What is Sciatica?
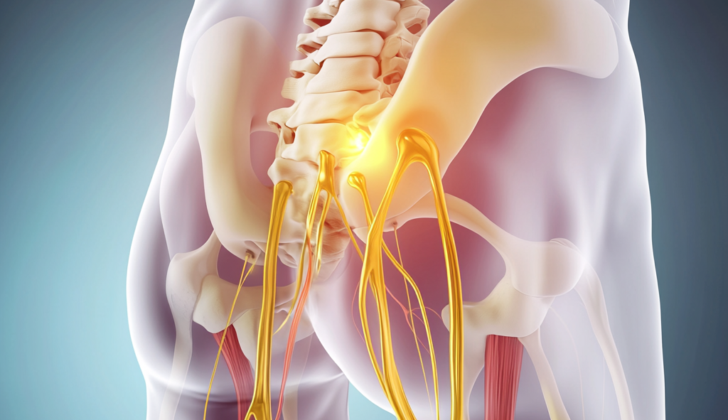
Sciatica is a painful condition that is caused by pressure or damage to the sciatic nerve or an associated nerve in the lower back and spinal area. It’s a common misunderstanding to label any low back pain or shooting leg pain as sciatica. However, sciatica refers specifically to pain that comes directly from issues with the sciatic nerve or its root nerves. This nerve is quite large, with a diameter of up to 2 cm, and includes nerve roots from the lower lumbar area to the lower sacrum area. Movements such as bending, twisting your back, or coughing can make the pain worse.
The sciatic nerve is very important as it controls the hamstring muscles and the muscles that pull the legs together. It also indirectly controls the muscles of the calf, front of the lower leg, and some foot muscles. In addition to controlling these muscles, its ends help with feeling in the back and side of the lower leg and the sole of the foot. Sciatica most often comes from an inflammatory condition that irritates the sciatic nerve. On the other hand, direct pressure on the nerve can cause more noticeable muscle problems, and if this happens, a detailed and speedy diagnosis is needed.
What Causes Sciatica?
Sciatica is a condition that arises when the sciatic nerve, which runs down your lower back to your feet, is pinched or irritated. This can happen due to various structural issues. The most frequent cause of sciatica is a herniated or bulging disc in the lower spine. In simpler terms, think of this as a cushion between your spinal bones slipping out of place, which, in turn, pinches the sciatic nerve.
In older people, a condition called lumbar spinal stenosis can lead to sciatica. This means that the spaces within the spine in the lower back become narrow, putting pressure on the nerves.
Another condition called spondylolisthesis, which is a misalignment of the vertebrae or spinal bones, can also cause these symptoms.
Additionally, muscle spasms or inflammation in the lower back or pelvic area can squeeze a nerve root in the lower back or sacrum, which subsequently might lead to sciatica.
A mass or lump located near the spine, including serious conditions like cancer, a blood clot (epidural hematoma), or a pocket of infection (epidural abscess), can also squeeze the nerve and bring about sciatica symptoms.
Risk Factors and Frequency for Sciatica
Sciatica, a condition affecting the sciatic nerve, has some unique characteristics in terms of who it affects and when. It doesn’t favor any particular gender and tends to be most common in people in their 40s. It’s also likely to affect between 10% to 40% of people at some point in their lives, with 1% to 5% of people developing it each year.
Interestingly, body height doesn’t seem to be a factor unless a person is between 50 and 60 years old. It’s also not common in people under 20, unless it’s caused by an injury. There are some evidence suggesting that genetics may play a role. In terms of lifestyle factors, certain types of physical activity can either increase or decrease the risk, depending on whether a person has had sciatic symptoms before. And there are certain jobs – like machine operators, truck drivers, and those requiring physically awkward positions – that may increase the likelihood of developing Sciatica.
- Sciatica doesn’t favor any particular gender.
- The majority of cases appear in people in their 40s.
- About 10% to 40% of people will experience it in their lifetime.
- It affects 1% to 5% of the population annually.
- Body height doesn’t usually play a role, except for people aged 50 to 60.
- It’s rare in people under 20 unless it’s due to an injury.
- There is some evidence suggesting a genetic link.
- Physical activity can increase or decrease the risk, depending on previous sciatic symptoms.
- Certain occupations, including machine operators and truck drivers or jobs requiring awkward positioning, may increase the risk.
Signs and Symptoms of Sciatica
Sciatica is a condition where pain is experienced along the path of the sciatic nerve. It often begins in the lower back and radiates down the affected leg. Some people describe it as a burning sensation with accompanying deep pain in the buttocks. Occasionally, a person may say that the affected leg feels “heavy”, which might indicate some level of weakness.
A common test for sciatica is the straight-leg raise. This test is performed while the patient is lying on their back. The doctor will raise the patient’s leg, keeping it straight at the knee. The test is most likely pointing to a herniated lumbar Disc if pain is felt between 30° and 70° of the hip being flexed and is predominantly in the back. If pain and an abnormal sensation is felt in the leg, it can be an indication that a peripheral nerve is being compressed. If pain is reproduced above 70° of flexion or below 30°, the cause is generally thought to be musculoskeletal and not related to herniation.
There are variants on the straight-leg raise test that can help to clarify the diagnosis. One adapted version is the crossed straight leg test. In this version, the test is conducted on the leg that doesn’t have symptoms. If pain is reported in the leg with symptoms while the other leg is raised to a 40° angle, it could indicate a central disc herniation with severe nerve irritation. There are also other signs that are specific to the nerve root being affected, such as certain types of weakness or altered reflexes that correspond to the area of the body supplied by that particular nerve.
- L3 radiculopathy: Features weakness of hip adduction, knee extension, and sensory pain in the front and inside of the thigh.
- L4 radiculopathy: Presents with ankle dorsiflexion weakness and an absent patellar reflex.
- L5 radiculopathy: Is indicated by hip abduction and big toe extension weakness.
- S1 nerve root compression: Is characterized by absent ankle reflexes.
Testing for Sciatica
Sciatica is diagnosed primarily by understanding your medical history and conducting a comprehensive physical examination. At the beginning, imaging tests like X-rays or scans usually aren’t necessary. However, if there’s a concern about a spinal fracture or a condition called spondylolisthesis (slipping of a vertebra), your doctor may ask for plain films of the lumbosacral spine, the lower part of your back. If these films don’t show anything, a non-contrast CT scan (a type of X-ray that shows detailed images of your body) may be used to check for a fracture.
If your pain lasts for 6 to 8 weeks despite treatment, imaging tests might be needed to figure out what’s going on. In these situations, magnetic resonance imaging (MRI) is typically the preferred method. MRI uses a powerful magnetic field and radio waves to create detailed images of your body. It can help locate the source of the pain and determine if there’s a pressing need for surgery.
An MRI will also be done right away if neurological symptoms like numbness, weakness, or tingling in your legs are present, or if there’s suspicion of a ‘mass effect,’ meaning something is pressing on your nerves or spinal cord. Remember, an MRI is the gold standard in determining the exact cause of the pain and making sure surgical treatment is not urgently needed.
Treatment Options for Sciatica
Here are some helpful tips to manage pain caused by sciatica:
Self-care recommendations:
- Use heat pads or ice packs to comfort the area and reduce swelling.
- Avoid activities that worsen your pain or sitting or standing for prolonged periods.
- Maintain a straight, upright posture.
- Do exercises that make your core muscles stronger.
- Gently stretch your lower back and the back of your thighs.
- Regularly engage in light exercises like walking, swimming, or water-based therapies.
- Always use the correct lifting techniques to prevent further injury.
Medical treatments:
- Short-term use of oral nonsteroidal anti-inflammatory drugs, known as NSAIDs these may help alleviate pain.
- Opioid and non-opioid painkillers may also be recommended.
- Muscle relaxants can provide relief.
- Anticonvulsants could be recommended for nerve-related pain.
- If NSAIDs aren’t enough, oral steroids may be beneficial.
- Local steroid injections may be offered.
- Spinal manipulation, a type of physical therapy, could be useful.
- Deep tissue massage may provide relief.
- Consulting with a physical therapist can provide additional exercises or treatments.
- Patients may need to be evaluated for surgery to correct any structural issues in the back such as disc herniation, epidural hematoma, epidural abscess, or tumor.
- Acupuncture, a traditional Chinese medicine practice, can also be a useful treatment.