What is Caustic Ingestions?
When someone swallows a corrosive substance (caustic ingestion), it can damage the upper part of the digestive system, which consists of your mouth, throat, gullet (or esophagus), stomach, and the first part of your small intestine, often called the duodenum. This part of your digestive system starts from around the head and neck area and stretches down to the upper stomach area (epigastric area).
Let’s talk about these parts more. Firstly, the mouth, which includes parts like the inside area, the gums, teeth, tongue, and tonsils, is where we break down food by chewing and begin digestion. It’s surrounded by muscles that help to move the food. The next part is the pharynx, or what we usually call the throat. It’s divided into three parts: the nasopharynx, oropharynx, and laryngopharynx. These parts not only feel the food but also help in moving the chewed food from your mouth to your esophagus.
The esophagus is a lengthy muscular pipe that moves food from your mouth and throat down to your stomach. It goes through different parts of your body – your neck, your chest, and your belly. The esophagus has three narrowing points along its length which are the cervical constriction (at the top), the broncho-aortic constriction (in the middle), and the diaphragmatic constriction (at the bottom, opening into the stomach). These constrictions are useful markers during procedures looking inside the esophagus. The upper part of the esophagus has striated muscles (which make a striped pattern), the lower part has smooth muscles, and the middle contains both types of muscle. The esophagus is prone to spreading infections or cancers quickly to other parts due to its unique layered structure.
The stomach begins where the esophagus ends, at the esophagogastric junction. In this area, the lining of the digestive tract changes from a flat layered structure to a column-like structure. The stomach plays a vital role in further breaking down the food by using acid and protecting itself from this acid with mucus.
The duodenum, the first part of the small intestine, comes after the stomach and it neutralizes the stomach acid and breaks down food further. It can absorb nutrients because of its column-like lining and tiny finger-like projections.
When a corrosive substance is ingested, it can harm any part of the upper digestive system. The esophagus is most likely to be damaged by swallowing a base (alkali), while swallowing an acid is most likely to hurt the stomach. In severe cases, the damage can be so extensive that it creates holes in these organs and hurts parts nearby.
Swallowing harmful substances is a significant cause of disease and death among all ages. It is especially common in children, accounting for 80% of cases in the US. For the best chances of recovery, it is essential for different types of healthcare professionals to work together to manage these incidents.
What Causes Caustic Ingestions?
Caustic exposure, which is the contact with strong chemicals that can burn or corrode, can happen by accident or on purpose. It is most commonly accidental and often happens with young children who ingest substances while exploring their environment. These “exploratory ingestions” usually involve small amounts of household cleaners that contain low concentrations of chemicals like bleach or ammonia. However, purposeful exposures often result from attempts at self-harm, where large quantities of highly concentrated caustic chemicals are ingested.
The majority of these chemical exposures happen through oral ingestion (about 76% of cases), and usually happen at home (around 93% of cases). More than 80% of the cases are unintentional. The chemicals consumed are either extremely acidic or extremely alkaline, and the treatment differs based on the nature of the substance.
Risk Factors and Frequency for Caustic Ingestions
In 2019, the American Association of Poison Control Centers documented 180,000 instances of harmful substance exposure in the U.S. The majority of these cases involved children accidentally consuming household cleaning products. Some cases also occurred among adults who intentionally consumed these harmful substances. Lye, an alkaline substance, was the most commonly reported ingredient involved in these accidents.
Signs and Symptoms of Caustic Ingestions
People who have suffered a harmful, or caustic, injury may become unresponsive and lose vital signs such as breathing and pulse. When this happens, immediate life-saving measures are necessary, regardless of the cause of the medical crisis. The patient’s airway, breathing, and circulation need to be stabilized, and they should be monitored continuously. Once the patient is stable, a more detailed examination can begin.
When looking into potential cases of harmful substance ingestion, there are five key details that need to gathered, known as the “5 Ws”:
- Who: This includes the patient’s personal details like age and weight. Information about anyone who was with the patient, like family or friends, is also useful.
- What: The specifics of what substances were ingested.
- When: The time and date the substances were ingested.
- Where: How the poisoning occurred and where it happened.
- Why: Establishing whether the ingestion was intentional. This can influence the next steps for care, like a referral to a mental health professional.
The location of the incident may play a part in what happened and it’s important to note whether the ingestion was unintentional or not. If the ingestion wasn’t an accident, it’s possible that other substances like painkillers, drugs, or alcohol were also consumed.
Someone who has ingested a harmful substance might not show any signs at first or could become severely sick. They may report symptoms like vomiting, drooling, chest or stomach pain, and difficulty breathing or swallowing. Blood in the vomit is a possible side effect caused by injury to blood vessels.
A physical exam may reveal swelling of the mouth and tongue, and excessive drooling. Swelling in the upper airway might cause changes in the voice, noisy breathing or breathlessness. If the substance has caused a tear in the food pipe, it can lead to serious infections. These infections may show up as a faster heartbeat, fever, or a peculiar sound over the chest during examination. Tenderness and stiffness in the abdomen could indicate another kind of infection. A thorough exam should be conducted to look for other injuries, like burns in the mouth or around the eyes.
Testing for Caustic Ingestions
After a patient swallows a harmful substance, doctors will perform several tests. This includes a complete blood count, or CBC, which can reveal inflammation. Dehydration or vomiting blood might interfere with these results. Additionally, a comprehensive metabolic profile, or CMP, is used to identify problems with the body’s electrolyte balance, which can be thrown off by repeated vomiting. It also reveals how well the kidneys and liver are functioning, which is valuable if surgery might be needed. Using blood gases, doctors can assess the degree of lung damage.
If there’s reason to suspect a drug overdose as well, your doctor could order a comprehensive drug panel. This can detect many different substances all at once.
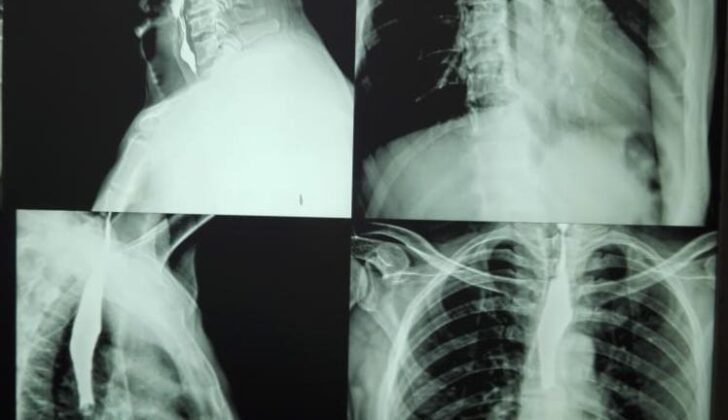
X-ray imaging can help identify areas that are trapping air as a result of injury, like the space in the middle of the chest (pneumomediastinum) or the space in the belly surrounding the organs (pneumoperitoneum). If a harmful substance was inhaled into the lungs, it might cause certain patterns on a chest x-ray. A type of x-ray known as an upper gastrointestinal series, where you swallow a special dye, could help to confirm damage to the esophagus, but this is not necessary if a special visual exam is available.
This visual exam, called an esophagogastroduodenoscopy, or EGD, is the most trusted method for examining injuries from swallowed substances. For instance, it can help doctors predict how likely someone is to develop scarring, or strictures, based on how severe the injury appears. But it’s not always clear who needs to get this procedure. Some experts say everyone who’s been exposed to a harmful substance should get one, while others think it’s only necessary in cases where the exposure was intentional or the symptoms are severe.
Using an EGD early on appears to be beneficial, but the decision to use it needs to be individualized. For some patients, surgery might be a more urgent priority. If an EGD isn’t done in the first 24 hours, though, it may become too risky, as the tissue can become too delicate to touch safely.
Other options include endoscopic ultrasound (EUS) and contrast-enhanced computed tomography (CECT). The usefulness of EUS is still being looked into, and so far it doesn’t seem to be better than EGD at predicting complications. CECT, on the other hand, is non-invasive and provides detailed views and requires less time than an EGD. However, while it’s good at finding structural damage, it’s less reliable at predicting the need for surgery or the chance of stricture formation, so it can’t fully replace EGD in this situation. Nevertheless, it can still be helpful as a supplementary test when managing swallowed substance injuries.
Treatment Options for Caustic Ingestions
If a person is showing signs that they might soon struggle to breathe, such as drooling, low levels of oxygen in the blood, or changes in their voice, their airway should be made safe. This might involve putting a tube down their throat to help them breathe, as studies have shown that about half of adults who swallow harmful substances need a tube to secure their airways.
For patients showing symptoms of shock, they should be given fluids through a needle inserted into a vein – this can be done quite quickly and can use larger needles if necessary. If their blood pressure is still not stabilising, it might be necessary to administer medications that constrict blood vessels to increase blood pressure.
In the past, it was thought that neutralising the pH or diluting the harmful substance with water or milk might help. But studies in animals have had mixed results and there isn’t enough data from humans to support this. Also, there can be difficulties in getting the acidity levels correct and this approach might lead to injuries caused by heat. Therefore, it is generally not a recommended treatment option.
Diluting the harmful substance with water or milk, initially thought to reduce injuries caused by alkalis, has shown only minimal effects and only in the very first minutes after ingestion. There’s minimal evidence to support this approach and it can potentially cause harm due to over-filling the stomach. This treatment is also not currently recommended.
In cases where the harmful substance ingested is zinc or mercuric chloride, it may be beneficial to give activated charcoal. These are heavy metals that can cause damage to the lining of the digestive tract and be absorbed, eventually causing damage to multiple organs. Activated charcoal can help to absorb these substances in the gut, prevent their return to the liver and speed up their removal from the body.
The role of medicines that reduce stomach acid, such as H2-blockers and proton pump inhibitors, is still unclear. One study suggests that omeprazole might help to improve the condition of the esophagus after 72 hours. However, inducing vomiting should not be used as a way to manage harmful ingestions.
Inserting a tube into the stomach (nasogastric or NG tube) to potentially maintain the patency of the esophagus and reduce the chances of narrowing due to scarring has mixed studies. Even though some studies show it might help, the blind insertion of this tube can cause harmful infections and perforation in the food pipe. Therefore, such a procedure is only safe if a doctor can see what they are doing, perhaps through an endoscope.
Besides dealing with the immediate injury, doctors need to manage long-term consequences of swallowing harmful substances. One major concern is the formation of a stricture, or narrowing, of the esophagus caused by scarring. There have been suggestions to use corticosteroids, drugs that can reduce inflammation and the formation of scar tissue. However, there’s conflicting evidence surrounding this, with some studies suggesting higher doses might only be beneficial with a certain grade of injury.
Doctors can treat these narrowings by gradually stretching the esophagus or using stents to keep it open, among other techniques. There are also other potential treatment options, including different medications, but more research is needed to confirm if they are effective and safe, hence they are currently not recommended in routine practice.
If the patient is showing signs of infection in the mediastinum (the area between the lungs) or peritoneum (the membrane that lines the abdomen), or their condition is unstable, immediate surgical advice is required. Those who swallowed a large quantity of the harmful substance and develop shock, coagulation problems, or acidosis might need more extensive surgical intervention. Surgery may also be considered for those with high-grade injuries identified by special scans or endoscopy.
The aim of emergency surgery is to remove all the dead tissue. The standard approach involves exploring the abdomen through an incision, also known as exploratory laparotomy. The area that needs to be removed depends on the extent of the damage – sometimes only small pieces need to be removed but if the damage is extensive in the pancreas and the first section of the small intestine, surgery to remove these organs might be necessary.
What else can Caustic Ingestions be?
When a person ingests a harmful substance, there are a few possible causes to consider:
- Injuries or trauma
- Birth defects
- Burns from other sources
- Consumption of multiple drugs at once
A detailed check-up can help figure out which of these situations is the actual cause.
What to expect with Caustic Ingestions
The future health of someone who has swallowed a harmful substance largely depends on how severe the initial injury was. The outlook is generally more positive for mild-to-moderate cases. On the other hand, those with serious injuries that require emergency surgery often face poorer outcomes. Grade 3 injuries are severe and require immediate surgery and extensive medical care afterwards. ‘Mediastinitis’, which is an inflammation of the chest cavity, usually accompanies severe injuries, also leading to a poor prognosis.
Patients and their families should be prepared for potential complications after surgery. People who survive serious harmful substance injuries often see a significant drop in their quality of life. When planning for surgery, medical teams must consider potential outcomes after the treatment.
Possible Complications When Diagnosed with Caustic Ingestions
Early problems following the swallowing of harmful substances (caustic ingestion) often involve inflammation of the area between the lungs (mediastinitis) and instability caused by bleeding. These serious issues will need urgent surgery. Meanwhile, the most common late issue from swallowing harmful substances is the narrowing of the gastrointestinal tract (stricture), with the esophagus, the tube that connects your mouth to your stomach, being the most frequently affected area. Widening the esophagus can often help ease this problem. But if this isn’t possible or doesn’t help, an operation might be required to remove the affected part of the esophagus and replace it or bypass it. Depending on how severe the narrowing is, tissue from the intestines or stomach may be used.
Preventing narrowing is a widely debated subject. Starting to eat orally early is thought to prevent the narrowing in patients with a minor injury. Placing a stent, a device used to keep body passageways open, has a limited success rate (less than 50%) and there is a high chance that the stent may move from its original position (up to 25%). So far, no drugs have been successful in preventing the narrowing of the gastrointestinal tract after swallowing harmful substances.
Common Problems:
- Inflammation of area between the lungs
- Bleeding instability
- Narrowing of the gastrointestinal tract
- Esophagus issues
- Needs for surgical bypass or replacement
Areas of Debate:
- Early oral feeding
- Stent placement success
- Effectiveness of drugs
Recovery from Caustic Ingestions
Patients undergoing surgery for removal of the esophagus, or for severe injuries resulting from swallowing harmful substances, will require intensive care. This could involve aid in breathing, support for their circulatory system, and providing nutrients through an injection or infusion because they may not be able to eat normally. Since these patients will have changes in their eating habits and needs for wound healing, nutritionists will likely be a necessary part of their care team. Mental health professionals will also have to keep an eye on the patients’ mental state, particularly in instances where the harmful substance was swallowed on purpose.
Preventing Caustic Ingestions
Preventing people, especially children, from accidentally swallowing harmful substances needs everyone in the community to pitch in, as this problem can put a lot of strain on society. It’s suggested that we have strong laws in place to control how these dangerous chemicals are packaged and make sure that children can’t easily get to them. Parents should also be reminded to keep these substances out of reach from children and to store them in containers that are clearly marked.
Most of the time, when adults swallow these substances, it’s done on purpose. So, it’s critical to make sure people have access to mental health services. It’s also crucial to have a system in place that offers support to those in society who need it, in order to reduce the chances of attempts to harm oneself.