What is Acute Subarachnoid Hemorrhage?
A subarachnoid hemorrhage (SAH) is a medical condition that happens when there’s a rupture in the blood vessels of the brain or due to a serious head injury. SAH takes place in a specific area within the brain, between the arachnoid membrane and the pia mater. The typical symptom of SAH is a sudden and severe headache, often described as “thunderclap-like”. However, only about 10% of people who go to the emergency room with a headache actually have an SAH. They may also experience other symptoms such as neck pain, nausea, vomiting, and sensitivity to light. SAH is generally a grave medical emergency that can lead to death or serious health issues among survivors.
What Causes Acute Subarachnoid Hemorrhage?
Around 85% of Subarachnoid Hemorrhage (SAH), a type of non-traumatic stroke, is caused by a ruptured aneurysm (a balloon-like bulge in a blood vessel) in a part of the brain known as the Circle of Willis. Other triggers for this condition could be drug abuse (particularly cocaine and amphetamines), hidden trauma, malformed or irregular blood vessels, inflammation of blood vessels, arterial dissections in the brain, certain bleeding disorders, sickle cell anaemia, or disorders related to the thinning of blood.
Having a family history of SAH can increase your risk, even if you don’t have any of these conditions. First-degree relatives (like parents, siblings, or children) of patients with SAH are found to be 3 to 5 times more likely to experience SAH than people in the general population. When cerebral aneurysms (brain aneurysms) are present in such families, these aneurysms have a higher chance of rupture. As a result, those with two or more first-degree relatives with SAH are recommended to go through preventative screening.
Some cases of SAH are linked to genetics. The genetic link seems to be diverse, involving multiple chromosomes. In some families, SAH seems to be passed down in a dominant manner, meaning only one parent needs to pass the gene on. In other cases, it could be passed down in a recessive manner (needing genes from both parents) or due to multiple genetic and environmental factors. Certain inherited conditions like polycystic kidney disease, a condition where glucocorticoids can fix high blood pressure (aldosteronism), and Ehlers-Danlos syndrome, also increase the risk of SAH. Around 8% of patients with polycystic kidney disease may also have brain aneurysms. So, if even one family member with this disease has a history of a ruptured aneurysm, it’s crucial for the patient to get screened.
Risk Factors and Frequency for Acute Subarachnoid Hemorrhage
Spontaneous cerebral bleeding, or SAH as doctors call it, occurs in about 1 out of 10,000 people every year. It’s more common in women and usually happens more as people get older, although more than half of the people with SAH are younger than 55. Certain habits or conditions can increase your risk of getting SAH, such as smoking, high blood pressure, and drinking a lot of alcohol.
About 10% of people report that they were doing something physically challenging, like bending over or lifting something heavy, when they first noticed their SAH symptoms. The main factors that increase your risk for SAH include high blood pressure, smoking, and having a family history of the condition. Other things that might raise your risk include using certain types of drugs, having low estrogen levels, and undergoing treatment to prevent blood clots.
- Spontaneous cerebral bleeding occurs in about 1 out of 10,000 people every year.
- It’s more common in women.
- More than half of people with this condition are under 55, but it becomes more common with age.
- Smoking, high blood pressure, and heavy drinking can increase your risk of getting SAH.
- Some people were doing strenuous activities when they first noticed their symptoms.
- High blood pressure, smoking, and a family history of the condition are the most common risk factors.
- Other risk factors for SAH include certain drug use, low estrogen, and treatment to prevent blood clots.
Signs and Symptoms of Acute Subarachnoid Hemorrhage
Subarachnoid hemorrhage (SAH) is a medical condition that typically presents with a sudden, intense headache that reaches maximum severity almost immediately. This is often accompanied by a stiff neck, vomiting, and a loss of consciousness. Additional symptoms can include one-sided weakness, or in some instances, seizures.
The pain typically radiates pulsating waves toward the back of the head. Seizures are more common in cases where an aneurysm is the cause of the SAH, and having a history of seizures often points towards an abnormal connection between arteries and veins in the brain. A stiff neck is a common symptom but it usually doesn’t appear until around six hours after the onset of the SAH.
Unequal pupil size and a lack of response to light can indicate severe brain swelling due to increased pressure within the skull. A condition known as Terson syndrome, where there is bleeding in the eye’s vitreous humor, can occur in 3% to 13% of SAH cases. This increased pressure in the skull can lead to a surge in stress hormones causing high blood pressure, heart rhythm problems, or even a cardiac arrest.
There might be changes in the heart’s electrical activity, including unusually large U-waves, T-wave abnormalities, QT prolongation, Q waves, high R-waves, irregular heart rhythm and fluctuations in the ST segment. Pulmonary edema may also occur if fluid leaks into the air spaces in the lungs due to elevated pressure within the pulmonary circulation. Risk factors for SAH include a previous head injury, known history of a brain aneurysm, high blood pressure, smoking, family history, connective tissue disorders, and abuse of drugs or alcohol.
- Sudden, intense headache reaching maximal severity immediately
- Stiff neck
- Vomiting
- Loss of consciousness
- One-sided weakness
- Seizures (occasionally)
- Pulsating pain radiating toward the back of the head
- Unequal pupil size and lack of response to light
- Condition involving bleeding in the eye (Terson syndrome)
- Heart rhythm problems
- Pulmonary edema
In some cases, patients may have experienced a warning sign in the form of a severe headache and/or a minor bleed with resolving symptoms within the past month. This is referred to as a sentinel bleed, a potential sign of a more serious SAH on the horizon. Diagnosing a headache from a sentinel bleed is extremely challenging.
A physical examination may reveal an issue with eye movement, which could point to the source of the bleeding. If there is irritation in the meninges due to the SAH, the patient may demonstrate neck stiffness. In this situation, the patient may also test positive for two signs: Kernig sign (unable to fully straighten the knees when the thigh is flexed at the hip and knee at 90-degree angles), and Brudzinski sign (hip and knee bend when the neck is passively flexed).
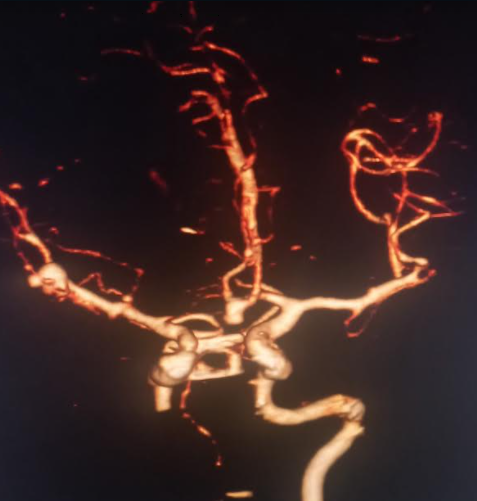
cerebral artery bifurcation.
Testing for Acute Subarachnoid Hemorrhage
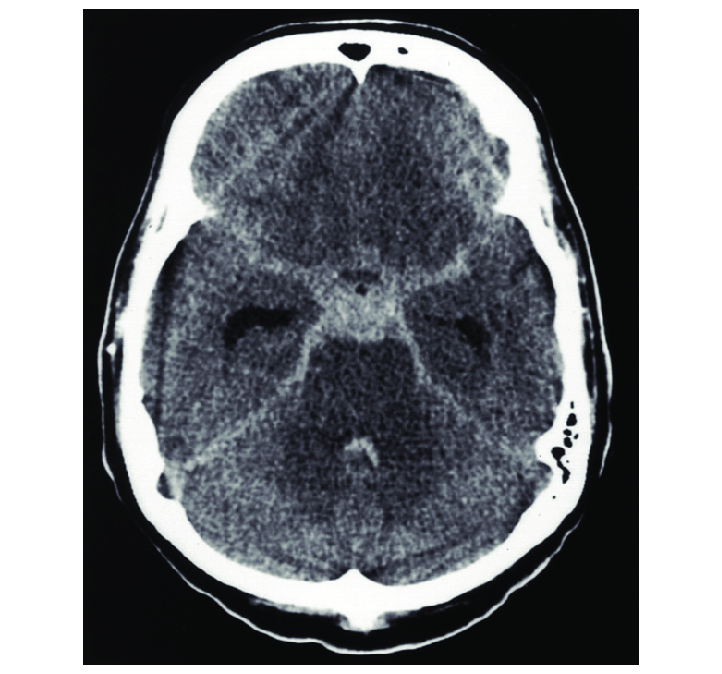
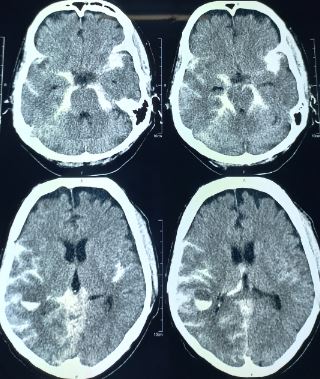
When someone may have a brain issue like a subarachnoid hemorrhage, doctors generally perform a head CT scan without contrast. This test can detect nearly all cases within 6 hours of the issue occurring. However, as more time passes, an MRI may be more sensitive and helpful for detection. If the CT scan doesn’t provide a clear answer or if it’s been longer than 6 hours since the issue’s onset, a doctor might decide to do a lumbar puncture, which is a way of testing the fluid around the brain and spine. Though this test can sometimes reveal evidence of a bleed in the brain even when a CT scan doesn’t, it has some risks and could lead to extended stays in the emergency room. Doctors need to discuss these risks with their patients and make decisions together.
Laboratory tests play an essential role in the diagnostic process. For example, consistently high numbers of red blood cells in all samples of cerebrospinal fluid (the fluid around the brain and spine), can indicate a subarachnoid hemorrhage. You can also test this fluid for xanthochromia or check for the presence of bilirubin to confirm a subarachnoid hemorrhage. However, it’s worth noting that this method only becomes reliable 12 hours after the brain bleed because it takes that long for hemoglobin to break down. Cerebral angiography or CT angiography can help identify the bleeding source.
Several different scales and classification systems have been developed over the years to evaluate how severe a subarachnoid hemorrhage is, both based on symptoms and what the head CT scan looks like. They also help predict how patients will fare and what the best course of treatment might be.

Treatment Options for Acute Subarachnoid Hemorrhage
Surgical treatment of brain aneurysms was first introduced in the 1930s. By the 1990s, less invasive procedures like coiling and clipping started to become popular for patients with a type of stroke known as subarachnoid hemorrhage (SAH). Research has found that smaller aneurysms, or those that have never bled before, are less likely to cause an SAH, and may not need surgery as a preventive measure.
If someone experiences an SAH, the first step is to make sure the patient is stable, which involves an urgent check by a brain surgeon. Intubation, or placement of a breathing tube, may be required for patients with a significantly altered state of consciousness. Blood pressure, heart rate, breathing rate, and consciousness level should all be monitored frequently. Medications for pain and nausea are usually necessary to control symptoms.
After an SAH diagnosis, most patients are usually taken to a specialized intensive care unit for brain surgery because there’s a risk that the bleeding could worsen. If the patient’s condition is severe or if brain imaging shows an increase in the size of the brain’s fluid-filled cavities, a drainage tube may be placed in the brain to relieve pressure.
Patient’s with larger blood collections, altered consciousness or any other new neurological symptoms, may require surgery to remove the blood and/or stop the bleeding site. If a brain aneurysm is found through angiography, a method of visualizing blood vessels, it can be treated through clipping or coiling to prevent further bleeding. Clipping requires opening the skull to place a clip around the base of the aneurysm. Coiling is a less invasive technique where coils are placed within the aneurysm through a catheter inserted in a blood vessel in the leg.
The most appropriate treatment method often depends on the location of the aneurysm. One study found that an endovascular coiling has better outcomes for certain aneurysms than clipping, while being aware of a slightly increased risk of aneurysm recurrence. Therefore, it’s recommended that these patients undergo periodic follow-up imaging.
Certain factors increase the risk of rebleeding, these include high blood pressure, blood collection in the brain or fluid-filled cavities of the brain, poor initial clinical condition, aneurysms in the back of the brain, and any aneurysms larger than 10 mm. Blood pressure control is crucial to prevent rebleeding. Certain medications, such as calcium channel blockers, can help prevent blood vessel constriction, which can lead to brain tissue damage due to decreased blood flow. This condition usually presents with new neurological symptoms and can be diagnosed with specific brain imaging procedures.
Up to one-third of patients with SAH experience vasoconstriction, and of these, about half suffer from lasting complications. The calcium channel blocker nimodipine can improve patient outcomes when administered within a specific timeframe after bleeding from an aneurysm in an SAH. However, it hasn’t shown to improve long-term outcomes in traumatic SAH, and is therefore not recommended in these cases.
What else can Acute Subarachnoid Hemorrhage be?
When trying to diagnose the cause of a sudden subarachnoid hemorrhage, which is like a severe brain bleed, doctors may consider several other possible conditions that may cause similar symptoms:
- Meningoencephalitis, an infection leading to inflammation of the brain
- Cluster headaches, which are highly painful headaches that can occur several times a day
- Adult seizures, or unexpected changes in behavior, movement, or sensation caused by abnormal brain activity
- Intracranial hemorrhage, another type of brain bleed
- Ischemic cerebrovascular accident, or what’s more commonly known as a ‘stroke’, caused by lack of blood supply to a part of the brain
- Migraine, a recurring type of headache often characterized by severe throbbing pain on one side of the head
- Transient ischemic attack, often referred to as a ‘mini-stroke’, where blood flow to part of the brain is temporarily blocked
These possible conditions require careful evaluation by the doctor to ensure a precise diagnosis and treatment plan.
What to expect with Acute Subarachnoid Hemorrhage
Subarachnoid hemorrhage, also known as SAH, unfortunately tends to have negative consequences. Approximately half of patients with SAH, which is often caused by an aneurysm, pass away within 30 days. Additionally, even those who survive the initial 30 days are not completely safe, as a third of them manage to develop complications.
About half of SAH patients suffer from neurocognitive impairment, which means that it affects their thinking abilities and quality of life. Over 60% of SAH patients deal with recurring headaches that persist over time.
Possible Complications When Diagnosed with Acute Subarachnoid Hemorrhage
Cerebral vasospasm, a condition where the blood vessels in the brain suddenly narrow, usually occurs between the third and seventh day after its onset. This happens because the release of blood products from a subarachnoid hemorrhage (bleeding between the brain and its surrounding membrane) stimulates certain pathways in the body that lead to the contraction of the cerebral arteries.
If this occurs, the treatment includes the administration of intravenous fluids to achieve a state of high blood pressure, increased blood volume, and dilution of blood — a strategy often dubbed the ‘Triple H’ approach. However, the effectiveness of this treatment has not been widely studied and is not backed up by robust scientific evidence. If the vasospasm doesn’t improve with this method, an angiography (an X-ray procedure to examine blood vessels) might be attempted to identify the location of the spasms and deliver medication directly into the arteries, or to inflate a balloon inside the artery to help it open up.
Other complications associated with a subarachnoid hemorrhage include:
- Hydrocephalus (buildup of fluid in the brain)
- Hypopituitarism (diminished hormone secretion by the pituitary gland)
- Cardiac decompensation (heart failure)
- Changes in blood pressure and electrolyte levels
- Seizures
Research indicates that seizures occur in up to one-third of hospitalizations for subarachnoid hemorrhage. Although doctors often administer antiepileptic drugs to prevent seizures, there is no solid research to support the benefits of this practice. Some studies have suggested a worse outcome and an increased risk of stomach bleeding associated with these medications, but the reason for these findings remains unclear.
Preventing Acute Subarachnoid Hemorrhage
It’s crucial for individuals at risk of Subarachnoid Hemorrhage (SAH), a type of brain bleed, to recognize the symptoms. Many people who’ve had SAH often describe it as the “worst headache of their life.” Other signs requiring urgent medical attention can include:
- Sudden weakness or numbness in the face, arm, or leg, especially on just one side of the body
- Out of the blue confusion or problems with speech or understanding what others are saying
- Abrupt loss of coordination, difficulty walking or standing straight, or keeping balance
- A sudden, intense headache that comes out of nowhere
Following an SAH and immediate surgery, the stay in the Intensive Care Unit (ICU) can carry a substantial risk of further health complications and even life-threatening conditions. Patients should therefore manage their expectations based on certain indicators that predict worse outcomes. It’s essential for patients to learn about the best ways to monitor their blood flow and pressure.












