What is Pulmonary Contusion?
The lungs are the primary organs responsible for breathing, located within a protective cage made of bones and tissues known as the thorax and pleurae. The top part of the lungs can be felt just above the collarbones, while the lower edges run along the ribs. Each lung is divided into sections called lobes, and they contain tiny air sacs called alveoli which are the building blocks of the lungs where oxygen and carbon dioxide are exchanged.
Air travels to and from the lungs through the tracheobronchial tree, a series of branching tubes. The tree starts with the trachea which splits into two main bronchi—one for each lung. These further divide into smaller tubes, called lobar and segmental bronchi, which supply the different lobes of the lungs. Eventually, these tubes end in the smallest branches, the respiratory bronchioles, which lead to the alveoli where gas exchange occurs.
The lungs get their blood supply from the right and left pulmonary arteries which carry carbon dioxide-rich blood from the body to the lungs. After gas exchange in the alveoli, the oxygenated blood is carried back to the heart by the pulmonary veins. The bronchial arteries carry oxygenated blood to the bronchi and other lung tissues, while the bronchial veins and lung lymphatic vessels drain used blood and lymph fluid, respectively.
A pulmonary contusion is a type of injury to the lung tissue that does not cause cuts to the lung or its blood vessels. It’s usually caused by blunt force trauma to the chest, shockwaves from puncture wounds, or explosions. Pulmonary contusions were first identified in 1761. Detailed studies during World Wars I and II found that many soldiers who were near an explosion developed lung bleeding, which is a symptom of pulmonary contusions, even without apparent injuries on the outside of the body.
What Causes Pulmonary Contusion?
Chest injuries can cause a condition known as a pulmonary contusion, which is essentially a bruise on the lung. These injuries could be caused by a blow to the chest, a penetrating injury, or a combination of both. Other triggers can include violent events like explosions or assaults, accidents like falls from high locations or car crashes, and sports collisions.
Severe chest injuries often result in broken breastbones. But interestingly, older adults are more likely to develop lung contusions, even when their chest injuries are relatively minor. It’s also worth knowing that lung contusions are a common issue for people who have broken ribs.
Risk Factors and Frequency for Pulmonary Contusion
Pulmonary contusions, or lung bruises, are fairly common, although their exact prevalence is unclear due to limitations in research studies. They account for a large proportion of injuries observed in those who had blunt chest trauma, where they make up 30% to 75% of lung injuries. Additionally, these injuries present a higher risk, leading to a fatality rate of about 10% to 25%. They are the second leading cause of death in people suffering from blunt thoracic injuries, right after injuries relating to the head and spinal cord. Pulmonary contusion is also frequently seen in cases where the breastbone is fractured, making up about a third of these cases. While fractures of the scapula, or shoulder blade, are uncommon, over 90% of these cases are associated with severe injuries and lung contusions.
- Pulmonary contusions are fairly common, but their exact prevalence is unclear.
- They account for 30% to 75% of lung injuries in blunt chest trauma cases.
- The fatality rate for people with pulmonary contusions is 10% to 25%.
- They are the second most common cause of death in people with blunt thoracic injuries, after injuries to the head and spinal cord.
- Pulmonary contusions are seen in about a third of cases where the breastbone is fractured.
- Over 90% of rare scapula fractures are associated with severe injuries, including lung contusions.
Signs and Symptoms of Pulmonary Contusion
Patients who have experienced significant injuries to the chest may become unresponsive and have difficulty breathing or no pulse at all. These individuals need immediate medical treatment to revive them, no matter what caused their condition. Once they’ve been stabilized, the medical team can perform a more thorough examination to assess any further issues.
When someone has a seriously bruised lung, symptoms can vary depending on how severe the injury is. Difficulty breathing, chest pain, and coughing up blood can be signs of a severe lung contusion. Those with a milder injury might not show any symptoms at all. However, these symptoms usually follow a trauma or injury and may indicate the possibility of other concurrent injuries.
Severe lung contusions can cause rapid breathing and increased heart rate, and it’s often clear to see that the individual is struggling to breathe in the early stages. Their oxygen levels in the body may be low. Other signs might include the chest visibly retracting inwards as they breathe, a swollen neck vein, and a blue discoloration of the skin due to lack of oxygen. Listening to their breathing could reveal lower than normal breath sounds. Other injuries may also be evident. As the contusion becomes more severe, the patient may experience low blood pressure, slow or stopped breathing, altered consciousness, and a slow heart rate.
For serious contusions, symptoms can show up within a few hours. But for milder injuries, symptoms might not appear until 24 to 48 hours after the trauma.
Testing for Pulmonary Contusion
In order to diagnose a lung injury, such as a pulmonary contusion (a bruise of the lung), a doctor uses several methods. This usually involves getting your personal account of the injury, undergoing a thorough physical examination, and carrying out imaging tests. The types of imaging tests your doctor might use include chest X-rays, CT scans (like a super-detailed X-ray that uses computer processing to create more images), and ultrasound (a machine that uses soundwaves to create pictures of the inside of your body).
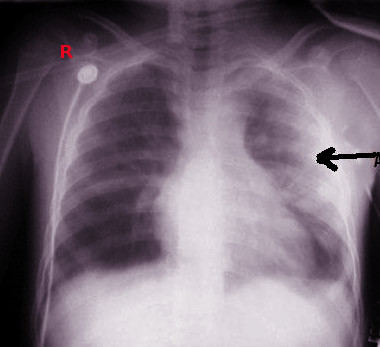
The chest X-ray is the most commonly used imaging technique for diagnosing lung injuries. However, interpreting these images can be challenging as the bruised areas of the lung do not always respect the normal borders of the lung. Furthermore, other injuries such as a pneumothorax (collapsed lung) or hemothorax (collection of blood in the chest) can obscure other injuries. Sometimes, signs of a contusion may not even show up on a chest X-ray immediately and may take between 6 to 48 hours to appear.
A mild lung contusion may show up as a foggy area on a chest X-ray, while a severe injury may resemble pneumonia (lung infection). However, unlike pneumonia which is usually confined to specific areas of the lung, a pulmonary contusion can spread across different parts of the lung. If the chest X-ray is inconclusive, your doctor may recommend a CT scan for further evaluation.
A chest CT scan is more sensitive than plain X-rays for detecting lung contusions, and it could spot these injuries immediately after trauma. A special three-dimensional chest CT can also measure the volume of the injured lung area which is helpful in identifying patients at higher risk of ARDS (a severe lung condition that causes breathing difficulties). Patients with a contusion volume of at least 20% are viewed as having a severe condition and are more likely to develop ARDS and pneumonia than patients with contusion volumes of less than 20%.
An ultrasound is a powerful tool that clinicians use at the bedside to help quickly identify lung contusions, particularly when a chest X-ray or CT scan can’t be done immediately. An ultrasound exam called E-FAST, which includes a chest exam, can help plan treatment more quickly in patients with lung injuries.
An Electrocardiogram (ECG), a test that measures the electrical activity of your heart, is also crucial when checking patients with chest injuries. This test is particularly important because a heart contusion (bruise of the heart), which can be life-threatening, is also a possibility with these types of chest injuries. For instance, a direct blow to the chest during a sports collision can trigger an irregular heartbeat like ventricular fibrillation, leading to a fatal condition known as “commotio cordis”.
Treatment Options for Pulmonary Contusion
Most injuries to the lungs, known as pulmonary contusions, require supportive care to give the injury time to heal. It’s important to keep a close eye on these injuries as they can become worse 24 to 48 hours after the initial trauma. The main goal in treating lung injuries is to prevent respiratory insufficiency, a condition where the lungs can’t provide the body with enough oxygen. To avoid this, patients need sufficient pain relief to prevent the tensing of chest muscles and allow for the lungs to expand fully.
Supportive care can include various therapies to prevent the collapse of the tiny air sacs in the lungs, a condition known as atelectasis. These therapies can range from postural drainage and suction therapy to deep breathing exercises and coughing encouragement. Managing any associated injuries, such as broken ribs or breastbone fractures, is also crucial. Adequate pain control can help improve lung function by allowing the lungs to expand and preventing atelectasis.
An injury to the lung can indicate an increased need for a medical procedure known as tracheal intubation, which involves placing a flexible tube into the windpipe through the mouth or nose. The settings for such a procedure need to be carefully chosen to keep the air sacs in the lungs open and recruit more air sacs, all while avoiding injury to the lungs from too much pressure, known as barotrauma. If a patient does not require intubation, continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP) can be used.
Positioning a patient with a lung injury on their stomach can help reduce pressure on the diaphragm, the main muscle involved in breathing. Also, positioning the injured lung in a position that doesn’t bear weight can help recruit more air sacs. However, noninvasive ventilation, a therapy that helps a patient breathe better without the need for intubation, may not be suitable for patients with impaired consciousness as it can cause stomach distention and aspiration, when food or liquids are accidentally inhaled into the lungs.
Patients may need invasive ventilation, where a machine supports breathing, if positive pressure ventilation fails. This needs to be done carefully as large tidal volumes, the amount of air moved into or out of the lungs during each breath, can increase the risk of barotrauma. It’s recommended to start with a low tidal volume.
Diuretics, medicines that help reduce fluid in the body, can be used to decrease pressure in the small blood vessels of the lungs and help avoid fluid accumulation in the lungs. If fluid therapy, a treatment to replace lost fluids, is needed to maintain balance in the body, measuring the pressure in the pulmonary artery can help prevent a buildup of fluid in the lungs, a condition known as pulmonary edema.
Surgery may be necessary for patients with multiple broken ribs or a flail chest, where a portion of the rib cage moves separately from the rest of the chest wall, to correct the mechanics of the lungs. Surgery to fix broken ribs can reduce the number of days a patient with mild to moderate lung injuries needs to rely on a ventilator. For patients with low levels of oxygen in the blood that don’t respond to conventional treatments, a treatment called venovenous extracorporeal membrane oxygenation (vv-ECMO), which provides prolonged cardiac and respiratory support, has been found to be effective.
What else can Pulmonary Contusion be?
If you’re finding it hard to breathe after an injury, the problem could be due to a number of different conditions. These might include:
- Diseases of the lungs: cuts or tears in the lung (lung laceration), pneumonia, blood in the chest cavity (hemothorax), air in the chest cavity (pneumothorax), fluid in the lungs (pulmonary edema), a blockage in the lung’s blood vessels (pulmonary embolism), an injury to the lungs related to a blood transfusion (TRALI), or asthma
- Heart-related conditions: bruises on the heart (cardiac contusion), heart attack (myocardial infarction), air in the middle part of the chest (pneumomediastinum), inflammation of the heart (myocarditis), a tear in the aorta (the main blood vessel in the body; aortic dissection), or pressure on the heart due to fluid buildup (cardiac tamponade)
- Conditions related to the muscles and bones: broken ribs, an object stuck in the body (foreign body injury), or a bruise on a muscle
- Mental health conditions: panic attack, rapid breathing (hyperventilation), or anxiety disorder
- Whole-body (systemic) conditions: poisoning, severe allergic reaction (anaphylaxis), or build up of acid in the body (acidosis)
A thorough check-up can help healthcare providers to figure out whether these conditions or a bruise on the lung (pulmonary contusion) is causing the problem.
What to expect with Pulmonary Contusion
Pulmonary contusions, or lung bruises, typically heal within 5 to 7 days with proper care and support. A study involving 73 patients with this condition found that 38.4% developed pneumonia and 6.8% advanced to severe lung problems known as Acute Respiratory Distress Syndrome (ARDS). Also, 52.1% of the patients had a contusion volume (the size of the bruise) greater than 20%.
In some cases, those who recover from severe pulmonary contusions might suffer from chronic lung disease. This can lead to a decreased functional residual capacity, meaning reduced air remaining in the lungs after a normal breath out.
The rate of death from lung contusions can vary greatly, from 14% to 40%, mainly based on the seriousness of any associated injuries.
Possible Complications When Diagnosed with Pulmonary Contusion
Pulmonary contusions, or lung injuries, can lead to pneumonia, a severe lung condition called ARDS (Acute Respiratory Distress Syndrome), and breathing problems which often require support like a breathing machine. People with multiple injuries have a higher chance (78%) to develop ARDS compared to those with only lung injuries (17%). The main causes of death within the first month after a pulmonary contusion are ARDS (44.1%) and respiratory infections (26.5%).
Potential Complications:
- Pneumonia
- ARDS (Acute Respiratory Distress Syndrome)
- Respiratory failure (Breathing problems requiring support)
- Death caused by ARDS
- Death caused by respiratory infections
Preventing Pulmonary Contusion
There are several ways you can help avoid injuries to your lungs, or pulmonary contusions:
– Always remember to wear seatbelts, use airbags, and install age-appropriate car seats when you’re driving
– If you are likely to fall, take steps to prevent this from happening
– Abide by safety rules at your workplace
– If you play sports, always wear the right protective gear
– Steer clear of risky behaviors
Even with adhering to these precautions, lung injuries might still happen. So, it’s crucial that you seek medical help right away if you ever suffer from a trauma to the chest.