What is Tension Pneumothorax?
Pneumothorax is a medical term used for describing a condition where air gathers in the pleural space. The pleural space is the thin pocket of air between the lung and the chest wall. When this happens, the pressure causes the lung to collapse. If this condition gets worse, it can evolve into tension pneumothorax, which involves air pressure pushing against the mediastinum. The mediastinum is the area in the middle of the chest that contains the heart, large blood vessels, and the windpipe. Tension pneumothorax is a dangerous condition and can be fatal if untreated. It can happen anywhere, including in ambulances, emergency departments, and intensive care units.
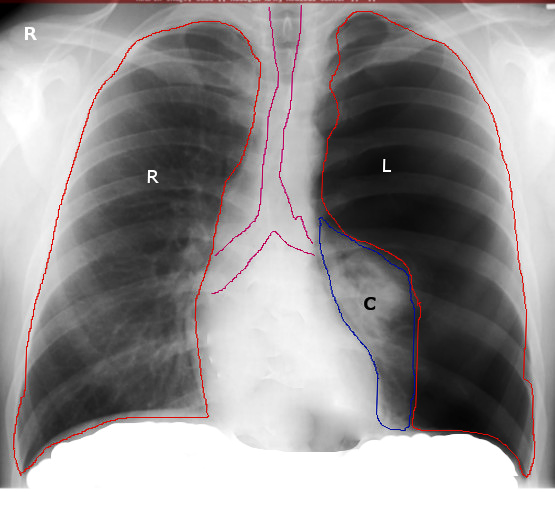
Let’s break it down a little more. The chest area or the thorax is made up of three sections: the right lung, left lung, and the mediastinum in the center. The lungs are each enveloped by a lining called the pleura. Pleura is like a protective wrapping around the lungs, and between this wrapping is a slim space called the pleural cavity. This cavity is usually lubricated by a fluid which makes it easier for the lungs to move when we breathe.
When we breathe in, our diaphragm (a muscular sheet below the lungs) moves down and our ribs move outward. This makes the lungs expand as the pressure inside the pleura decreases. When we breathe out, the diaphragm moves up and the ribs move inward, causing the lungs to shrink and push air out.
If the pleura gets damaged in any way, air can escape into the pleural cavity. This causes positive pressure which contracts the lung, affecting its ability to absorb oxygen and remove carbon dioxide. If the pressure becomes too high, it can press against the mediastinum and affect important structures including the heart, large blood vessels, and the windpipe. This results in tension pneumothorax, which can affect breathing, blood return to the heart, and the heart’s output of blood to the body.
Recognizing and managing tension pneumothorax as soon as possible is vital. Emergency chest decompression, a procedure that removes air from the chest cavity, can save lives and is a skill all healthcare professionals should have.
What Causes Tension Pneumothorax?
Pneumothorax, also known as a collapsed lung, can happen due to an injury (traumatic) or occur without a clear cause (atraumatic).
If you’re not in a hospital when it happens, a traumatic pneumothorax can occur due to a penetrating or blunt injury, a broken rib, or from a condition called decompression sickness, which can happen to divers.
In a hospital, a traumatic pneumothorax can happen after certain medical procedures. These include:
* Inserting a central venous catheter (a thin tube placed into a large vein in your neck or chest)
* Lung biopsy (removal of lung tissue for testing)
* Positive pressure ventilation (a technique that helps you breathe)
* Percutaneous tracheostomy (a surgical procedure to make an opening in your neck to help you breathe)
* Thoracentesis (draining fluid from around your lungs)
* Pacemaker insertion (a small device placed in the chest to help control heart rhythms)
* Bronchoscopy (a test that allows your doctor to examine your airways)
* Cardiopulmonary resuscitation (CPR, a life-saving technique)
* Intercostal nerve block (a pain control procedure)
When pneumothorax occurs without an injury, it’s referred to as atraumatic pneumothorax. It can either have no known cause (primary) or it could be a complication of an existing lung disease (secondary).
Tension pneumothorax, a severe type of pneumothorax, can also be caused all by all the scenarios mentioned above.
while the trachea and heart are displaced toward the right.
Risk Factors and Frequency for Tension Pneumothorax
The exact number of tension pneumothorax cases is hard to pinpoint as most patients receive treatment before reaching trauma centers. Among patients who have undergone trauma, about 20% also experience pneumothorax or tension pneumothorax. Extreme chest injuries can be associated with pneumothorax up to 50% of the time. The likelihood of a traumatic pneumothorax will depend on the size and type of injury. A review of military deaths pointed that as much as 5% of soldiers with chest injuries died from tension pneumothorax.
Traumatic and tension pneumothorax cases occur more often than spontaneous pneumothorax. Tension pneumothorax may also develop in 1-2% of cases that initially present as spontaneous pneumothorax without a clear cause. Furthermore, the rate of iatrogenic pneumothorax, which is caused by medical interventions, is going up in U.S. hospitals due to the widespread use of Positive Pressure Ventilation (PPV) and Central Venous Catheter (CVC). Making multiple attempts to insert the catheter, using the subclavian vein for the catheter, or using PPV can all increase the risk of pneumothorax.
The risk of a pneumothorax relating to a CVC insertion increases when inserted into the internal jugular or subclavian vein. Pneumothorax can occur in about 1% to 13% of the cases after CVC insertion, and this can rise to 30% under certain circumstances. Using ultrasound while inserting a CVC can help reduce this risk.
Iatrogenic pneumothorax usually causes significant illness but it rarely leads to death. Every 10,000 hospital admissions sees about 5 to 7 cases of iatrogenic pneumothorax. A recent study found that 95% of observed pneumothorax instances resulted from medical interventions. Among these, about 69.6% were due to barotrauma from a mechanical ventilator, with 41.1% of these cases escalating to tension pneumothorax. CVC insertion was the cause for about 13.2% of the cases.
Signs and Symptoms of Tension Pneumothorax
Tension pneumothorax is a medical emergency. This condition refers to serious lung damage leading to life-threatening symptoms and it requires immediate diagnosis and help. The main symptoms that might indicate the presence of a tension pneumothorax include severe difficulty in breathing, lower blood pressure, and a noticeable increase in the size of one side of the chest. There would also be no audible breath sounds when a doctor tries to listen to the chest. A shift in the position of the windpipe and organs in the chest cavity could indicate tension pneumothorax. Inserting a large needle into the chest and observing air escape can confirm the diagnosis.
The cause of tension pneumothorax is often linked to a patient’s medical history. Recent trauma or medical procedures like positive pressure ventilation or central venous catheter can contribute to its occurrence. Some people may already have lung diseases like asthma or pneumonia. Common complaints include sharp pain in the chest, spreading to the back or shoulder of the affected side.
Other early signs of tension pneumothorax include:
- Rapid breathing
- Fast heart rate
- Skin pulling inwards between the ribs when breathing
- Blue or purple skin color
- Distended veins in the neck
- Reduced sensation of vibration in the chest
- An abnormal ‘drum-like’ sound when tapping on the chest
- Air bubbles underneath skin in some cases
This can be a critical condition and patients can worsen rapidly. If left untreated, tension pneumothorax can lead to cardiac arrest. If a patient is unconscious or without a pulse, it is essential to start resuscitation immediately, regardless of the underlying cause.
Testing for Tension Pneumothorax
When a doctor isn’t certain about a diagnosis, your condition – whether you’re stable or not – can guide them on how to proceed. If you’re not stable, bedside ultrasound, which means an ultrasound done there and then in the room you’re in, can help determine what’s wrong. Patients receiving ultrasound need to be stabilized, where checks are ran to ensure their airway is clear, they’re breathing normally, and their heart is working properly.
The ultrasound process is very effective – about 94% sensitive and 100% specific – when performed by an experienced practitioner. It can identify a pneumothorax (a collapsed lung), which can be particularly helpful in patients who aren’t stable. The ultrasound looks for signs such as an absence of natural lung movement or the presence of a “lung point.”
If there is still doubt about the diagnosis even after the ultrasound, there’s a procedure called needle decompression that might be performed. This treatment involves inserting a needle or tube into the chest cavity to relieve pressure and allow the lungs to re-inflate.
When you are stable, an X-ray of the chest is usually the first diagnostic step. Some signs that pneumothorax might be present include evidence of a thin line that is actually the edge of a lung membrane, areas of the lung that suddenly lose their normal print pattern, or a full collapse of the lung on one side. In serious cases, the X-ray might show that parts of the chest – like the heart and lungs – have shifted over, away from the pneumothorax, or air could be seen under the skin.
If the X-ray isn’t enough to diagnose you, a CT scan of the chest may be carried out. CT scans are the most reliable way to diagnose pneumothorax, but they usually aren’t used routinely due to their high levels of radiation.
Treatment Options for Tension Pneumothorax
Tension pneumothorax, a severe condition where air gets collected in the space around the lungs, can be managed in an emergency department or intensive care unit, and the exact treatment depends on the patient’s stability. When someone comes in with chest injuries, the first step for healthcare professionals is to assess the patient’s ability to maintain an open airway, breathe, and have a steady circulation.
In this condition, chest wounds need to be covered with an airtight dressing and plastic covering. Giving the patient 100% oxygen can help decrease the amount of air around the lung – this process works by creating a gradient that makes the nitrogen in the air pocket diffuse out faster. However, getting the patient to take deep, forceful breaths should be avoided at first, as this could make the pneumothorax worse. This approach can be considered once a chest tube has been inserted.
If the patient is unstable and doctors think they may have a tension pneumothorax, an urgent procedure to let the trapped air out, called needle decompression, is performed. This is done by placing a needle in the area above a certain point on the collarbone. This procedure helps to re-expand the lung, but needs to be done carefully because doing it too quickly can lead to fluid accumulation in the lungs. After this, a chest x-ray is done, followed by a procedure called tube thoracostomy, which involves placing a tube into the chest to continuously drain the air.
Chest x-rays are done periodically to monitor the healing process. The chest tube can be removed once the lung is fully re-expanded, no new air is leaking out, and the patient’s health has significantly improved.
In most cases of pneumothorax, tube thoracostomy is sufficient. But if it doesn’t help, a surgical procedure involving cameras (video-assisted thoracoscopic surgery, or VATS) or a traditional open-chest operation may be required. These are usually needed for patients whose condition doesn’t improve after several days, or who have had multiple episodes of pneumothorax on the same side, or who have had incidents of decompression sickness (a risk for divers).
During VATS, a procedure called pleurodesis is performed to treat the pneumothorax, which can be done in two ways: mechanical or chemical. Mechanical pleurodesis involves using methods to cause irritation and subsequent adhesion of the layers around the lungs, such as using scratch pads, dry gauze, or strips of tissue around the lung. If the patient cannot tolerate mechanical pleurodesis, chemicals can be used instead – options include talc or certain antibiotics, such as doxycycline, minocycline, or tetracycline.
Studies show that pleurodesis can decrease the chances of recurrence of pneumothorax. Mechanical pleurodesis, in particular, has shown to reduce this risk to less than 5%.
What else can Tension Pneumothorax be?
Tension pneumothorax, a serious lung condition, could be mistaken for other health problems. Here’s a list of conditions that doctors need to rule out:
- Pulmonary embolism (a blood clot in the lungs)
- Acute coronary syndrome (a sudden reduction in blood flow to the heart)
- Acute aortic dissection (a serious condition involving a tear in the large blood vessel branching off the heart)
- Myocardial infarction (a heart attack)
- Pneumonia (a lung infection)
- Acute pericarditis (inflammation of the sac-like covering around the heart)
- Rib fracture (a broken rib)
- Diaphragmatic injuries (damage to the muscle that helps you breath)
The signs that suggest tension pneumothorax, such as severe breathing difficulty, low blood pressure, an enlarged side of the chest, absent breath sounds on one side, and shift of the windpipe to the opposite side, would help doctors distinguish it from these other conditions.
What to expect with Tension Pneumothorax
Tension pneumothorax is a severe medical condition that can quickly progress to severe breathing difficulties, cardiovascular failure, and even death if not identified and treated immediately. Unfortunately, any delay in diagnosis or treatment can lead to disturbing outcomes.
A less severe form, known as uncomplicated pneumothorax, may still reappear within a period of six months to three years. This is especially common in smokers and those who have chronic obstructive pulmonary disease (COPD) – a long-term lung disease that makes it hard to breathe, or acquired immunodeficiency syndrome (AIDS) – a disease that weakens the immune system.
Tension pneumothorax that develops in relation to the use of a ventilator – a machine that supports breathing, has been observed to have devastating results and often leads to death. Interestingly, tension pneumothorax occurring due to a medical procedure tends to have better outcomes compared to those related to ventilator use.
Possible Complications When Diagnosed with Tension Pneumothorax
Tension pneumothorax is a severe and potentially life-threatening condition. If a person survives tension pneumothorax, they might experience several complications. These complications could arise from the lung injury itself or from the chest tube thoracostomy (CTT), a procedure to drain fluid or air from the space around the lungs.
Here are some possible complications:
- Pneumopericardium: Air in the space around the heart
- Pneumoperitoneum: Air in the abdominal cavity
- Hemothorax: Blood in the space around the lungs
- Bronchopulmonary fistula: An abnormal passageway between the bronchial tubes (airways) and the lungs.
- Damage to the neurovascular bundle during CTT: Harm to the group of nerves, veins, and arteries in the chest during the procedure
- Pain and skin infection at the CTT site: Discomfort and risk of infection where the chest tube was inserted
- Empyema: Pus in the space around the lungs
- Pyopneumothorax: The collection of pus and air in the pleural space.
Quick diagnosis and treatment can help improve the outcomes for patients with tension pneumothorax.
Preventing Tension Pneumothorax
Preventing a serious condition called tension pneumothorax involves reducing the risk factors. Here are some crucial steps that you can take to protect yourself:
Firstly, be careful when doing high-risk activities. Things like using seatbelts and adhering to speed limits can prevent car accidents. You can also protect yourself by following safety rules at work and wearing protective gear while playing sports.
Secondly, if you have a long-term lung condition like COPD (Chronic obstructive pulmonary disease) and asthma, it’s important to follow your treatment plan. Keeping these conditions under control can lower the chance of getting pneumothorax, which is a buildup of air in the chest that can cause a lung to collapse.
Thirdly, if you’re a diver or a pilot, practice safe ascent. Decompression sickness is another name for the illness divers can get if they come up to the surface too quickly. To prevent this, you should ascend gradually and avoid drinking alcohol before diving or flying. In addition, if you’re diving, make sure you give yourself enough time between dives and avoid flying soon after a long, deep-sea dive. Staying fit and healthy can also help.
Fourthly, if you smoke, try to quit. Smoking increases the risk of lung conditions that can lead to pneumothorax.
Finally, if you notice any new symptoms, or if existing ones get worse, especially after an injury, you should seek medical attention immediately.
While you can’t predict every case of tension pneumothorax, following these steps can greatly lower your risk and help you avoid serious health complications.












