What is Tracheobronchial Tear?
A tracheobronchial tear is a rare but serious injury that can harm the main airways of your lungs, which include your windpipe (trachea) and the two tubes that deliver air to your lungs (right and left bronchi). These tears can be either partial or complete rips or punctures in these airways, often resulting from a sharp or blunt trauma, or sometimes caused by medical procedures.
Tragically, around 80% of people who get these types of injuries due to blunt trauma may die at the incident site or while being transported to the hospital, due to the severity of the injury and other related injuries. However, survival rates seem to be increasing thanks to advancements in managing patients before they get to the hospital. It’s crucial to suspect, diagnose and manage tracheobronchial injuries early on, in order for the patient to have the best possible chance of recovery.
What Causes Tracheobronchial Tear?
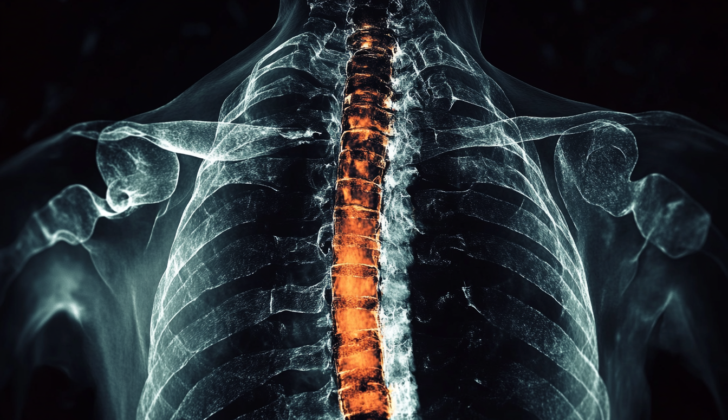
The trachea, also known as the windpipe, is a flexible structure made up of 16 to 20 rings of cartilage. It’s located and shielded close to the breastbone, ribs, and backbone. Tracheobronchial tears refer to injuries to the trachea and bronchi (the main air passages to the lungs). Causes can include sharp injuries (like gunshots or stabs), blunt force (like car accidents or falls), as well as certain medical procedures.
Car accidents are the most common cause of these injuries. People are more likely to suffer a tracheobronchial tear from a piercing injury than a blunt force one. Gunshot wounds are more common than stab wounds but both usually affect the part of the trachea in the neck. Although less common, blunt force injuries can also cause tracheobronchial tears and are associated with a higher mortality rate.
Blunt force injuries to the neck part of the trachea can result from things like whiplash during a car crash or an overextension injury from activities like weightlifting. Direct injuries can occur from things like wire strangulation during snow biking or from seat belts and steering wheels during a car crash.
The part of the trachea in your lower chest is often involved in blunt force injuries. Multiple severe injuries combined generally lead to a higher fatality rate. Severe deceleration, like in a car crash, can injure your airway system in your chest, like your trachea, carina (the point where the windpipe splits into the bronchi), and main bronchi. Most of these injuries occur on the right side, probably due to the larger right lung and shorter right main bronchus.
Tracheobronchial tears can also result from medical procedures like endotracheal intubation (inserting a tube through the mouth into the airway), bronchoscopy (a procedure that allows your doctor to examine your airway), or surgeries. Most of these types of injuries occur at the back part of the airway.
The risk factors for a tracheobronchial tear from a medical procedure can be mechanical (related to the procedure or instruments used, and they are usually preventable) or anatomical (related to the structure or condition of the patient’s airway). Among the latter, being female, being over 65 years old, and having an emergency intubation are the most common non-preventable factors.
Risk Factors and Frequency for Tracheobronchial Tear
It’s challenging to determine the exact number of cases involving damaging injuries to the airway passages caused by forceful or sharp impacts. This is mainly because many victims do not make it to the hospital. There’s a 2 to 3% chance of such injuries happening in those who do not survive the incident. Sharper injuries cause more damage to the airway passages as compared to blunt impacts. Such injuries account for up to 6% of all airway injuries, while chest injuries caused by penetration account for 1 to 2% of airway injuries.
In a long-term study conducted over 20 years, 74% of the patients recorded had cross tears in their airways, with 4% being in the neck airway, 12% in the chest airway, and the remaining injuries in the main branches of the right and left bronchi, and smaller bronchi (25, 17 and 16% respectively). Vertical tears were reported in 18% of the patients, with 6.5% being in the neck airway, 10% in the chest airway and 1.5% in the main bronchi. The remaining 8% of injuries were complex, involving the windpipe and one or both main bronchi.
A German study found 1033 such injuries over five years, with 41.5% of the injuries non-doctor induced, and the remaining 58.4% were doctor-induced. Almost 64.3% of the non-doctor induced injuries were blunt traumas.
Survival rates are lower for blunt traumas as they typically come with more severe wounds. In a research including 104 patients, 23% overall did not survive, and deaths from blunt injury were twice those from penetrating injuries. Likewise, patients coming to emergency with blunt traumas have a 0.5 to 2% chance of an airway injury.
It’s also difficult to determine the exact number of airway injuries caused by medical procedures because they often go undetected or underreported. Airway injuries during esophageal surgeries involving chest and abdominal approach occur in about 1 to 1.8% of the cases.
- The incidence of airway injury with a single-lumen breathing tube is approximately 0.005%.
- With a double-lumen tube, the rate is between 0.005% to 0.19%.
- About 1% of patients experience a tear in the back wall of the airway during a particular type of airway surgery.
According to the same German study previously mentioned, of the medical caused airway injuries, 61.5% were caused during the insertion of a breathing tube or during mechanical ventilation. Nearly 30% were related to specific airway surgeries, and the remaining injuries were linked to endoscopic procedures.
Signs and Symptoms of Tracheobronchial Tear
When a person experiences an injury to their airway, the symptoms they face will largely depend on where exactly the tear is located. Even though this is the case, many people may have non-specific symptoms no matter where the injury occurs. Common symptoms can include trouble breathing, a strained or harsh sound during breathing (known as stridor), and respiratory failure. Respiratory failure occurs when there’s a blockage of the airway. Other symptoms can include swelling due to air trapped under the skin (known as subcutaneous emphysema), hoarseness or complete loss of voice, coughing up blood (hemoptysis), and other symptoms related to the injury.
Some of the most commonly observed signs of tracheobronchial injury, which is damage to the airways in the lungs, are subcutaneous emphysema and pneumothorax, which is a collapsed lung. These signs can occur in 35% to 85% and 20% to 50% of cases respectively. Therefore, if someone exhibits these signs, it should signal the possibility of tracheobronchial injury. Other signals can include air around the lungs and air under the skin. If the injury is closer to the core of the body, it’s more likely to present with air around the lungs, while a more distant injury could result in pneumothorax and air under the skin. Sometimes, a crackling sound that keeps pace with the heartbeat might be heard in cases of mediastinal emphysema. If a persistent air leak or unresolvable pneumothorax is noticed after the insertion of a chest tube, it should raise suspicion of a tracheobronchial tear in a traumatic situation.
Blunt chest injuries can sometimes result in the rupture of the trachea or the main bronchus on the right side of the body leading to air in the abdomen, a condition known as pneumoperitoneum. This happens when the air from around the lungs enters the abdomen through certain openings. After removing a ventilator, some patients might start showing respiratory symptoms, which could be because of an unnoticed tracheal tear. This tear would have been closed by the ventilator tube but reopens after the tube is removed, causing symptoms related to the airway. If air is coming out from a penetrating wound in the neck and it stops after inserting a breathing tube, it could be a telltale sign of a tracheal injury.
Testing for Tracheobronchial Tear
A tracheobronchial tear, or tear in the windpipe and main airways of your lungs, often gets diagnosed based on symptoms, a physical examination, or what doctors find during surgery. It can also be identified through a procedure that involves inserting a small camera through the nose or mouth to look at the airways, known as a bronchoscopic fiberoptic assessment. However, these injuries can sometimes be missed, affecting 25% to 68% of patients. Imaging tests can provide more clues for suspicion, particularly in cases of chest and neck injuries.
A chest X-ray might not show anything unusual in around 10% of patients where the tear hasn’t extended beyond a certain point or has sealed itself off due to a healing component known as fibrin. The most common place for this kind of tear to occur is where your windpipe splits into the lungs, an area that is more susceptible to shear stress. If the tear is within a particular layer of tissue, it could cause air to collect outside of the lungs in the mediastinum – a condition known as pneumomediastinum. If the tear extends beyond that point, it could lead to pneumothorax, where air collects in the space around the lungs, making it difficult for them to expand fully.
An injury to the airway leading to the right lung is likely to cause pneumothorax, whereas an injury to the left one is more prone to cause pneumomediastinum due to its longer course within the chest. In severe cases, the lung may even move to a different position in the chest due to detachment of the airway – this is known as the fallen-lung sign.
Other classic signs include placement of a breathing tube in an unusual position, overinflation of a breathing tube’s cuff, or persistent pneumothorax even after a tube has been placed between the ribs to remove excess air. However, the most specific signs of a tracheobronchial tear are the location of the breathing tube beyond the expected windpipe anatomy and the fallen-lung sign.
A CT scan is much more sensitive in identifying tracheobronchial injury and is the preferred non-invasive investigation. It can identify subtle findings like tiny pneumothoraces, emphysema in the mediastinum, and active bleeding in an injured airway. It can also detect air in the wall of the windpipe or airways, which can indicate a tear. In addition to this, the CT scan can helps in identifying critical injuries to the heart and major blood vessels. If the CT scan isn’t clear, a bronchoscopic assessment can provide more information.
While an MRI scan has benefits such as detailed imaging, less risk for kidney damage from contrast dye, and no radiation exposure, it can be offset by the need for preparation time, increased scan time, and the risk involved in monitoring unstable patients during the test. Additionally, not all facilities have an MRI machine.
Nuclear imaging won’t be helpful, particularly in minor injuries. However, angiography, an imaging technique that uses X-rays to visualize the blood vessels, could be useful to identify any associated vascular injuries, especially in cases where the tear is actively bleeding.
The gold standard for detecting a tracheal tear is the fiberoptic bronchoscopy. This procedure allows the doctors not only to diagnose the injury but also manage the airway safely in patients with suspected or confirmed tracheobronchial injuries.
Treatment Options for Tracheobronchial Tear
Emergency management of patients with suspected or confirmed injuries to the tracheobronchial (windpipe and main airways in the lungs) area typically involves establishing a secure airway, which is crucial for patients to breathe safely. Contrary to what might seem logical, patients with these types of injuries should avoid being intubated too quickly, a procedure where a tube is inserted into the windpipe to help with breathing. This common emergency procedure, called rapid sequence intubation, can cause further harm and even create a false passage if the airway is torn or damaged.
To manage such situations, healthcare professionals aim to promote spontaneous breathing for the patient, i.e., the patient is allowed to breathe on their own without assistance, until a safe airway is established. A procedure involving a fiberoptic bronchoscope, a fancy term for a flexible camera that doctors use to look into the patient’s airway, is often the best plan of action. This allows doctors to see the state of the airway clearly, insuring the breathing tube is placed safely. If the tear is low in the airway, single-lung ventilation could be started where only the healthy side of the lungs is ventilated.
However, this solution, while generally successful, may not work well if the patient is bleeding heavily, as this could make visualizing the airway difficult. Also, it requires the patient to be cooperative and calm, which might not always be the case in traumatic situations.
Sometimes, particularly severe injuries could require a surgical intervention. One such surgery, known as a tracheostomy, involves creating an opening in the neck to insert a breathing tube directly into the trachea or windpipe. This is typically performed if the injury completely severs the windpipe and voice box (the larynx) from each other.
The seriousness of the injury and other factors such as the patient’s overall health, age, and the nature of the tear determine what kind of treatment is best. While surgery is often necessary, in some cases, conservative management that includes spontaneous healing can be considered. However, this can sometimes lead to narrowed airways later on.
In recent years, a number of minimally invasive options have emerged for the management of tracheobronchial injuries. Using tiny incisions to access the area, these procedures are less intensive and can reduce the recovery time, making them particularly useful in high-risk patients or cases where the injury was caused by a medical procedure.
In all of these cases, once a safe airway is established, it’s crucial to check for injury to other nearby vital structures. These include the vocal cords, esophagus, spine, lungs, ribs, sternum (breastbone), clavicle (collarbone), arteries, veins, and major blood vessels in the neck. Severe injuries to these structures can affect a patient’s overall survival outcome. Therefore, ensuring their safety is paramount in managing tracheobronchial injuries.
What else can Tracheobronchial Tear be?
Conditions like pneumomediastinum, subcutaneous emphysema, and pneumothorax can occur due to injuries to different parts of the body such as the windpipe, lungs, esophagus, and vocal cords. Also, air can enter the chest cavity through external chest injuries or from the abdomen. Trauma related injuries, both blunt and sharp, can lead to damage in various areas in the neck and chest. This could include injuries to major arteries and veins, as well as the major trunk of the lung and nerves. These associated injuries could further lead to severe complications like:
- Shock
- Sepsis (infection in the blood)
- Pneumonia (lung infection)
- Atelectasis (collapse of part or all of a lung)
- Bronchiectasis (permanent enlargement of parts of the airways of the lung)
- Stroke
- Multiple organ dysfunction
All these complications can increase the risk of death in case of a tracheobronchial injury.
What to expect with Tracheobronchial Tear
The chance of recovery from tracheobronchial injuries (damage to your windpipe and main airways) depends on several factors. This includes the patient’s general health, how severe the injury is, when it was discovered, other injuries that happened at the same time, and the type of medical care they receive.
Sadly, around 80% of people with these injuries due to blunt trauma (sudden physical damage) pass away before they can get to a medical facility. This could be because they often have other injuries as well which are very serious by themselves. Thankfully, the survival rate for these injuries has greatly improved over time. Before 1950, the mortality rate was 36%, but this fell to 9% by 2001.
A 2009 study found that men had a higher risk of dying from these injuries. However, it’s thought that this might be more linked to the reasons they were struggling to breathe in the first place, rather than the injury itself.
Complications such as mediastinitis (infection of the area between your lungs), a delayed diagnosis, and receiving treatment when critically ill can increase the chance of passing away. In fact, the mortality rate is up to 80% for critically-ill patients receiving treatment. Patients should be carefully monitored for signs of stenosis (a narrowing of the airways) until their injury has fully healed.
The care of these patients can be expensive, as it involves regular check-ups. Some patients may need medical treatment using an endoscope (a flexible tube with a camera) for dilation (widening) exercises during these checks.
Possible Complications When Diagnosed with Tracheobronchial Tear
The complications from tracheobronchial tears, or tears in the windpipe, can vary based on the type and extent of the injury. About 80% of individuals suffering this injury due to a forceful impact die before even reaching the hospital, often due to other severe injuries sustained during the accident. Tracheobronchial injuries can have a wide range of symptoms, from subtle issues that barely show any symptoms to severe respiratory distress and breathing failure. In some cases, it may cause a sudden collapse of the windpipe. Other common symptoms and problems include skin swelling due to trapped air beneath the skin, air around the mediastinum (the central compartment of the chest), or a punctured lung. Furthermore, these injuries can lead to infections and sepsis that can impact multiple organs, thus increasing the risk of death. If these injuries are left to heal over time on their own, this could lead to bronchiectasis, a permanent enlargement of the airways, significantly reducing lung function.
Even injuries caused by medical treatment can result in problems with the esophagus and mediastinum, which can give rise to a life-threatening infection called mediastinitis. If untreated, these injuries may cause later narrowing of the airway. Injuries related to the pressure from an airway cuff can range from simple tears in the mucous membrane, which can progress to narrowing of the windpipe, or a hole forming between the windpipe and esophagus. Complications from a surgical repair of a tracheobronchial tear may include separation of the sutures, a lesion that forms on the brachial artery with sudden, deadly bleeding, narrowing of the airway, sores or openings, and changes to the voice due to nerve palsies. Reported problems with endoscopic management using a stent include infections, the stent moving out of place, narrowing of the windpipe due to granulation tissue, metal wearing out, and mucus formation causing a blockage.
Approximately 50% to 70% of tracheobronchial tears are not recognised at first and can later show up as breathing difficulty, stridor (a harsh or grating sound when breathing), and frequent infections. The rate of death is high in such cases that require surgery after initial injuries have been missed.
Common Complications:
- Death at or en route to hospital
- Respiratory distress or failure
- Sudden collapse of the windpipe
- Swelling due to trapped air beneath the skin
- Air around the mediastinum
- A punctured lung
- Infections, sepsis, and impact to multiple organs
- Bronchiectasis and reduction in lung function
- Esophageal and mediastinal injuries
- Mucous membrane tears, narrowing of the windpipe, hole between the windpipe and esophagus
- Separation of the sutures, life-threatening bleeding, narrowing of the airway, sores or openings, and voice changes
- Infections, stent moving out of place, narrowing of the windpipe due to granulation tissue, metal fatigue, and mucus blockage
Recovery from Tracheobronchial Tear
After surgery to fix a tracheal injury, the patient’s neck is kept in a specific position, known as the Pearson position (which involves keeping the neck bent forward), for about 7 to 14 days. This helps prevent the tissues from stretching. Furthermore, the inflated portion of the breathing tube, known as the cuff, should not press on the repaired area. To prevent potential infections, doctors also typically give patients antibiotics, as a precautionary measure, for at least one week.
Preventing Tracheobronchial Tear
Health care professionals, including paramedics, could help lower the death rates from windpipe-related injuries if they were more aware of advanced trauma care techniques. There is a way to lessen the severity of accidental windpipe and lung channel injuries; this can be achieved with suitable precautions and secondary support. Use of a specific type of cuff on breathing tubes – one that’s high in volume but low in pressure, can help reduce windpipe injury in patients who need assistance in breathing.
Proper training for professionals, using the right size of breathing tube, correctly using tools like stylets and boogies (thin, flexible rods used to guide the breathing tube), and avoiding over-filling the cuff of the breathing tube may all help lessen windpipe injuries during the process of inserting a breathing tube.
For tricky breathing tube insertions or when there’s a risk of injury to the windpipe and lung channels, using a tool called a fiberoptic bronchoscope can not only lessen further injury but also prevent creation of harmful false passages. Before removing the part of the esophagus due to cancer, it is crucial to use this fiberoptic bronchoscope to ensure that the cancer has not spread to the airways. Also, surgeons should exercise caution when using heat-producing devices close to the windpipe during head and neck surgeries.
Patients and their families should be well-informed about the possible immediate and long-term complications of windpipe-related injuries that could happen accidentally during medical procedures. Knowledge about the immediate and long-term complications of blunt or sharp windpipe injuries is also crucial. Preventive measures like improving car safety features, such as seatbelts and airbags; making helmet use mandatory while motorcycling or mountain biking; and providing mental health support to prevent suicide-related windpipe injuries also form part of a preventive strategy.