby pulling in its chest and abdomen while breathing (retractions), and a bluish color to the skin (cyanosis). Also, when the doctor listens to the baby’s lungs, the sounds may be quieter than expected.
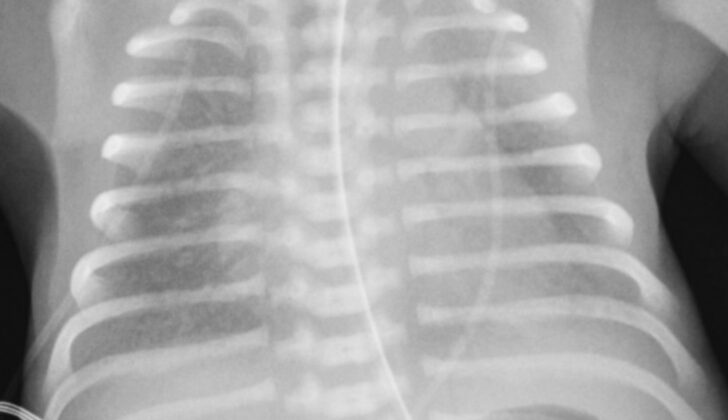
In addition, the doctor may use a chest x-ray to get a better look at the baby’s lungs. In newborns with this condition, the lungs typically show a uniform disease pattern with collapsed regions, sometimes described as having a sandy or grainy look, with air-filled pockets or bronchograms due to collapsed tiny air sacs called microalveoli. This pattern on the x-ray is a classic sign of respiratory distress syndrome.
Arterial blood gas analysis, another kind of blood test, may also be used. This test measures how much oxygen is in the baby’s blood and can indicate low oxygen levels that may improve with added oxygen, and increased carbon dioxide levels. If the syndrome gets worse, doctors may see evidence of increasing acid levels in the blood due to difficulty in breathing and accumulation of lactic acid.
The doctor might also perform other tests like an echocardiogram, a test that uses sound waves to take pictures of the heart, to look for a heart issue that could complicate the baby’s condition. Additional blood tests might show signs of anemia or infection. Sometimes, tests may be done on blood, cerebrospinal fluid (the fluid around the brain and spinal cord), and tracheal cultures (cultures from the windpipe) to check for an infection as well.
Treatment Options for Neonatal Respiratory Distress Syndrome
The best management strategies for a newborn experiencing respiratory distress syndrome aim to cut down the frequency and severity of this condition. The strategy involves preemptive use of corticosteroids before birth, then providing the newborn with respiratory support, surfactant therapy, and proper care.
Before the baby is born, corticosteroids are used to enhance the development of the baby’s lungs. After birth, the baby’s oxygen levels and breathing are closely monitored. If necessary, the baby may be given help with breathing. Surfactant therapy might be used which involves giving the baby a substance called surfactant, which helps the lungs function properly. Supportive care comes next, which includes maintaining the baby’s body temperature, providing the necessary nutrition, managing fluids and salts in the baby’s body, and using antibiotics if necessary.
Close monitoring of the baby’s oxygen levels and breathing is necessary. This is done through blood tests and pulse oximetry, a simple and painless test that measures the oxygen in the baby’s blood. The oxygen level in the baby’s blood will be maintained within a certain range. If the oxygen level rises above the specific range, it can complicate the measures to monitor the condition of the baby.
If the baby is struggling to breathe, various forms of assisted ventilation may be used. The preferred method is to start continuous positive airway pressure (CPAP) early. CPAP is a treatment that uses mild air pressure to keep the airways open. With CPAP, the baby might need less surfactant therapy, and the chances of developing chronic lung disease may also reduce.
Other forms of non-invasive respiratory support might be used, such as nasal intermittent positive pressure ventilation, which adds pressure to the baby’s breathing using a ventilator. Another method is high flow nasal canula where the baby receives warm, humidified air through tubes in the nostrils. If the baby does not respond to these treatments and has severe breathing problems, then invasive mechanical ventilation might be necessary, which involves using a machine to help the baby breathe.
Surfactant therapy is a targeted treatment for a deficiency in a substance called surfactant, which helps the lungs function properly. It is given through a breathing tube and can be beneficial if administered shortly after the baby’s birth. Surfactant can speed up recovery and reduce the risk of various complications. However, for babies who receive surfactant after they develop respiratory distress syndrome, there is an increased risk of premature apnea, a condition where the baby stops breathing.
Next comes supportive care. If the baby has premature apnea, caffeine therapy might be necessary. Along with caffeine, proper management of fluids and salts in the baby’s body is also crucial. Some babies may need additional fluids or medications for low blood pressure. Additionally, the baby’s body temperature, nutrition, and anemia should be managed well, and treatment for a condition called patent ductus arteriosus may also be necessary. The baby might also need antibiotics.
What else can Neonatal Respiratory Distress Syndrome be?
Newborn babies can experience a condition called respiratory distress syndrome for many reasons, including:
- Temporary quick breathing after birth, known as transient tachypnea of the newborn
- Lung disorders that allow air to leak, like pneumothorax or pneumomediastinum
- Pneumonia in newborns
- Aspiration of meconium (a newborn’s first feces)
- Persistent high blood pressure in the lung (pulmonary hypertension)
- Heart diseases present from birth that cause low levels of oxygen in the blood (cyanotic congenital heart disease)
- Disease that affects lung tissue (interstitial lung disease)
Transient tachypnea of the newborn happens when the leftover fluid in a baby’s lungs from being in the womb doesn’t get absorbed as it should. This causes the baby to breathe quickly right after birth. Usually, this eases off after the first 24 hours.
Pulmonary air leak syndromes might cause breathing issues, but symptoms often come on more suddenly compared to other causes. Some signs include uneven chest movement when breathing, or weaker breath sounds on one side of the chest. If air leaks are serious, they might show up as overly bright areas on a chest x-ray.
Pneumonia caused by bacteria, particularly Group B Streptococcus, in a newborn often looks a lot like respiratory distress syndrome, both in how it appears to doctors and on x-rays. The typical treatment for this is antibiotics, along with managing breathing issues.
Newborns with cyanotic congenital heart disease can have similar symptoms, but their chest x-rays will look different. Instead, the x-ray results will vary based on the specific heart condition.
What to expect with Neonatal Respiratory Distress Syndrome
The outlook for newborns treated with antenatal steroids, respiratory support, and surfactant therapy (a treatment to help premature lungs function better) is excellent. The rate of these infants not surviving is less than 10%, and some studies show survival rates as high as 98% with advanced care.
This good survival rate in developed countries significantly contrasts with that in low-income countries, where the rate of premature babies with RDS (Respiratory Distress Syndrome, a breathing disorder in premature babies) not surviving is often near 100% if no medical intervention is given.
Just with proper breathing support, the baby eventually starts producing surfactant naturally. This, along with the beginning of diuresis (when the body gets rid of extra fluid through urine), usually leads to an improvement in RDS within 4 or 5 days. However, without treatment, severe oxygen deficiency in the first days of life can lead to failure of multiple organs and death.
Possible Complications When Diagnosed with Neonatal Respiratory Distress Syndrome
Neonatal respiratory distress syndrome can lead to various complications that are linked mainly to the disease’s progression and the long-term wellbeing of the babies affected. Surfactant therapy has helped reduce these complications, but some babies continue to experience challenges during and after the disease’s critical stage.
These acute complications often occur due to the use of positive pressure ventilation or invasive mechanical ventilation, leading to air-leak syndromes such as:
- Pneumothorax
- Pneumomediastinum
- Pulmonary interstitial emphysema
Babies with a very low birth weight, who also have this syndrome, have a higher chance of getting a brain bleed (intracranial hemorrhage) and an open blood vessel in the heart (patent ductus arteriosus), though these can also occur due to prematurity itself.
A chronic long-term complication of this syndrome is bronchopulmonary dysplasia (BPD). This occurs when lung development is disrupted due to inflammation and injuries to the lung. Also, oxidative stress from too much oxygen secondary to mechanical ventilation, and a premature lung’s inability to handle this, can further damage the lung.
Late development (neurodevelopmental delay) and a condition causing uncontrolled muscle movements and stiffness (cerebral palsy), are other potential complications especially in infants who needed long-term mechanical ventilation. The chance of these conditions occurring increases with the duration of mechanical ventilation and as the gestation period at birth decreases.
Preventing Neonatal Respiratory Distress Syndrome
Scientists are still working on finding ways to completely prevent premature births. However, the condition called Respiratory Distress Syndrome (RDS), which can occur in prematurely born babies, can be effectively reduced with the help of medication known as antenatal corticosteroids. By giving this medication to expecting mothers, the risk of RDS, and the need for their baby to be put on a ventilator can be lowered significantly.
These findings come from an analysis of multiple studies involving over 4000 infants. The medication not only lowered instances of RDS but also reduced cases of infant death and brain damage (periventricular leukomalacia). Importantly, there was no noticeable increase in death rate among mothers who were given these steroids.
But, the benefits of giving this medication after 34 weeks of pregnancy is still a debated topic due to gaps in data about long-term development of the child. Currently, doctors recommend this medication for women who may deliver prematurely, specifically between the 23rd and 34th week. In some cases, if there is a high risk of premature delivery in the next week, this medication may be given at 22 weeks.
Despite many efforts and different treatments, the complete prevention of premature birth still remains a challenge.