What is Spinal Stenosis?
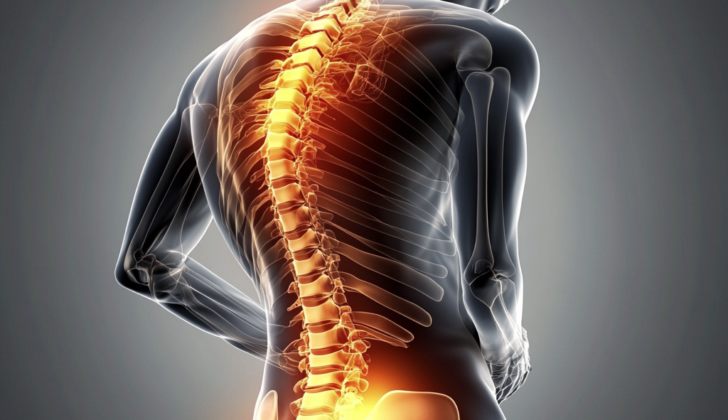
Spinal stenosis is a medical condition where the nerve roots within the spinal canal get squeezed by different unhealthy factors. This compression often results in symptoms like pain, numbness, and weakness. This typically happens in the upper neck (cervical) and lower back (lumbar) areas, but it can also occur in the thoracic spine (middle back), often due to a disk herniation.
In spinal stenosis, three specific parts within the spinal canal can be compressed. The first part is the central canal, where our spinal cord is located. This canal can become narrower, putting pressure on the nerves and lowering the blood supply to the spinal cord in the neck and the bundle of nerves at the bottom of the spinal cord (cauda equina) in the lower back area.
The second part affected is the neural foramen, which are small openings through which the nerve roots leave the spinal cord. Compression can occur here due to disk herniation, enlargement of the facet joints and ligaments, or unstable movement of one vertebra (backbone) with respect to the underlying one.
The final part is the lateral recess, an area in the lower spine where a nerve root enters just before its exit through the neural foramen. This area can also be compressed as a result of an enlarged facet joint.
Depending on which spinal area is affected, each type of compression can lead to different symptoms that need their own specific treatment.
Most patients experiencing spinal pain tend to recover eventually even without surgery. Only a small percent, around 1-3%, will have a herniated disc and less than 2% will deal with a compressed nerve root.
Spinal stenosis is common among older people, but it’s difficult to predict who will develop symptoms. In most cases, making lifestyle changes can help manage the degenerative process associated with this condition.
What Causes Spinal Stenosis?
Spinal stenosis, which is a narrowing of the spaces within your spine, can be caused by a number of different factors. Some of these causes are present from birth (congenital), but these only make up about 9% of cases. Some conditions someone could be born with that could lead to spinal stenosis include achondroplasia (dwarfism), an abnormally small length of certain bones in the spine, a bone disease called osteopetrosis, a bent spine, spinal dysraphism (faulty formation of the spine’s structure), early bone hardening in the spine, a curvature of the spine in the upper back area, Morquio syndrome (a rare genetic disorder that affects bone growth), and abnormal bone growths.
Spinal stenosis can also develop over time due to acquired causes. These include injury, wear and tear on the spine, certain medical treatments, and whole-body diseases. Injuries could happen for a number of reasons, but they generally involve a sudden force to the area. The spine can also become narrow if it wears down over time from things like a slipped disc, overgrown ligaments, and bones in the spine slipping out of place. Certain back surgeries, like removing a portion of a vertebra, fusing bones together, or removing a disc, can sometimes lead to a narrower spine. Systemic processes refer to diseases that affect the entire body and may also involve the spine.
Risk Factors and Frequency for Spinal Stenosis
In the United States, spinal stenosis is a common condition seen in outpatient clinics, particularly among older adults. Spinal stenosis in younger people is often due to birth defects, while in people over 50, it’s typically due to age-related degeneration. Studies have shown that approximately 1 in 1000 people over the age of 65 and about 5 in 1000 people over the age of 50 are likely to develop spinal stenosis. The number of people affected by this condition is expected to rise to around 18 million in the next ten years.
Lumbar spinal stenosis (LSS), a type of spinal stenosis, is the primary reason for spine surgery in adults over 65. As you move lower down the spine, the space available for the spinal nerves decreases. This narrowing increases the chance of foraminal stenosis, thereby leading to spinal stenosis.
Signs and Symptoms of Spinal Stenosis
Spinal stenosis is a condition that arises when the spaces in your spine narrow. This narrowing can cause a range of symptoms. The way these symptoms show up depends on whether the narrowing is happening in your neck (cervical spine) or lower back (lumbar spine).
Doctors usually start diagnosis by asking patients about symptoms and conducting a physical exam. In the case of cervical spine stenosis, symptoms are related to compression of nerve roots and the spinal cord itself. Initial signs typically include neck or arm pain.
If a nerve root gets squeezed, symptoms will vary based on which vertebrae are affected. Of those, some common symptoms associated with disk herniations include:
- C5-6 disk herniation: Weakness in forearm flexion and a tingling sensation in the thumb and radial forearm.
- C6-7 disk herniation: Leads to a drop in wrist function and numbness in the second and third fingers.
- C7-T1 disk herniation: Results in weakness in hand muscles and numbness in the fourth and fifth digits.
- C4-5 disk herniation: Can lead to weakness in the deltoid muscles and a tingling sensation in the shoulder.
Other symptoms can include pain and a tingling sensation in the head, neck, and shoulder. More intense symptoms such as clumsiness in upper limbs, changes in walking style, weakness in lower limbs, and balance issues may develop if the spinal canal narrows by more than 30%.
When stenosis occurs in the lumbar spine, a patient may experience leg cramps, calf or buttock ache, and symptom correction when sitting or leaning forward. As with the cervical spine, certain symptoms can be associated with disk herniations at specific levels:
- L5-S1 disk herniation: Weakness in the feet, decreased sensation in the lateral foot, and pain in the back of the leg.
- L4-5 disk herniation: Weakness leading to foot drop and numbness in the large toe web and top of the foot.
- L3-4 disk herniation: Weakness in knee extension, numbness in the medial foot, and pain in the front of the thigh.
Testing for Spinal Stenosis
If your doctor suspects a certain type of spinal disorder, they may use various imaging techniques to make a diagnosis. These techniques may include an extended-release x-ray, CT scan, or MRI scan.
The extended-release x-ray is not as commonly used anymore due to the availability of superior scanning techniques like the MRI. However, it can be useful in certain cases to show any movements or shifts in the spine that could point to instability or a condition called spondylolisthesis.
CT scans are beneficial for diagnosing a variety of spine conditions. These scans can help tell the difference between a hardened disc or bone spur and a “soft disc.” CT scans can also help identify if the longitudinal ligament is ossified (hardened with extra bone growth) or thickened and spot any fractures or areas where bone is being gradually destroyed.
Meanwhile, MRI scans are considered the gold standard in imaging for spine issues as they provide a detailed view of the spinal cord and surrounding structures. These scans can show abnormalities within the spinal cord itself, check the extent of spinal stenosis (a narrow spinal canal), and distinguish other health problems like tumors, blood clots, or infections.
However, if a patient has a pacemaker, an MRI may be off the table. In such cases, a variant of the CT scanning technique, called a CT myelogram, can be performed instead. This technique includes injecting a contrast dye to provide a clearer picture of the spinal canal and identify any narrowing or other abnormalities.
To further support diagnosis, the doctor may perform electrodiagnostic studies. These involve procedures such as nerve conduction tests, needle electromyography (a test that measures electrical activity in your muscles), and somatosensory evoked potentials (which analyze the nerve pathways related to sensory function). These tests can help confirm the diagnosis and rule out other similar conditions.
Treatment Options for Spinal Stenosis
If you have cervical stenosis, which is a narrowing of the spinal canal in your neck, but it’s not severe enough to affect your spinal cord (a condition called myelopathy), usual treatments include wearing a brace, resting, or taking anti-inflammatory medications. However, if the stenosis has led to myelopathy, which can cause pain and a loss of sensation, a surgical procedure that relieves the pressure on your spinal cord (decompression) may help.
Decompression surgery, in this case, might remove some of the bone or tissue causing the pressure or it might be done in combination with a fusion surgery that joins two or more of your neck bones together for stability. It can be performed from the front of your neck (anterior) or the back (posterior), depending on the specifics of your situation.
If you’re experiencing back pain due to issues in your lower back (lumbar spine), initial treatment may involve anti-inflammatory medication and physical therapy, followed by procedures to manage the pain if it continues. However, if these methods aren’t helping, or if your condition worsens, causing neurologic deficits like numbness or weakness, or spinal instability, you might need decompression and fusion surgery like in the case of cervical stenosis.
The surgical approach may also vary, including an anterior (front), lateral (side), or posterior (back) method. The choice depends on the nature of your specific condition. These surgeries aim to restore the normal curvature of the lumbar spine (lordosis), alleviate the narrowing of the spinal canal (stenosis), and induce the joining of the affected bones in the spine (fusion).
What else can Spinal Stenosis be?
- Lumbar Compression Fracture
- Lumbar Degenerative Disk Disease
- Lumbar Facet Arthropathy
- Lumbar Spondylosis
- Mechanical Low Backpain
- Rehabilitation for Osteoarthritis
- Rheumatoid Arthritis
- Spondylodiskitis
- Spondylolisthesis Imaging