What is Epidural Hematoma?
An epidural hematoma (EDH) is a serious condition where blood builds up in the space between the tough outer layer of the tissue that protects the brain (dura mater) and the inside of the skull. This buildup is usually contained between the joints of the skull (especially the coronal sutures) where the dura mater attaches. It’s a dangerous situation that could potentially lead to severe illness or death if not treated in time. Quick identification and removal of the blood are key to recovery.
What Causes Epidural Hematoma?
Around 10% of people who need to be hospitalized due to a traumatic brain injury (an injury to the brain often caused by a violent blow or jolt to the head) end up having an epidural hematoma. An epidural hematoma is a collection of blood that forms between the outer layer of the brain and the skull, which can be caused by both traumatic and non-traumatic reasons.
Most of the time, epidural hematomas happen because of head injuries from car accidents, assaults, or accidental falls.
But they can also occur for non-trauma related reasons, like:
- Infections or abscesses (pus-filled pockets in your body)
- Coagulopathy (a condition where the blood’s ability to clot is impaired)
- Bleeding tumors
- Vascular malformations (abnormalities in the blood vessels)
Risk Factors and Frequency for Epidural Hematoma
An epidural hematoma is a type of head injury that happens in 2% of all head injuries, and it can be fatal in up to 15% of the cases. It typically affects males more than females, and is more common among young people, specifically those aged 20 to 30. The occurrence of this injury is rare in people over the age of 50 to 60. As a person gets older, the dura mater, a layer covering the brain, becomes more tightly attached to the skull, reducing the chances of a hematoma, or a blood clot, forming in that space.
- An epidural hematoma is a head injury that happens in 2% of all head trauma cases.
- It can be fatal in up to 15% of these incidents.
- Males are usually affected more than females.
- The most affected age group is 20 to 30 years old.
- This injury is rare in people over 50 to 60 years old.
- Due to natural changes in the brain’s protective layers with age, the chances of getting this injury decrease.
Signs and Symptoms of Epidural Hematoma
An Epidural hematoma (EDH) is a medical condition often caused by trauma that can cause symptoms to vary significantly; from temporary loss of consciousness to a coma. A particular sequence of events happens in 14% to 21% of patients with EDH. This includes an initial loss of consciousness, a complete, but temporary, recovery (also sometimes referred to as ‘lucid interval’) and then a quick worsening of neurological conditions. Some individuals might not lose their consciousness initially or might regain consciousness after a brief coma. The lucid interval isn’t unique to just EDH as it might also occur in cases with other growing mass lesions.
Active bleeding observed through a CT scan is a characteristic sign when the lucid interval is present in clean EDH that is very large. The speed of an EDH’s development within the cranial vault, or skull, influences how rapidly the symptoms show. A smaller EDH may go unnoticed, showing no symptoms, though this is a rarity. Also, the development of an EDH could be delayed.
Around 5% of all post-traumatic intracranial mass lesions are caused by a rarer form of EDH known as posterior fossa EDH. Patients with this condition often remain conscious until the later stages when they may suddenly lose consciousness, stop breathing, and potentially die. Such a hematoma often reaches the compartment above the tentorium by stripping the dura over the transverse sinus, leading to severe intracranial bleeding.
The growing hematoma causes an increase in intracranial pressure, which can be identified clinically. Observations may include a dilated pupil on the same side as the hematoma (caused by herniation and oculomotor nerve compression), high blood pressure, slow heart rate, and irregular breathing. Known as the “Cushing reflex”, these signs may indicate an urgent need for intracranial intervention to prevent central nervous system depression and death.
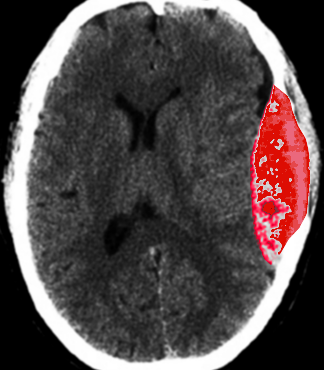
depicts an epidural hematoma post-trauma on computed tomography scan.
Testing for Epidural Hematoma
If you are suspected of having certain conditions, doctors use a particular type of imaging known as a CT scan (computed tomogram) to examine what’s happening inside your body. Also used to measure any potential bleeding risk or other blood-related disorders, doctors may assess your liver function or tests, which measure how long it takes your blood to clot. These tests include the INR (International Normalized Ratio), PTT (Partial Thromboplastin Time), and PT (Prothrombin Time).
CT scans are commonly used to identify bleeding inside the skull due to their wide availability in emergency departments. In many cases, if there is bleeding in the brain, it can show up on a CT scan. This bleeding might look like a lens-shaped mass, because the blood can’t spread beyond certain points within the skull. However, these bleedings do not cross the lines where the bones of the skull meet, called sutures.
Radiologists (doctors who specialize in imaging) often use a formula to estimate the amount of blood present if there’s bleeding. This formula takes into consideration the size of the bleeding on the CT slice where it appears the most, measures it from different angles, and checks how many slices present the bleeding.
Other features on CT scans help doctors understand more about the bleeding. For example, areas of fading or “swirl-sign” could indicate continuous leaking of the blood, and might signal the need for surgery. Sometimes, if the bleed is touching bruised brain tissues, it may appear flatter or less prominent on the scan, which if not carefully checked, might be overlooked.
There are times when a CT scan might not reflect what truly is happening inside the brain. Certain conditions like severe anemia, hypotension, or if the scan was done too quickly after the trauma, can lead to imprecise interpretation. Also, if the bleeding is caused by a weakened vein, the progress of blood accumulation might take longer and could complicate the interpretation of the CT scan.
Magnetic Resonance Imaging (MRI) is an alternative to CT scans. MRI of the brain is better at detecting bleeding especially at the top part, or vertex, of the head. Doctors usually recommend an MRI if a CT scan did not show anything, even though the clinical symptoms suggest the possibility of bleeding inside the brain or skull. When it comes to suspected spinal bleeding, an MRI is typically the better option because it offers a more detailed image compared to a spinal CT scan.
In certain cases, especially if the bleeding is near the top of the head (the vertex), doctors might need to check for a condition called a dural arteriovenous (AV) fistula. It’s a connection that may develop between an artery and a vein in the dura, the tough layer that covers the brain. This condition usually emerges from the middle meningeal artery, an artery that runs through the side of the head. To fully examine this, doctors may use angiography, a procedure that uses X-rays and a special dye to see the blood vessels.
Treatment Options for Epidural Hematoma
Extradural hematoma (EDH) is a serious condition that often requires immediate surgery to prevent severe brain damage or death. This condition happens when blood accumulates between the outer layer of the brain and the skull due to a head injury. Quick consultation with a brain surgeon (neurosurgeon) is essential because it’s critical to act within 1 to 2 hours after symptoms begin.
The first step is to stabilize the patient, ensuring they can breathe and have a good blood flow (referred to as the basics: airway, breathing, circulation).
Surgery is generally recommended for people with:
* Acute (new and severe) EDH
* A hematoma, or blood clot, volume greater than 30 ml irrespective of their level of consciousness (Glasgow Coma Scale score)
* A Glasgow Coma Scale score of less than 9, with eye-related abnormalities like unequal pupil size
In patients with acute and symptomatic (causing noticeable symptoms) EDH, the typical treatment is an operation called a craniotomy, where a part of the skull is temporarily removed to allow access to the brain, followed by removal of the blood clot. If the necessary surgical expertise is unavailable, another slightly less invasive method called “trephination” (or burr hole evacuation), where a small hole is drilled into the skull, may be used to help decrease the risk of death. However, a craniotomy can provide a more thorough removal of the blood clot, if it can be done.
There’s a lack of research comparing non-surgical (conservative) management with surgery in patients with EDH. However, in some cases, a non-surgical approach might be considered. These cases might include patients with acute EDH who have mild symptoms and meet all the following criteria:
* EDH volume of less than 30 ml
* Blood clot diameter of less than 15 mm
* A shift of the brain structures to one side (midline shift) of less than 5 mm
* A Glasgow Coma Scale score greater than 8, and without any specific neurological symptoms in the physical examination.
If it’s decided to manage the condition without surgery, it’s important for these patients to be monitored closely with regular brain scans and neurological exams due to the risk of the clot expanding and leading to a worsening of the patient’s condition. A follow-up brain scan is usually recommended 6 to 8 hours after the brain injury.
What else can Epidural Hematoma be?
Here are some potential causes that are considered if someone is experiencing certain neurological symptoms:
- Intracranial abscess (an infection in the brain)
- Intracranial mass (a tumor in the brain)
- Seizure
- Transient ischemic attack (a mini-stroke)
What to expect with Epidural Hematoma
Generally, patients with pure EDHs (Extradural Hematomas – blood accumulations between the outer layer of the brain and the skull) have a high likelihood of returning to normal function after surgery if diagnosed and treated quickly. Delay in diagnosis and treatment can lead to increased health risks and a higher chance of death.
EDHs caused by artery bleeding happen quickly and can be noticed early. However, ones due to tears in the dural sinus – a group of blood channels found at the back of the head – can take longer to show signs, which can cause a delay in both diagnosis and treatment. If an EDH measures greater than 50 cm before surgery, it usually results in worse brain function and higher mortality risk.
The following factors can influence the outcome of the condition and the prognosis after the removal of the EDHs:
- Age of the patient
- The time between the injury and treatment
- Whether the patient was in a coma or conscious during the interval right after the injury
- Abnormalities in pupil reaction to light
- GCS/motor score (the Glasgow Coma Scale is a tool to assess the severity of brain injury) upon arrival
- Findings from the CT scan, such as the volume of the hematoma, the degree of alignment shift of the brain, whether there’s active bleeding in the hematoma or any associated brain injuries
- The pressure inside the skull after the surgery
Meanwhile, the factors that might indicate a poor prognosis in EDH cases comprise a low GCS before or upon the surgery, problems in pupil reaction, being of an older age, delay between neurological symptoms and surgery, and an elevated pressure inside the skull after the operation.
A head CT scan can show specific signs that may suggest a worse outlook, such as a hematoma that’s larger than 30 to 150 ml, a shift in the alignment of the brain greater than 10 to 12 mm, a “swirl sign” indicating active bleeding, and associated brain injuries like contusions (bruises), brain bleeding, bleeding into the space surrounding the brain, and widespread brain swelling.
Possible Complications When Diagnosed with Epidural Hematoma
If the bleeding is substantial, it can cause pressure on the brain which is referred to as a mass effect. Another potential consequence is herniation, which is when the brain tissue, blood or cerebral spinal fluid is moved away from its normal position in the skull. Seizures are also a possible complication.
Common Side Effects:
- Mass effect: Pressure on the brain due to significant bleeding
- Herniation: Movement of brain tissue, blood, or cerebral spinal fluid away from its normal location
- Seizures