What is Subfalcine Herniation?
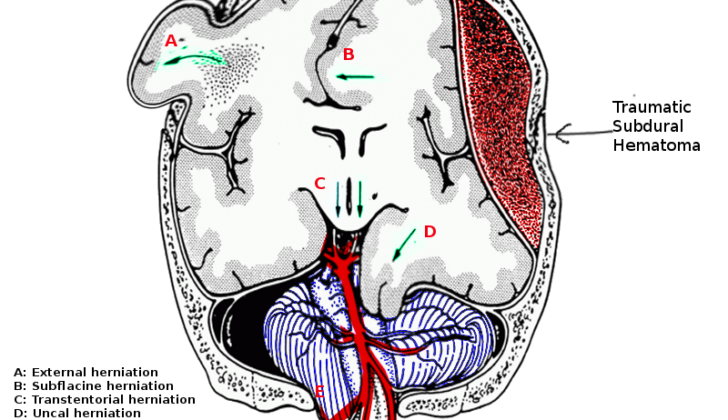
Herniation is when a part of the brain moves from its usual place to somewhere else within the skull. The most common type of this is called subfalcine herniation. In this case, a part of the brain, called the cingulate gyrus, is pushed under an area in the skull known as the falx cerebri. If the condition progresses, more parts of the frontal lobe of the brain may be affected.
In infants, once the spaces in their skull (called fontanels) close up, their skull becomes a closed, inflexible structure. The skull then holds the brain, a fluid called cerebrospinal fluid (or CSF), and blood. There’s a principle known as the Monroe-Kellie doctrine which states that the total volume inside the skull remains constant. So, if the volume of one of these components increases, the others must decrease. This shift can have serious consequences, like reducing blood flow to the brain or causing a herniation of brain tissue. The symptoms and outcomes of herniation are determined by where in the brain the herniation occurs.
What Causes Subfalcine Herniation?
Subfalcine herniation is a condition that can happen in the brain due to other primary injuries. This means that part of your brain moves out of its normal position due to changes in volume in the brain’s compartments. Here’s a list of things that might be associated with subfalcine herniation:
1. Increased brain volume: This can happen due to a traumatic brain injury, different types of brain bleeding, a stroke, a tumor, or swelling in the brain. Certain medical conditions like seizures, low sodium level, diabetic ketoacidosis or diabetes insipidus, and high levels of ammonia can also result in brain swelling.
2. Changes in cerebrospinal fluid (CSF) volume: CSF is a clear, colorless body fluid found in your brain and spinal cord. Its volume can increase due to a tumor in the brain, blockage of the fluid’s normal flow paths (obstructive hydrocephalus), overproduction of fluid in the brain (non-obstructive hydrocephalus), a non-cancerous growth in the brain (pseudotumor cerebri), or inflammation of the brain coverings or growths.
3. Changes in intracranial blood volume: The amount of blood present inside your skull can increase due to injury, increase in blood flow to the brain because of high carbon-dioxide or low oxygen, clotting in brain’s vein, high pressure in the right upper chamber of heart, or increase in acid levels in the blood. It can also decrease quickly due to removal of a clot in the brain.
It’s important to note that these events themselves can be severe and require immediate medical attention.
Risk Factors and Frequency for Subfalcine Herniation
Subfalcine herniation is often mentioned as the most common type of brain herniation, although not everyone agrees with this. This is mainly due to the fact that precise details about how often it happens aren’t easily available. This is probably because the symptoms can sometimes be too minor to require brain imaging, or the patient’s condition worsened very quickly. When this happens, the brain imaging might not show a subfalcine herniation but rather more serious forms of brain herniation.
Despite this, it is generally assumed that the number of cases of subfalcine herniation is reflected in the incidents of conditions known to cause it, as well as ischemic events that might result from it. The leading causes of subfalcine herniation are traumatic brain injuries (TBI), brain tumors, and strokes.
- According to the Centers for Disease Control (CDC), TBI is a major cause of death and disability in the United States for all races, ethnic groups, socioeconomic levels, and ages.
- Between 2002 and 2006, about 1.7 million US civilians experienced a TBI each year.
- Of these, nearly 1.4 million were treated and released from emergency departments, 275,000 were hospitalized and discharged alive, while 52,000 died.
- TBI-related deaths account for about one-third of deaths caused by injuries.
This data doesn’t include US military personnel who suffered a TBI while overseas, or people who didn’t seek medical help. An estimated 25% of patients who sustain TBI do not seek medical care. Therefore, it is likely that the real number of cases is higher than the recorded number. The same could also be true for the incidence of subfalcine herniation.
According to reports from the CDC, children under five years old are most likely to experience TBI, as shown by emergency department visits, hospital visits, and TBI-induced deaths. The next most affected group are adolescents aged 15 to 19, followed by adults aged 75 or older. Among these three age groups, older adults experience the highest rates of TBI hospitalizations and deaths.
- The frequency of ischemic strokes in infants, children, and adults younger than 45 ranges from 0.62 to 7.9 per 100,000 children per year and 3.4 to 11.3 per 100,000 adults per year.
- These rates mostly apply to white populations. For young black adults, the incidence of ischemic stroke can go as high as 22.8 per 100,000 people per year.
If we accept that the number of TBI cases and ischemic strokes represents the number of subfalcine herniations, then medical personnel treating patients with these conditions should keep a close eye on the potential for subfalcine herniation.
Signs and Symptoms of Subfalcine Herniation
A subfalcine herniation is a medical condition where the brain’s cingulate gyrus gets pushed under the falx cerebri, which is a membrane in between the brain’s halves. This condition could start with seemingly harmless symptoms such as headaches, nausea, vomiting, or changes in mental state. In some instances, subfalcine herniation can lead to contralateral (opposite side) leg weakness, as it can compress the artery that supplies blood to that part of the brain. If the affected area happens to be the speech center of the brain (the contralateral arcuate fasciculus), the patient may have difficulty with conducting, understanding or expressing speech.
If the primary lesion (damaged area) gets significantly large, it could result in uncal or central herniation. This type of herniation prompts more noticeable symptoms, including:
- One pupil larger than the other (anisocoria)
- Decreased consciousness
- Changes in respiratory pattern
- Changes in muscle tension
- Abnormal positions held by muscles (motor posturing)
- The combination of high blood pressure, slow heart rate, and irregular breathing (known as Cushing’s triad), which indicates a possible impending tonsillar herniation.
Testing for Subfalcine Herniation
If you notice any signs or symptoms that suggest things might be getting worse for your brain or nervous system, you should see a doctor straight away. They will listen to your story, ask about your symptoms, and do a physical exam. These will allow them to check if there’s a possibility of issues inside your brain causing these symptoms.
A head CT scan, or ‘CAT’ scan, is the first choice for imaging if there’s been traumatic brain injury. This is like a special kind of x-ray that gives a detailed image of your brain.
However, if the doctor thinks a brain tumor might be the cause, they might suggest a magnetic resonance imaging (MRI) scan, which gives an even more detailed picture – and can show up things that might be mistaken for tumors. This type of scan uses magnetic fields and radio waves, and is often done with and without a special dye, or contrast, to show different tissues more clearly.
If you have symptoms that suggest your brain might be suffering, you’ll be checked regularly to see if things are getting worse. If there are worrying signs that suggest pressure is building up in the brain (a condition known as intracranial herniation), the doctor will order a CT scan straight away. This type of scan is very good at picking up bleeding in the brain or subtle changes in its structure. It’s available in most hospitals and can be done quickly, which can make a big difference to how well you do.
An MRI does provide more detail, but you can’t always get one when you need it, and they do take longer than CT scans. While CT scans remain the first choice for quickly checking out the brain, there are other ways of checking for pressure in the brain. These include non-invasive intracranial pressure monitoring and transcranial Doppler ultrasonography. These techniques can be used at your bedside and do not carry the risks of radiation exposure.
Treatment Options for Subfalcine Herniation
If you’ve been diagnosed with a herniation syndrome, this means that a part of your body (in this case, usually part of the brain) has moved out of its normal position and is pressing onto another area. The goal of treating such conditions usually concentrates on supporting your breathing and circulatory systems, as well as trying to reduce the pressure inside your skull.
If you show signs of herniation, doctors will follow an emergency response plan called an Emergency Neurological Life Support (ENLS) management protocol. This involves various different levels of intervention, and if one level doesn’t seem to help, your doctor will move onto the next level in the protocol. While this is happening, your doctor will also try to identify and treat the underlying cause of the herniation. Nerve-based treatments often require a lot of patience and it’s important to see changes over time. Even if the initial steps don’t work, there are other more involved treatments like creating a small hole to drain excess fluid, removing anything putting pressure on the brain (like bleeding, tumors or infections), or performing a type of surgery called decompressive craniectomy.
Let’s talk a bit about how a herniation syndrome might be managed:
For basic medical management:
* The head of the bed might be raised more than 30 degrees to help decrease pressure.
* Some medications can be prescribed. To avoid confusion, we won’t go into detail about each type, but these include steroid therapy (only in some cases), several types of therapy involving specialized solutions, sedation, cooling the body, a specific type of powerful sedation, short-term heavy breathing, and preventative methods for controlling seizures.
About surgical management:
* There might be monitoring of intracranial pressure, which is the pressure inside your skull.
* A procedure called an external ventricular drain could be performed. This helps both to measure intracranial pressure and to rid the brain of excess fluid.
* A craniotomy might be performed to remove a blood clot or a mass in the brain.
* Finally, a surgery called a decompressive craniectomy might be performed, where part of the skull is removed to lessen pressure on the brain.
Overall, the management of herniation syndromes will depend on the specific situation, but always aims to protect the patient’s vital life functions while reducing intracranial pressure.
What else can Subfalcine Herniation be?
Subfalcine herniation doesn’t have other conditions that it can be mistaken for. However, it’s important to identify the main issue causing the herniation. If there hasn’t been any trauma, doctors would need to consider and rule out the following possible causes:
- Tumor
- Stroke
- Infection
- Edema
- Radiation necrosis
- Hydrocephalus (a condition where fluid builds up in the brain)
What to expect with Subfalcine Herniation
The outlook for patients with a brain herniation depends on several factors such as what caused the herniation, how much the pressure inside the head has increased, how long there’s been a reduction in blood supply to the brain, and which brain regions are affected. While some people fully recover, several others experience short-term and long-term brain-related struggles and disabilities. Studies point out that mortality rates can reach up to 33% in children that have serious head injuries not caused by a penetrating object and up to 60% in patients with a type of brain herniation called transtentorial herniation.
It’s been reported that 17% of patients with traumatic brain injuries have poor outcomes with moderate to severe disability or lasting coma. However, the good news is that the overall rates of illness and death from traumatic brain injuries have decreased in recent years. According to a 2017 surveillance report from the US Centers for Disease Control and Prevention, 73% of patients discharged after suffering a traumatic brain injury had a good level of functional recovery.
Possible Complications When Diagnosed with Subfalcine Herniation
The main issue with subfalcine herniation is that it can block blood flow through a major brain artery called the anterior cerebral artery. This blockage can trigger decreased blood supply, leading to damage in the frontal and parietal areas of the brain. As a result, the condition can progressively worsen, leading to decreased awareness, weakness on one side of the body, breathing difficulties as well as falling into a coma and death. Seizures could occur due to the regions of the brain where there isn’t enough oxygen or blood flow.
Common Effects:
- Blockage of blood in the brain
- Damage in the frontal and parietal regions of the brain
- Decreased awareness
- Weakness on one side of the body (hemiparesis)
- Breathing difficulties
- Coma
- Potential death
- Seizures
Preventing Subfalcine Herniation
When a part of the brain, called brain herniation, moves out of its normal position, it can cause serious health problems or even death. However, in some instances where the herniation occurs in a specific part of the brain known as the subfalcine, the patient might still be alert and able to make decisions. There’s potential for this condition to be reversed if it is treated quickly and correctly.
It’s crucial that the patient’s family and other loved ones are fully informed about what brain herniation is, what options are available for treatment, and how those treatments might help to improve the patient’s condition. This information is important because it allows the family to have a voice in making decisions about the patient’s treatment. The sooner this condition is diagnosed and treatment is started, the better the chances are for the patient to recover and have a good health outcome.