What is Tonsillar Herniation?
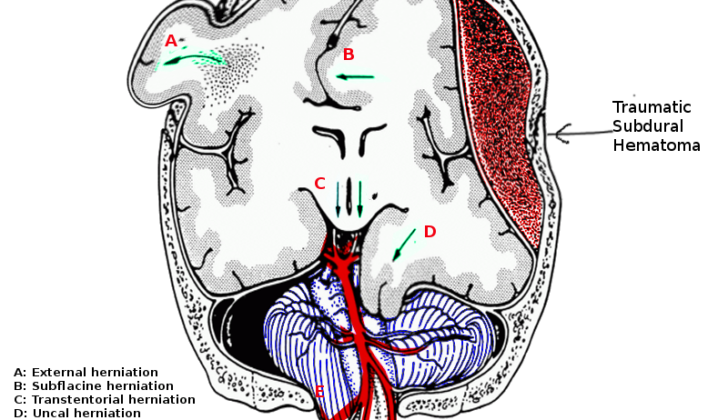
Brain herniation, which refers to the shifting of brain tissue from one area within the skull to another, is a serious condition. Your skull is divided into three main compartments by two firm sheet-like structures known as the falx cerebri and the tentorium. The falx cerebri sits between the two halves of your brain, while the tentorium divides the upper and lower areas of the skull. This lower area is also referred to as the posterior fossa which contains the cerebellum and brainstem, two critical parts of the brain. This compartment has two openings: the foramen magnum and the tentorial notch. The foramen magnum allows passage to the spinal canal, while the tentorial notch enables communication between the upper and lower compartments of the skull.
One particular type of brain herniation is tonsillar herniation, this happens when parts of the cerebellum, known as the cerebellar tonsils, push down through the foramen magnum. This causes pressure on the medulla, a part of the brainstem, leading it to flatten against the clivus/odontoid process (structures at the base of the skull). This descent of brain tissue can be pictured as “coning,” where the tissue is squeezed into a narrow space, much like ice cream being pushed into a cone. As this condition worsens, it can lead to a dangerous reaction known as Cushing’s reflex, which can ultimately result in death if not treated promptly.
What Causes Tonsillar Herniation?
Tonsillar herniation, a potentially serious brain condition, can occur if there is increased pressure inside the skull (also known as increased intracranial pressure or ICP). A variety of brain disorders can lead to this increase in pressure, particularly those that affect the region at the back of the skull, known as the posterior fossa.
These conditions include different types of bleeding in the brain, such as:
- bleeding within the brain tissue itself, particularly in the cerebellum, which controls balance,
- bleeding between the brain and the protective layers that cover it, known as subdural or extradural hematomas, and
- bleeding inside the fluid-filled spaces in the brain, called intraventricular hematomas.
Another condition is subarachnoid hemorrhage, which is bleeding around the brain. There are also tumors or abscesses (areas filled with pus) that take up space in the posterior fossa. Another cause can be hydrocephalus, a buildup of fluid inside the brain.
Brain swelling can also cause increased ICP, such as in diffuse axonal injury (a severe head injury causing damage throughout the brain), and in a condition called malignant middle cerebral artery stroke syndrome.
Finally, removing too much cerebral spinal fluid (CSF), which surrounds the brain and spinal cord, by a procedure called a lumbar puncture can also increase intracranial pressure.
Historically, lumbar puncture, where a large volume of CSF was removed, was a common cause of tonsillar herniation. The drop in spinal canal pressure could create a pressure difference, pushing brain tissue through the foramen magnum, a hole at the base of the skull. However, nowadays, before a lumbar puncture is carried out, a CT scan or MRI is performed if a patient has symptoms of raised ICP, such as headache, nausea, altered consciousness, or specific neurological issues. This imaging helps doctors determine if it is safe to proceed with the lumbar puncture.
Risk Factors and Frequency for Tonsillar Herniation
Tonsillar herniation, a reaction to different health issues, doesn’t have a documented rate of occurrence. The main cause is usually a traumatic brain injury (TBI), but it can also occur due to intracerebral hemorrhage and subarachnoid hemorrhage. Around the world, an estimated 69 million people suffer from TBI each year.
Signs and Symptoms of Tonsillar Herniation
When someone has increased pressure inside their skull, known as raised intracranial pressure, and pressure on the lower part of the brain, known as brainstem compression, they could be in a comatose state. During a physical examination, the individual might present abnormal body positions like decortication or decerebration. In more severe or late cases, they could have flaccid paralysis. Additionally, their pupils might show unusual sizes or reactions depending on the specific cause of the condition. For instance, pressure on the midbrain could result in pupils that are medium-sized and do not respond to light, while a condition like a pontine hemorrhage could cause the pupils to become tiny and unresponsive. Furthermore, if the pressure started due to a lesion above a part of the brain known as the tentorium, the person might have unequal pupils as a result of pressure on their oculomotor nerve.
Another way to understand the progression of increased intracranial pressure is through the four stages outlined by the physician Harvey Cushing:
- Compensation – The pressure inside the skull rises, but there are no noticeable changes in physical or mental state
- Early manifestations – Symptoms like headaches and irritability begin to emerge
- Maximum manifestation – Symptoms become severe, and high blood pressure, slow heart rate, and slow breathing are observed
- Paralysis – Individuals fall into a deep coma, have low blood pressure and fast heart rate, and could potentially stop breathing before passing away
Testing for Tonsillar Herniation
If a patient has a traumatic brain injury (TBI), doctors will assess their neurological condition using a globally accepted measure called the Glasgow coma scale. However, this scale isn’t perfect and may sometimes misrepresent the nature of the injury. For example, a two-point drop in speech on this scale could signify damage to a specific brain area responsible for speech, rather than a general drop in consciousness.
Patients who have slipped into a coma will usually get a head CT scan (a type of advanced X-ray), unless the cause of their coma is known and reversible. If the patient’s consciousness is lowered and their pupils are unequal in size, it’s highly likely that they have a ‘surgical lesion,’ or area of injury that might be treatable with surgery. Such patients need urgent scans to confirm this.
Symptoms showing up on a head CT scan that might go along with a surgical lesion include a shift in the brain’s central line, disappearance of the areas in the brain called basal cisterns and ventricles, and effacement (or thinning) of the sulci (furrows on the brain’s surface) and ventricles. Doctors will then look for signs of herniation, or the protrusion of brain tissue into an area where it does not normally reside. A specific type of herniation called tonsillar herniation can be identified in specific CT scan views by its typical crowding and effacement features.
If the patient’s situation is acute, or severe, they might need an intracranial pressure (ICP) monitor placed. ICP monitors, which come in forms like a bolt or an intraventricular catheter, measure the pressure inside your skull. If there is herniation going on, the ICP is usually high (over 20 mm Hg) and the ICP monitor will show a loss in the brain’s ability to regulate pressure (compliance). ICP monitors produce a waveform with three main peaks. In a healthy individual, the first peak (related to the heartbeat) should be tallest, followed by the second (related to the brain’s capacity to regulate pressure) and third (related to the veins) peaks. However, if the second peak is tallest, it indicates loss of compliance. An added advantage of using an intraventricular catheter to monitor ICP is that it lets doctors lower high ICP levels by draining cerebrospinal fluid when needed.
Treatment Options for Tonsillar Herniation
A tonsillar herniation suggests that there’s an underlying issue that could be caused by a traumatic injury, bleeding, a tumor, or an excess of fluid on the brain (hydrocephalus). Treatment, therefore, focuses on addressing these root causes. Initially, with all patients who are unconscious, certain supportive procedures are put into place:
* The first priority is ensuring the patient can breathe properly, particularly if they have a low score on the Glasgow Coma Scale, which measures a patient’s level of consciousness.
* Providing enough oxygen is also critical to prevent low oxygen (hypoxia). The aim is to maintain oxygen saturation, a measure of the amount of oxygen getting to the tissues, above 90%.
* Adequate ventilation, or helping the patient breathe, is important as well. The goal is to maintain paCO2 – a measurement of carbon dioxide in the blood – at 35-40 mmHg, which is in the normal range. There might be times when a short period of hyperventilation, or increased breathing, might be needed to quickly lower paCO2. This causes the arteries in the brain to constrict, reducing the flow of blood to the brain and, in turn, lowering intracranial pressure (ICP), or pressure in the brain. This can be a temporary, life-saving technique for a patient showing signs of herniation – a dangerous condition where parts of the brain are pushed out of their usual positions. A patient’s paCO2 should not go below 25 mmHg, as this can decrease blood flow to the brain too much, causing damage.
* Balance of body fluids is also important. The aim is to keep mean arterial pressure (MAP) – the average pressure in a person’s arteries during one heartbeat – between 60 to 70 mm Hg. Low blood pressure can double the risk of death in traumatic brain injury. Osmotic therapy, where medications called osmotic diuretics are used to decrease pressure on the brain, is another temporary measure which can be applied when a patient shows acute signs of herniation. It works by lowering intracranial pressure, improving brain function, and increasing cerebral perfusion pressure (CPP), or the blood flow to the brain. Medications such as mannitol, or hypertonic 3% saline — solutions of salt dissolved in water — can be used. Normal body temperature, treatment for sepsis, and adequate nutrition are also started.
With regards to surgery, there are three guiding principles:
1. Removing the lesion, like a hematoma (a collection of blood) or a tumor, which is increasing the pressure on the brain.
2. Reducing intracranial pressure by draining cerebrospinal fluid (CSF), the fluid that surrounds the brain and spinal cord. This is usually achieved with an external ventricular drain, a tube placed in the brain to drain excess fluid.
3. Performing a decompressive craniectomy, a procedure where a part of the skull is removed to allow the brain to swell without being constricted. There is some evidence to suggest this can be helpful for patients with severely raised intracranial pressure and signs of herniation.
What else can Tonsillar Herniation be?
There are certain abnormal physical conditions present from birth, such as Chiari malformation, where the lower part of the brain descends into the spinal canal. These can be discovered unexpectedly during medical imaging. Although this condition can cause symptoms, it isn’t usually a sudden occurrence and won’t cause a swift compression of the brainstem area.
High blood pressure with a slow heart rate can also be triggered by a condition called autonomic dysreflexia. However, people with this condition are not rendered unconscious and their breathing remains normal.
An acute, or very sudden, spinal injury that affects the neck can also cause a slow heart rate, but it would typically also cause low blood pressure.
What to expect with Tonsillar Herniation
Tonsillar herniation is the final stage of a severe condition that happens inside the skull. Notably, according to Cushing, there are four stages of tonsillar herniation, and some research suggests that early surgical intervention could prevent death. One particular study focused on early detection of tonsillar herniation in patients with tumors in the back, lower part of their brain (posterior fossa). The study found that early surgical relief of pressure (decompression) could potentially prevent death.
Tonsillar herniation is usually a critical event and if not treated immediately, it greatly lowers the chances of recovery. If this condition starts impacting the patient’s ability to breathe, similar to what happens in a condition known as Cushing’s triad, there is virtually no chance of significant recovery.
Brain herniation after traumatic brain injuries (TBI) usually has a poor predicted outcome, and if there are signs of pressure on the brain stem, it is rarely reversible. In cases where patients are in a coma after gunshot wounds and show signs of damage to the brainstem, the mortality rate is a full 100%.
Possible Complications When Diagnosed with Tonsillar Herniation
Aside from potential brain related issues stemming from tonsillar herniation, like enduring brain damage, brain death, breathing failures, coma and death, there are other complications to consider. These correlate with severe sickness and include conditions linked to use of a ventilator, such as pneumonia, or consequences of bed rest like deep vein thrombosis and pulmonary embolus. Muscle weakness due to a grave illness, termed critical illness myopathy, could also be noted. Around 5% of patients suffering from traumatic brain injury could also face injuries to the visual system. Traumatic brain injury with fractures at the base of the skull may also lead to a late presentation of hypopituitarism, a condition where the pituitary gland at the base of the brain doesn’t produce sufficient hormones.
Complications may include:
- Enduring brain damage
- Brain death
- Breathing failures
- Coma
- Death
- Pneumonia linked to use of ventilator
- Deep vein thrombosis
- Pulmonary embolus
- Weak muscles (critical illness myopathy)
- Visual system injuries
- Hypopituitarism (linked with Traumatic brain injury with skull base fractures)
Preventing Tonsillar Herniation
Taking steps to minimize occurrences of road accidents, workplace mishaps and severe head injuries are crucial for public health. Such steps include mandatory practices such as always wearing seatbelts in cars and helmets while riding motorcycles and bicycles.
Brain complications, like tonsillar herniation (which refers to downward displacement of the brain due to pressure) and other related conditions, place a heavy physical, emotional, and financial load on the patient and their families. These conditions are costly to the healthcare system. This is mostly due to the fact that patients often need to spend a long time in the hospital followed by an extensive period of recovery and rehabilitation.