What is Superficial Siderosis?
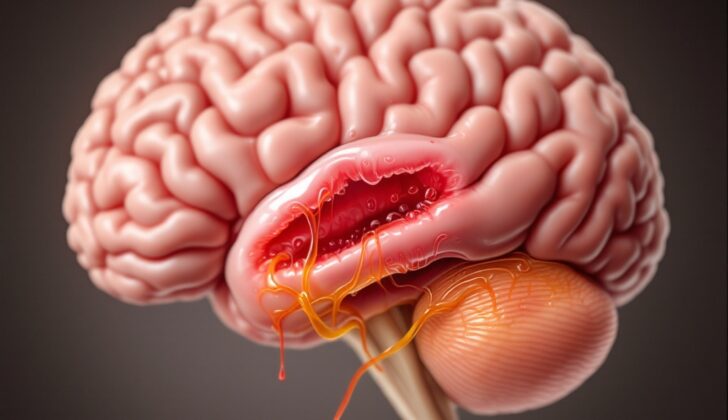
Superficial siderosis of the central nervous system is a long-lasting condition caused by continuous or repeated bleeding into the space surrounding the brain and spinal cord. This leads to the build-up of iron-rich protein called hemosiderin. This is a slow-moving condition that eventually damages the nerves and can greatly affect someone’s daily life. Most people with this condition do not have a history of a certain type of bleeding in the brain called a subarachnoid hemorrhage. However, previous injuries and surgeries involving the brain and spinal cord may increase the risk of getting superficial siderosis.
This condition can be grouped by the parts of the brain it affects, which can be divided into two types: cortical and infratentorial. There are multiple health problems that can cause superficial siderosis, and they vary depending on the type. Cortical superficial siderosis is usually caused by iron deposits in the outer layer of the brain due to bleeding from small vessels along the surface of the brain. This is often linked to a condition known as cerebral amyloid angiopathy, mostly seen in people who are 55 or older. The most typical cause for the classic or primary infratentorial superficial siderosis, also known as iSS, is defects in the covering of the spinal cord, often due to tears. Usually, the bleeding comes from delicate, leaking veins around the area of the tear. Secondary iSS could arise from injuries, surgery on the brain or spinal cord, tumors, or blood vessel issues. Surprisingly, in about 35% of cases, the cause of superficial siderosis remains unknown.
People with superficial siderosis might have no symptoms at all, but they usually experience unsteady walking, spinal cord disease, or hearing loss in different combinations. Symptoms associated with the part of the brain that controls movement and balance are mandatory, while signs of dysfunction of the facial nerves and spinal cord nerve roots are not always present. A diagnosis can be made when the characteristic iron-rich protein deposits are spotted on a special type of brain or spinal cord scan known as magnetic resonance imaging (MRI), particularly with sequences called gradient-echo (GRE) and susceptibility-weighted imaging (SWI).
What Causes Superficial Siderosis?
Depending on their classification, the causes of bleeding in the brain can differ. There are two main types: cortical superficial siderosis (cortical SS) and infratentorial superficial siderosis (iSS).
Cortical Superficial Siderosis
Cortical SS usually happens because of iron build-up in the outer layers of the brain following a bleed from small vessels within the membranes covering the brain (leptomeningeal vessels). This is most often seen in people over 55 due to cerebral amyloid angiopathy, which is a brain condition related to the build-up of a protein called amyloid. Other causes can include syndromes that narrow blood vessels in the brain, inflammation of blood vessels, injury, radiation, blood clots in brain veins, treatments that target amyloid proteins, or abnormal blood vessels.
Infratentorial Superficial Siderosis
iSS can be divided into two subtypes – classic and secondary (based on whether the bleeding was spontaneous or due to an injury). The most frequent cause of classic or primary iSS is a defect in the spinal dura, which is the outermost layer covering the spinal cord. These defects are often tears, frequently caused by bony outgrowths or calcified disc herniation.
iSS can also be caused by a connective tissue disorder resulting in the enlargement of the membranes covering the spinal cord (dural ectasia), traumatic nerve root avulsion (where a nerve is torn away), or a collection of cerebrospinal fluid that leaks out of the brain or spinal column after surgery (known as pseudomeningocele), leading to decreased pressure within the skull.
The most common source of bleeding in iSS is from delicate, leaky bridging veins, especially around dural tears. Secondary iSS can come from injuries, surgery of the head or spine, tumors, or abnormal blood vessels. In about 35% of superficial siderosis cases, the cause is unknown.
Risk Factors and Frequency for Superficial Siderosis
Superficial siderosis is a health condition that impacts all races and ages, but men usually experience it more than women. It’s not known why men are more prone to it, but it might be due to them being more susceptible to injuries to the head. Usually, people start seeing signs of superficial siderosis between their 40s and 60s, but it can show up at any age depending on the cause.
A study done by the Mayo Clinic showed that 0.21% of people aged 50 to 69 and 1.43% of people over the age of 69 have superficial siderosis. The number of people diagnosed with this condition has been going up over time because of the broader use of MRI scans and specific techniques that can detect iron.
- Superficial siderosis affects all races and ages.
- Men are more likely to get it than women.
- The cause for its higher prevalence in men might be due to more frequent head injuries.
- People usually start showing symptoms of superficial siderosis between the ages of 40 and 60.
- However, it can occur at any age, depending on the cause.
- According to a study by the Mayo Clinic, 0.21% of people aged 50 to 69 and 1.43% of people older than 69 have this condition.
- The number of diagnosed cases has been increasing because of the use of MRI and specific techniques that detect iron.
Signs and Symptoms of Superficial Siderosis
People who have inertial superficial siderosis (iSS) often show symptoms in their 40s to 60s. It can take many years after the onset of superficial siderosis for symptoms to start showing. In some cases, people have experienced a gap of 19 years between the inciting event and the appearance of their first symptoms. Usually, the first symptoms begin to show at least six months after a subarachnoid hemorrhage caused by an injury. iSS is rarely acute.
Hearing impairment is the most common symptom of iSS, often accompanied by a slow, progressive loss of motor control, or cerebellar ataxia. Cerebellar ataxia and deafness both occur in 90% of cases. Progressive sensorineural hearing loss, common in iSS, can lead to complete deafness in 1 to 12 years and is often accompanied by tinnitus and bilateral peripheral vestibular loss. Hearing loss is typically bilateral but asymmetric, and it usually affects high tones. The classic triad symptoms of superficial siderosis are hearing loss, ataxia, and myelopathy, but it’s rare for a patient to have all these symptoms at once. Gait ataxia is usually more common than appendicular ataxia.
Myelopathy, which involves spinal cord conditions, can present as pyramid signs, sensory symptoms, bladder dysfunction, and spasticity. Cerebellar signs, cranial nerve dysfunction, and myeloradiculopathy are also possible symptoms. Other possible symptoms include nystagmus, saccadic dysmetria, kinetic tremor, and cerebellar dysarthria.
Patients may have mild cognitive impairment, reduced sense of smell, headaches, and seizures. Cognitive impairment in superficial siderosis follows a distinct pattern, showing deficits in areas like executive function, visual recall, and speech production. This impairment is caused by iron-containing dark pigment, hemosiderin, depositing in the medial and inferior frontal cortex. It’s important to note that there’s no direct correlation between the extent of hemosiderin deposition and the severity of cognitive impairment.
In rare cases, patients diagnosed with superficial siderosis may also experience seizures, uncommon nerve palsies, optic neuropathy, and trigeminal neuropathy. For patients with superficial siderosis due to dural defects, symptoms of intracranial hypotension caused by a cerebrospinal fluid (CSF) leak might occur but don’t usually dominate the clinical presentation.
Older patients aged 60 and above, diagnosed with cortical superficial siderosis which is primarily due to cerebral amyloid angiopathy, often present chronic memory impairment or transient focal neurological episodes, colloquially termed as “amyloid spells”.
Testing for Superficial Siderosis
If you are experiencing symptoms that could suggest a condition called superficial siderosis, your doctor will want to take a detailed look at your medical history. They’ll pay attention to any past events, including surgeries, injuries, or conditions, which may have caused bleeding in your head. Superficial siderosis develops slowly, which means even old incidents that seem irrelevant may be important.
In the past, doctors had to rely on biopsies and autopsies to diagnose superficial siderosis. Nowadays, this disease is usually diagnosed through a type of brain scan called an MRI, specifically with special sequences like SWI or GRE that can identify the presence of a protein called hemosiderin. An MRI can show the extent of the disease and help pinpoint the source of any bleeding. This is not only helpful in diagnosing the condition but can also guide your doctor on the right treatment approach.
In some cases, an MRI with contrast, a dye that makes certain tissues, vessels, or diseases stand out, might be performed. This can suggest a tear in the durous membrane surrounding the brain and spinal cord or a significant drop in cerebrospinal fluid pressure. MRI contrast also helps identify blood vessels disorders or masses. On your MRI, you might hear your doctor talk about things like hypointensity, which means areas where the MRI signal is darker than normal. They could also mention something called “pencil”-like hypointensities or characteristic linear bands, which are specific features seen in this condition.
Superficial siderosis typically affects the cerebellum and brainstem. A CT scan (another type of imaging test that takes detailed pictures from different angles using X-rays) can show if there is a shrinkage of the cerebellum. In some cases, it may even show signs of damage to your spinal cord or signs of inflammation due to the presence of blood in the subarachnoid space, which is the area between the brain and the skull.
However, if the cause of the superficial siderosis is evident during the initial MRI with contrast, no further imaging is required. If the MRI doesn’t provide enough information, your doctor might recommend a CT or MR myelogram. This test involves injecting contrast dye into your spinal canal to get detailed pictures of your spinal cord and nerves.
In addition to imaging tests, you might need a lumbar puncture, where a small amount of fluid is drawn from your spinal canal for testing. This can provide more information about the disease. A high number of red blood cells in this fluid could suggest active bleeding, although a normal result doesn’t rule out superficial siderosis.
Lastly, your doctor might consider using artificial intelligence and advanced machine learning techniques for better detection and understanding of the disease. These innovative technologies could potentially provide new ways to identify and track the progression of superficial siderosis.
Treatment Options for Superficial Siderosis
Superficial siderosis is a condition that slowly affects the nervous system. The treatment largely depends on what’s causing the condition. In some cases, the root cause is a flaw in the dural, a protective covering of the spinal cord and brain. If a defect in the dural is detected, medical professionals recommend treatment, regardless if the patient is showing symptoms or not due to the potential for neurological damage.
The dural defect is typically spotted using a special type of X-ray known as CT myelography. To repair the defect, doctors can choose to suture, patch it, implant muscle or fat grafts or use a type of adhesive called fibrin glue. Other options include minimally invasive procedures or blood patches. Special instruments like spinal endoscopes and ultrasound used during surgery can aid in finding and managing defects in the dural.
Once the dural defect is repaired, tests such as CSF (cerebrospinal fluid) xanthochromia, which analyzes the color of spinal fluid, and checking for fluid collection around epidural area are used to confirm the success of the repair. It’s important to note that even after repairing the dural defect, symptoms of superficial siderosis often do not improve, but the repair can prevent the condition from worsening. Regular follow-up is therefore necessary even after successful treatment.
If the superficial siderosis is caused by other issues like abnormal blood vessels, amyloid accumulation in the brain, issues with blood supply to the brain, blood clot in cortical vein, and tumors in the central nervous system, the therapeutic approach will focus on treating these specific conditions to reduce bleeding into the space surrounding the brain and spinal cord. However, in most cases, the true cause of superficial siderosis may not be identified and symptoms may not be reversed upon treatment. In such cases, supportive care can help the patient avoid falls and further injury. Offering physical and occupational therapy can be beneficial especially for patients navigating walking issues, pyramidal symptoms, and balance problems.
Hearing loss is a common symptom of superficial siderosis, which usually worsens and cannot be reversed. Some patients may find benefit with cochlear implants, a device that can help provide a sense of sound to a person who is profoundly deaf or severely hard of hearing. However, because results can vary and hearing may decline due to the progression of superficial siderosis, patients are advised about the potential drawbacks before proceeding.
Chelation therapy, a procedure to remove excess iron in the body, has been explored as a treatment option because iron deposition in the brain is the root cause of superficial siderosis. Iron chelating drugs like deferiprone can lessen iron content in the body and on brain MRI scans. Though iron decrease in the body doesn’t correspond with clinical improvement and severity of the condition. Therefore, chelating therapies are currently not recommended for patients with superficial siderosis as they are shown not to give significant benefit.
What else can Superficial Siderosis be?
Superficial siderosis, a slow-progressing condition that affects the nerves, can be sometimes be tricky to diagnose due to the variety of symptoms it presents. Various health conditions can share symptoms with superficial siderosis and need to be considered before making an accurate diagnosis.
Some diseases with symptoms similar to superficial siderosis include:
- Parkinsonism – Due to the long-term progression and problems linked to walking and coordination
- Acoustic neuroma or vestibular schwannoma – These can also cause progressionhearing loss and balance problems
- Normal pressure hydrocephalus (NPH) – This condition can also manifest through progressive walking abnormalities. It can be tricky to distinguish between NPH and superficial siderosis as both could cause bladder incontinence.
- Vestibular neuritis – Often appearing after a viral illness, it presents over a relatively short span of time rather than chronically
- Meniere disease – Similar to superficial siderosis due to the chronic nature and extent of hearing loss. However, it manifests as unilateral low-frequency hearing loss as opposed to bilateral, high-frequency hearing loss found in superficial siderosis.
Once a brain scan is obtained, it becomes significantly easier to tell apart superficial siderosis from NPH, the former shows hemosiderin deposits while the latter presents enlarged ventricles.
Besides these conditions, there are also other conditions that might appear similar to superficial siderosis in brain scans including:
- Meningioangiomatosis
- Neurocutaneous melanosis
- Motor neuron disease like amyotrophic lateral sclerosis (referred to as the ‘snake eye sign’)
What to expect with Superficial Siderosis
The future health of a patient often depends on whether the doctors can identify and treat the cause or source of the bleeding. However, even if the source is identified and treated, it’s unlikely that the patient’s symptoms will fully go away. Despite treatment, the patient might continue to progress towards permanent disability.
This is usually due to a situation called “hemosiderin-induced irreversible neurodegenerative cascade”. Let’s break down what that means. “Hemosiderin” is a kind of iron storage complex – it’s what your body uses to keep iron when it’s not currently being used. Sometimes, under certain conditions, this can cause a domino effect where more and more brain cells become damaged which is the “neurodegenerative cascade”. This process isn’t likely to reverse itself once it’s started.
However, a specific kind of issue—spinal longitudinal intrathecal collections—has a better outcome. These are abnormal fluid-filled spaces in your spinal cord that can cause various symptoms. If the leak of the spinal fluid (also known as cerebrospinal fluid or CSF) is sealed or stopped, this could potentially halt and even improve symptoms. However, how well the patient does over time is strongly influenced by how long they have had these symptoms without treatment.
According to studies, the possibility of developing a condition called superficial siderosis after the CSF leakage varies over time. Superficial siderosis is a rare neurological disorder where hemosiderin – that iron storage complex we mentioned earlier – deposits along the surface of the brain and spinal cord which causes damage over time. The chance of this happening ranges from 0% at 4 years (48 months) to about 33% at 12 years (144 months).
In terms of aiding hearing impairments, cochlear implants — a type of medical device that converts sound into electrical signals which stimulate the hearing nerve— have varying degrees of success.
Possible Complications When Diagnosed with Superficial Siderosis
Superficial siderosis, a condition related to iron accumulation in the brain, can lead to various serious health issues. These issues often include hearing loss, balance problems that cause falling, and trouble walking. Other complications are losing sense of smell, brief neurological disturbances similar to stroke-like attacks, memory loss, sensory problems, urinary incontinence, and problems with cranial nerves functioning.
Worsening of the condition, called cortical superficial siderosis, can increase the risk of symptomatic brain bleeding. It is also strongly linked to amyloid angiopathy (abnormal deposition of proteins in brain blood vessels) and Alzheimer’s disease.
A treatment approach called deferiprone chelating therapy can lead to a severe complication known as agranulocytosis, which is a severe deficiency in a certain type of white blood cells. It’s alarming to note that 25% to 40% of patients treated with this method have had to stop treatments due to a life-threatening infection related to low white blood cell counts.
Notable complications:
- Hearing and balance problems leading to falls
- Trouble walking
- Loss of sense of smell
- Transient neurological episodes mirroring stroke-like attacks
- Memory loss
- Sensory problems
- Urinary incontinence
- Cranial nerve dysfunction
- Risk of symptomatic brain bleeding
- Links to amyloid angiopathy and Alzheimer’s disease
- Agranulocytosis linked to deferiprone chelating therapy
- Withdrawal from chelation treatment due to life-threatening infection
Preventing Superficial Siderosis
The main methods to stop and prevent a condition called superficial siderosis focus on dealing with the root causes that lead to continuous bleeding in the space around the brain and spinal cord, known as the subarachnoid space. This means carefully managing health issues that make a person more likely to have such bleeding, like injuries to the head or spine, tumors, and abnormal blood vessel formations. Taking steps to stop the bleeding from happening again, like keeping close watch and control over blood vessel lesions or tumors, can greatly lessen the chance of iron build-up and following nerve damage.
It’s also important to raise healthcare professionals’ awareness about the possible brain and nerve complications of a brain bleed, known as a subarachnoid hemorrhage. Prompt medical intervention can help diagnose and treat the condition early, therefore reducing the worsening of superficial siderosis and improving the patient’s health outcome. There are still many cases where the condition is not diagnosed or treated well. Because of this, a detailed health history and physical exam is crucial.
Doctors should think about superficial siderosis in patients who show gradual problems with balance and walking. Hearing loss can be hard to diagnose due to the older average age of patients with superficial siderosis and the usual hearing loss related to aging. Balance and walking issues are often mistaken as being due to age-related muscle weakness. This shows how important a complete physical exam is, with special attention to cerebellar function (coordination and balance control) and muscle strength. Symptoms like falling and loss of smell, may mistakenly point doctors to think of nerve degenerating diseases. A brain MRI with specific features for iron is key for a quick diagnosis and managing symptoms.
People with superficial siderosis should be made aware that their disease will get progressively worse and that the chances of full recovery are low. It’s important to have a team of different specialists working together to take the best care of patients with superficial siderosis. This team includes the patient’s audiologist, primary care doctor, physical therapist, occupational therapist, and neurologist.