What is Neurapraxia?
In 1942, a person named Seddon came up with a way to categorize the damage that can happen to our nerves (Peripheral Nerve Injury or PNI). Seddon said there were three levels of this damage: neurapraxia, axonotmesis, or neurotmesis. Later, in 1951, Sunderland added on to this and made a five-degree system.
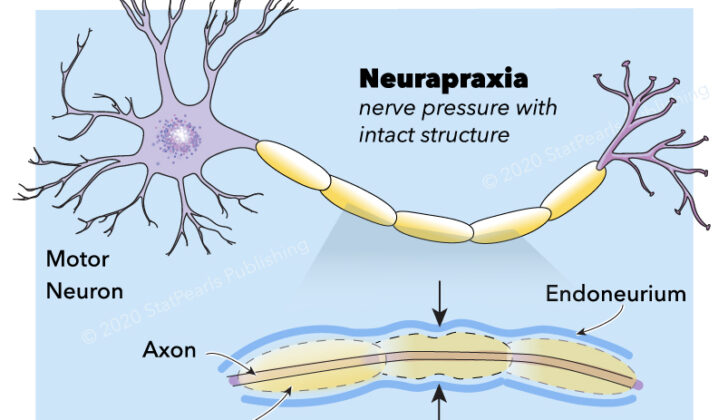
Neurapraxia is the most mild kind of nerve damage and is often caused by pressure on the nerve or an injury that temporarily cuts off its blood supply. According to Sunderland’s system, neurapraxia is grade 1, implying it’s the least severe. In neurapraxia, the injury causes a block in the nerve’s ability to send signals inside the injured area. This means that there could be partial or complete loss of feeling and movement. However, the main parts of the nerve remain intact.
Neurapraxia happens when the nerve’s outer protective layer is damaged. But if the nerve is activated further down from the injured area, it can still send signals. Normally, neurapraxia has a good outcome. The nerve is expected to repair itself and get back to normal within three months. This natural recovery can be tracked both by changes in the patient’s symptoms and by tests that measure the nerve’s ability to conduct electricity.
It is important to note that the term ‘neurapraxia’ is often used incorrectly in scientific papers. The term was first used by Seddon in 1942, so it is recommended that we continue to use the term correctly in scientific settings.
What Causes Neurapraxia?
Neurapraxia is a condition that can be caused by many things.
* Bone fractures can cause neurapraxia.
* Fractures of the humerus, the bone in your upper arm, can affect certain nerves and cause neurapraxia between 6-19% of the time.
* If you’re positioned incorrectly during anesthesia, it can affect nerves like the ulnar, brachial, radial, common peroneal, sciatic, peroneal, and great auricular nerves.
* A specific type of spinal surgery, known as transpsoas lumbar interbody fusion, can cause nerve problems and reduce strength in your thigh and hip muscles in about 2.6% of cases.
In a procedure called shoulder joint replacement, specific nerves can be affected about 21% of the time. This can happen because of a direct injury or the nerves being pulled too much during the procedure. Shoulder dislocation can also affect these nerves in 5-55% of cases. Other surgeries, like ones involving the thyroid or the spine, can also cause nerve injuries and lead to things like hoarseness or paralysis of certain areas.
High impact sports like football and rugby can cause neurapraxia, sometimes referred to as “burners” or “stingers,” in a significant number of players. After childbirth, or certain medical procedures like biceps tendon repair or regional anesthesia, nerve injury can occur in some patients.
A knee surgery called anterior cruciate ligament repair can cause injury to a specific nerve in the leg. Temporary nerve problems can occur after certain types of nerve blocks, while permanent problems are quite rare.
Finally, if a patient is not positioned correctly during anesthesia, it can cause complications like neurapraxia. This is often avoidable. The ulnar nerve, which runs down your arm, can be affected between 1 in every 215 to 1 in every 385 anaesthesia incidents. Most of these nerve injuries occur in patients who already had pre-existing nerve issues.
High-speed injuries, deep cuts, and trauma can also cause nerve damage.
Risk Factors and Frequency for Neurapraxia
Neurapraxia, a type of peripheral nerve injury (PNI), is not well documented, primarily because it’s often paired up with other PNIs. However, we do know that traumatic nerve injuries – which neurapraxia is a part of – affect about 350,000 people every year. These injuries are most commonly found in young adults between ages 20 and 39, with males making up 74% of cases.
During the conflicts in Iraq and Afghanistan, almost half of all nerve injuries were due to neurapraxia, specifically affecting the ulnar, common peroneal, and tibial nerves. In peaceful times, neurapraxia most often involves the upper body, with the ulnar nerve being affected 75% of the time, either alone or in combination with others. Some reports mention the radial nerve as the most commonly affected, followed by the ulnar and median nerves. The ulnar and median nerves are the ones most frequently involved in combined injuries. When it comes to lower body injuries, the common peroneal and sciatic nerves are usually the ones affected.
- The most common cause of PNI, including neurapraxia, is vehicular accidents (46.4%), usually involving young men.
- Other causes include penetrating trauma (23.9%), falls (10.9%), gunshot wounds (6.6%), pedestrians involved in car accidents (2.7%), sports-related incidents (2.4%), and other miscellaneous causes (7.2%).
- The prevalence of PNI is between 13 and 23 cases per 100,000 people each year.
Signs and Symptoms of Neurapraxia
Understanding how an injury took place is very important because it can help guide doctors on how best to treat it. After examining a patient, doctors can generally tell which nerve has been damaged. They should check both the sensory and motor functions to judge the extent of nerve damage.
Damaged nerves can result in motor problems such as weakened strength, slowed reflexes, or even muscle wasting in long-term cases. Sensory problems can include pain, heightened or decreased sensitivity to pain, and abnormal sensations like tingling or numbness. Typically, patients will have a mix of these symptoms, with motor issues being more noticeable.
If the nerve injury is complete, there will be a lack of any sensation in the area served by the nerve, and the muscles may become limp and unresponsive. If the injury is partial, some sensation or movement might still be present. If a patient exhibits a Tinel sign – a tingling sensation when a specific spot is tapped, it indicates some nerve signals are being conducted at the injury site.
Testing for Neurapraxia
Your doctor may order a series of tests including a complete blood count, blood sugar test, liver and kidney function tests, checking your erythrocyte sedimentation rate (a test that measures inflammation in your body), vitamin B12 levels, and thyroid-stimulating hormone (which controls the function of the thyroid).
To evaluate muscle and nerve function, a procedure called needle electromyography (EMG) may be conducted. EMG is best performed 2 to 3 weeks after the injury by stimulating the nerve and recording the resulting muscle response. It can determine the extent of the injury, and thus the likelihood of recovery.
There’s a particular muscle response referred to as Compound Muscle Action Potential (CMAP). If no CMAP is detected after nerve stimulation, it usually means a severe injury has occurred. In contrast, if small bursts of activity (Small-amplitude, short-duration motor unit potentials) are seen, it suggests excellent chances for recovery.
In a specific type of nerve injury known as neurapraxia, the EMG can show interesting results. In these cases, the test can help identify whether the problem is rooted in the nerves (neuropathic) or in the muscles (myopathic). If the origin is in the nerve, the muscle won’t show any spontaneous abnormal activity during the test. Eventually, with time and healing, the appearance of Motor Unit Action Potentials (MUAPs) can indicate that the nerve is starting to control the muscle again.
Imaging tests can also be helpful in the diagnostic process. An ultrasound can check the condition of the nerve, while a computed tomographic (CT) scan can reveal issues such as fractures or misplaced surgical hardware that might be causing nerve pressure.
In cases of trauma or post-surgery complications, Magnetic Resonance Imaging (MRI) of the lower back and pelvis should be done immediately to rule out any source of nerve compression. MRI can also provide detailed 3D images of nerve fiber bundles within the tissues, which can help assess nerve damage.
Treatment Options for Neurapraxia
Neurapraxic injuries, or minor nerve injuries, are typically cared for using a conservative or non-surgical approach. The main components of this method include using orthotic devices (like splints and supports for the affected limb), physical rehabilitation exercises, refraining from any activities known to worsen the condition, and medications designed to manage nerve pain. Such medications could include painkillers, antidepressants, anticonvulsants, corticosteroids, and numbing agents.
Doctors monitor progress through regular check-ups and electrical tests to evaluate if the nerve function is improving.
However, certain circumstances warrant urgent surgical intervention. For example, if the nerve injury arises from a build-up of blood due to internal bleeding (hematoma), or because of broken bone. In cases of ‘compartment syndrome’, where high pressure within enclosed muscle space is affecting the nerves, a surgery called a ‘fasciotomy’ is performed to release the pressure.
If there is still no improvement seen in terms of physical symptoms and electrical function after 3-6 months, it may be necessary to consider surgery. Sometimes, scar tissue can obstruct the healing process. In such a case, the surgeon can relieve pressure on the nerve or also move it to another location if necessary.
Rehabilitation is an essential part of recovery and involves providing not just physical support but mental and emotional support too. Pain management can be challenging with nerve injuries, as they often cause a distinctive burning feeling and abnormal sensations along the path of the nerve. To manage this pain, medications such as antidepressants, anticonvulsants, and drugs such as baclofen could be used. Short term use of nonsteroidal anti-inflammatory drugs, tramadol, and opioids can also be employed.
Key to the overall management plan is prevention, especially keeping an eye out for preventable causes of damage. It’s important to avoid repeat injury and persistent compression, as these can delay recovery or prevent complete recovery.
What else can Neurapraxia be?
Neurapraxia, a type of nerve and muscle disorder, can be confused with various other conditions. The following conditions should be remembered when examining patients with possible neurapraxia:
- Neurotmesis
- Axonotmesis
- Diabetic neuropathy (a type of metabolic disease)
- Inflammatory neuritis
- Infectious neuropathy, like HIV or leprosy
- Paraneoplastic neuropathy (associated with cancer)
- Hypothyroidism
- Alcohol-related conditions
- Malnutrition
- Radiculopathy (nerve root damage)
- Myelopathy (spinal cord injury)
- Spinal cord trauma
- Spinal cord infarction (lack of blood supply)
- Muscle diseases
- Upper neuron disease
It’s important to distinguish between these conditions as the method of treatment can vary.
What to expect with Neurapraxia
Neurapraxia, a non-nerve fiber damaging injury, usually has a really good outcome. Most people bounce back within two to three months. Younger folks tend to recover better, but there’s still a chance of permanent disability in about 30% of cases. And those with more severe injuries might need a longer break from work to fully recover.
If you’ve injured your ulnar nerve, which is in your arm, you should know that about half of people get better in six weeks. However, the rest might still have some problems after two years. In fact, people who injured their brachial plexus (a network of nerves that sends signals from your spine to your shoulder, arm, and hand) because of how they were positioned during anesthesia for surgery fully recovered in 82% of cases.
In terms of sport-related neurapraxia injuries, half of the athletes were back to their normal schedules in less than a week. But, about 9.4% of them ended up having to sit out for the whole season. For athletes, this kind of nerve injury (PNI) can impact when it’s safe for them to get back in the game.
Possible Complications When Diagnosed with Neurapraxia
Neurapraxia isn’t just a medical condition but can also significantly affect a person’s life. There are several complications associated with it.
- Pain linked to nerve damage (Neuropathic pain)
- Mental health problems (Psychological issues)
- Financial burdens (Economic losses)
- Muscle wasting due to wrong diagnosis (Muscle atrophy if incorrectly diagnosed)
Preventing Neurapraxia
The first step in managing neurapraxia, or temporary nerve damage, is prevention. Appropriate treatment and rehabilitation of these injuries can greatly enhance a patient’s health and wellbeing, as well as yield better results. It’s crucial that patients understand the importance of seeking medical help as soon as possible to determine whether there are causes that can be treated.
Patients may experience several weeks with no improvement in their sensory or motor functions, but they should still be encouraged to attend physical therapy and rehabilitation sessions. After about three months, they should see progress in their nerve recovery. Learning how to manage this condition effectively can lead to a more successful recovery and improve their quality of life.