What is Papilledema?
Papilledema is a medical condition where the optic disc, the spot at the back of the eye where the optic nerve enters, swells up because of increased pressure inside the skull, or intracranial pressure. This is different from disc edema, which is a more general term for any kind of swelling of the optic disc due to various causes. It’s important to note that sometimes the pressure inside the skull can rise without causing swelling of the optic disc. Papilledema can affect both eyes, but it sometimes affects the eyes unevenly or only one eye. It can be a warning sign for medical conditions that cause increased pressure inside the skull, like brain tumors, inflammation of the brain and spinal cord from infections or non-infectious causes, and a condition called idiopathic intracranial hypertension (IIH), where the pressure inside the skull increases without a clear cause.
What Causes Papilledema?
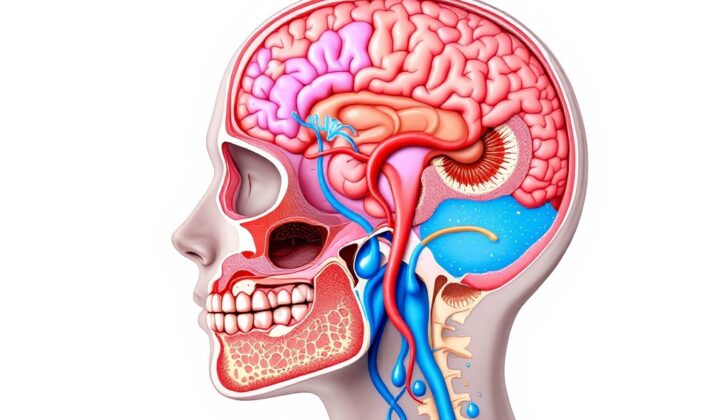
Papilledema happens when there’s an increase in the pressure inside the skull (intracranial pressure or ICP). According to the Monro-Kellie theory, this pressure depends on the total volume of different components in the skull – like blood, brain tissue, and cerebrospinal fluid (the fluid around the brain and spinal cord).
Because the skull has fixed space, if the amount of any of these components increases, something else must decrease in volume to maintain balance. This change can cause symptoms like headache and reduced blood flow to the brain. If the body can’t adequately balance these volumes, the intracranial pressure might increase.
Many situations might lead to an increase in ICP. Some of these include growth in the skull like a tumor or bleeding, an increase in cerebrospinal fluid as seen in conditions like obstructive hydrocephalus, increased blood volume as seen in conditions like venous sinus thrombosis, or sometimes the specific cause could not be determined, a condition known as idiopathic intracranial hypertension.
Risk Factors and Frequency for Papilledema
Papilledema, or swelling of the optic nerve in the eye, occurs with different frequencies depending on where it’s being recorded. One thing we do know is that it’s often associated with a condition called idiopathic intracranial hypertension, especially in an eye care professional’s clinic. Here’s how it breaks down:
- In the general population of the United States, about 0.9 out of every 100,000 people experience this condition each year.
- Obese women who are of child-bearing age (20 to 44) have a higher incidence, with 13 out of every 100,000 experiencing it.
- This issue doesn’t seem to favor any particular race.
- Person’s who are men, children, or elderly tend to experience it much less often.
Signs and Symptoms of Papilledema
If someone has an increased pressure inside their skull, also known as elevated intracranial pressure (ICP), it’s important for doctors to thoroughly record their visual complaints and the root cause of the increased pressure. They might experience vision loss, temporary darkening of vision, double vision, or hear a pulsating sound in their ears. Headaches are a common symptom and can worsen when the person is in positions that increase blood flow to the head. They may also experience nausea and vomiting when the pressure rises suddenly. It’s important for the patient to mention any medicines they’re taking such as steroids, retinoids, tetracyclines, or oral contraceptives since these can contribute to the increase in pressure. Conditions like weight gain and obesity should be checked as these are risk factors for idiopathic intracranial hypertension, a condition where the pressure inside the skull increases for no identifiable reason.
An eye and nervous system exam should also be done, focusing on the optic disc, which is the spot where the optic nerve enters the back of the eye. Lack of pulsations at the optic disc could indicate that the pressure inside the skull is higher than the pressure inside the eye. The exam may reveal certain changes like an elevated optic disc, widened veins, bleeding on top of the optic disc, an overly blood-filled optic disc, and certain types of retinal folds. The borders of the disc may appear blurred and doctors use a widely accepted grading system suggested by the ophthalmologist Lars Friesen to assess the changes:
- Grade 1: Disturbance of the normal arrangement of nerve fiber bundles with blurring on the nasal side of the optic disc and normal temporal side
- Grade 2: Blurring of the disc on both nasal and temporal (surrounding) sides with more prominent changes from grade 1
- Grade 3: The elevated and blurred edges of the disc cover one or more major segments of the retinal vessels
- Grade 4: Changes are more pronounced than in grade 3, with total obscuration of a segment of the central retinal artery or vein
- Grade 5: Changes are more pronounced than in grade 4, and all the vessels of the disc are completely obscured
Testing for Papilledema
When doctors suspect that you have papilledema, which is swelling of the optic disc at the back of each eye, they try to figure out what’s causing it. This investigation often starts with two kinds of scans: a contrast-enhanced magnetic resonance imaging (MRI) of your brain and eye sockets, and a magnetic resonance venography. The MRI helps to search for any abnormal growth like a tumor, and the venography checks for any blood clot in the veins of your brain.
After the scans, if your doctor thinks it’s safe, you may need a lumbar puncture, commonly known as a spinal tap. This procedure measures the pressure of the fluid that surrounds your brain and spinal cord to check if it’s too high. The pressure is considered normal if it’s less than 25 cm H20 while you’re lying on your side.
Besides pressure, the fluid, called cerebrospinal fluid, will also be tested to check the levels of protein and sugar, the number and types of cells, and whether there are any bacteria or other microbes; these results can give more clues to your diagnosis.
Your doctor will also closely check your vision. You may need a test called perimetry to map your field of vision and monitor any loss over time. In addition, tests like fluorescein angiography and B-scan ultrasound can help identify other causes of swelling or conditions that can mimic papilledema. Fluorescein angiography uses a special dye and camera to examine the blood circulation in your eye, while B-scan ultrasound uses sound waves to create an image of the eye.
Treatment Options for Papilledema
Papilledema is a condition where the optic nerve in your eye gets swollen due to high pressure in your brain. The treatment aims at resolving this elevated brain pressure.
This pressure can rise due to a growth or ‘mass’ present in the brain in which case, a surgical procedure might be necessary to remove it. Also, a blood clot in the brain’s veins, known as venous sinus thrombosis, could also cause this pressure to rise. Here, doctors will investigate what caused the clot and may recommend blood-thinning medication to prevent more from forming.
In cases where the brain pressure is high, but no specific cause can be found, the condition is called idiopathic intracranial hypertension (IIH). This can be managed with weight loss and medication like acetazolamide, which helps decrease the amount of fluid (or cerebrospinal fluid – CSF) your body makes, thus reducing the pressure.
In extreme cases, if the vision is under severe threat, a surgical procedure called optic nerve sheath fenestration might be carried out to relieve the pressure on the optic nerve.
There are other surgeries like ventriculoperitoneal and lumboperitoneal shunting that help manage this condition. These procedures involve placing a flexible tube to divert the flow of CSF from your brain or spine into your abdomen, thereby reducing the pressure.
In people with IIH who also have a narrowed vein in the brain (transverse venous sinus stenosis), a procedure called venous sinus stenting might be considered. This involves inserting a tube into the vein to keep it open and allow the normal flow of blood.
What else can Papilledema be?
When a doctor sees swelling of the optic nerve (also known as optic disc edema), they need to rule out other potential causes. These could be:
- Inflammation inside the eye
- Blockage of the central retinal vein
- Pressure on the optic nerve
- Inflammation of the optic nerve (optic neuritis)
- Changes to the optic nerve caused by diabetes (diabetic papillopathy)
- Problems with blood flow to the optic nerve (ischemic optic neuropathy)
There’s also a condition called pseudopapilledema. In this case, the optic nerve appears to be swollen, but it’s actually just a normal variation. This could be due to a birth defect, a buildup of deposits in the optic nerve (optic disc drusen), or an optic disc that is tilted.
What to expect with Papilledema
The outlook for papilledema, or swelling of the optic nerve at the back of the eye, depends on how long the condition has been present. Persistent high pressure inside the head can lead to permanent loss of the nerve layer in the back of the eye. This often leads to a slow decline in the field of vision and a reduction in the sharpness of central vision.
Possible Complications When Diagnosed with Papilledema
Problems can develop if raised ICP, or Intra-cranial pressure, is not correctly treated. This can be due to either a misdiagnosis of high ICP, or because a surgical procedure has not been successful. For example, if an operation on the sheath around the optic nerve does not work, there could be scarring afterward. Additionally, shunts that help to drain cerebrospinal fluid (or CSF) can fail if they malfunction, become obstructed, or blocked. Any kind of surgery, especially those involving the cerebrospinal space, carries a risk of severe infection.
Common Issues:
- Untreated or incorrectly diagnosed high ICP
- Unsuccessful surgeries
- Scarring after optic nerve operations
- Malfunctioning CSF shunts
- Obstruction or blockage of CSF shunts
- Severe infections after surgery particularly involving the cerebrospinal space